Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The small intestine is the longest organ in the gastrointestinal (GI) tract. It is responsible for the absorption of nutrients, maintaining water and electrolyte balance, providing an immunologic barrier, and endocrine secretion.
During the fourth week of gestation, the flat embryonic endoderm folds and fuses in the midline to create the gut tube. The tube consists of the foregut, midgut, and hindgut. The midgut, which will give rise to the distal duodenum, jejunum, and ileum, is located in the middle of this tube and is open to the yolk sac. During development, the connection between the midgut and the yolk sac will close and become only a thin stalk known as the vitelline duct. A Meckel diverticulum is the persistent remnant of this structure. The endoderm will form the epithelial lining of the digestive tract, and the splanchnic mesoderm will give rise to the muscle, connective tissue, and peritoneal components of the gut wall.
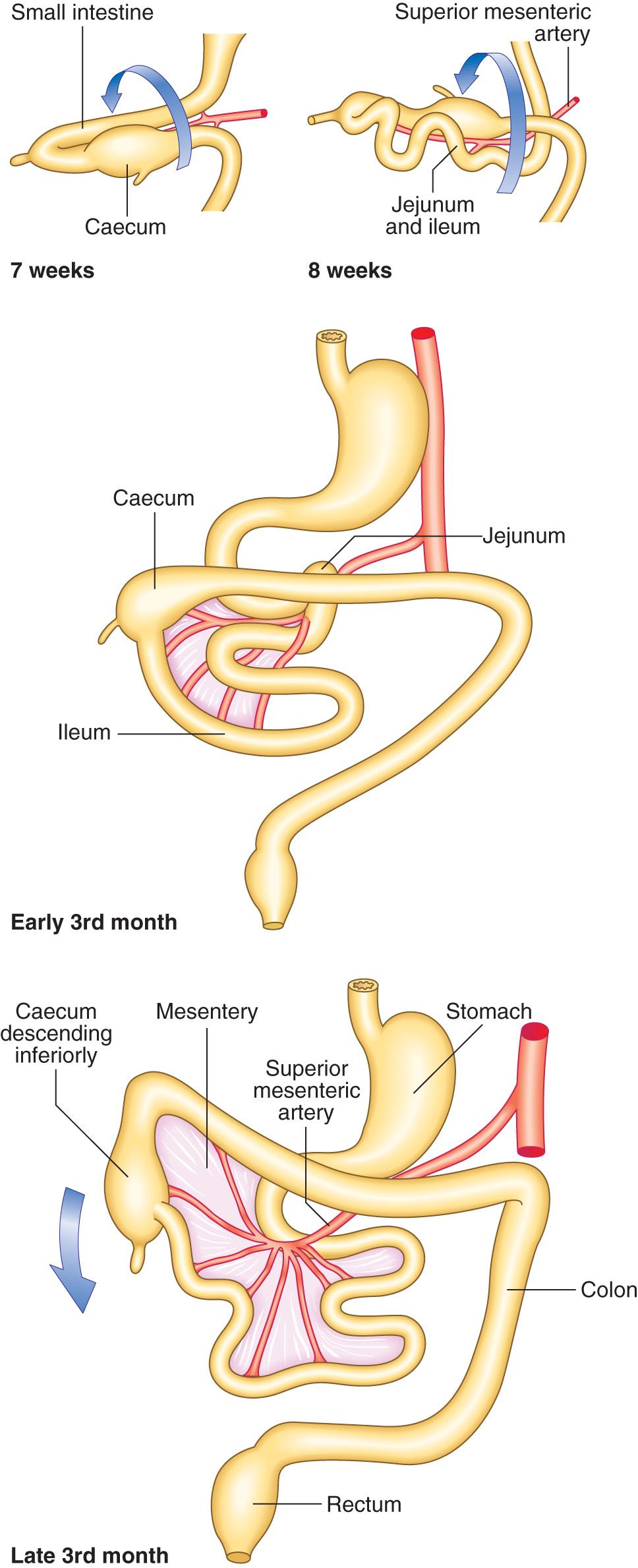
Throughout gestation, the small intestine will lengthen and rotate. By the fifth to seventh weeks, the midgut will have outgrown the capacity of the abdominal cavity, forcing it into a hairpin loop configuration and then herniating into the umbilical cord. As it herniates, the loop rotates 90 degrees counterclockwise. This rotation places the ileum in the left quadrant of the abdomen. Between the tenth and twelfth weeks, the midgut retracts back into the abdomen and will rotate an additional 180 degrees. By the end of the twelfth week, the midgut has rotated 270 degrees counterclockwise. The superior mesenteric artery is the axis of this rotation ( Fig. 71.1 ). The rotation of the intestines is important for establishing the permanent location of the abdominal organs. The proximal jejunum is positioned on the left side of the abdomen and the remaining loops of intestine will be displaced to the right. Errors in midgut rotation result in congenital malrotation. Omphalocele results from mistakes in the midgut returning to the abdominal cavity.
The location of the duodenum is affected by stomach rotation and pancreas development. As the stomach rotates during gestation, the duodenum will move to the right of the abdomen and up against the dorsal wall, and it will become retroperitoneal. The fusion of the ventral and dorsal pancreatic buds displaces the duodenum laterally creating the characteristic C-loop.
It is known that the gut develops along four different axes: (1) anterior-posterior, (2) dorsal-ventral, (3) left-right, and (4) radial. The development and differentiation of different regions of the gut are dependent on reciprocal interaction between the endoderm and the splanchnic mesoderm. In the initial stages of formation, the intestinal tract is lined by simple columnar endodermal epithelium that is surrounded by splanchnopleuric mesoderm. During the sixth week, the endodermal epithelium proliferates and occludes the lumen completely. Over the next 2 weeks, vacuoles will develop and coalesce to create a hollow tube. This process is known as recanalization. Duplication cysts and intestinal stenosis are the result of errors in recanalization. After this process is complete, the mucosal layer will develop villi as aggregates of mesoderm push through the epithelium. The submucosal connective tissue and smooth muscle layers arise from the mesodermal coating of the gut tube.
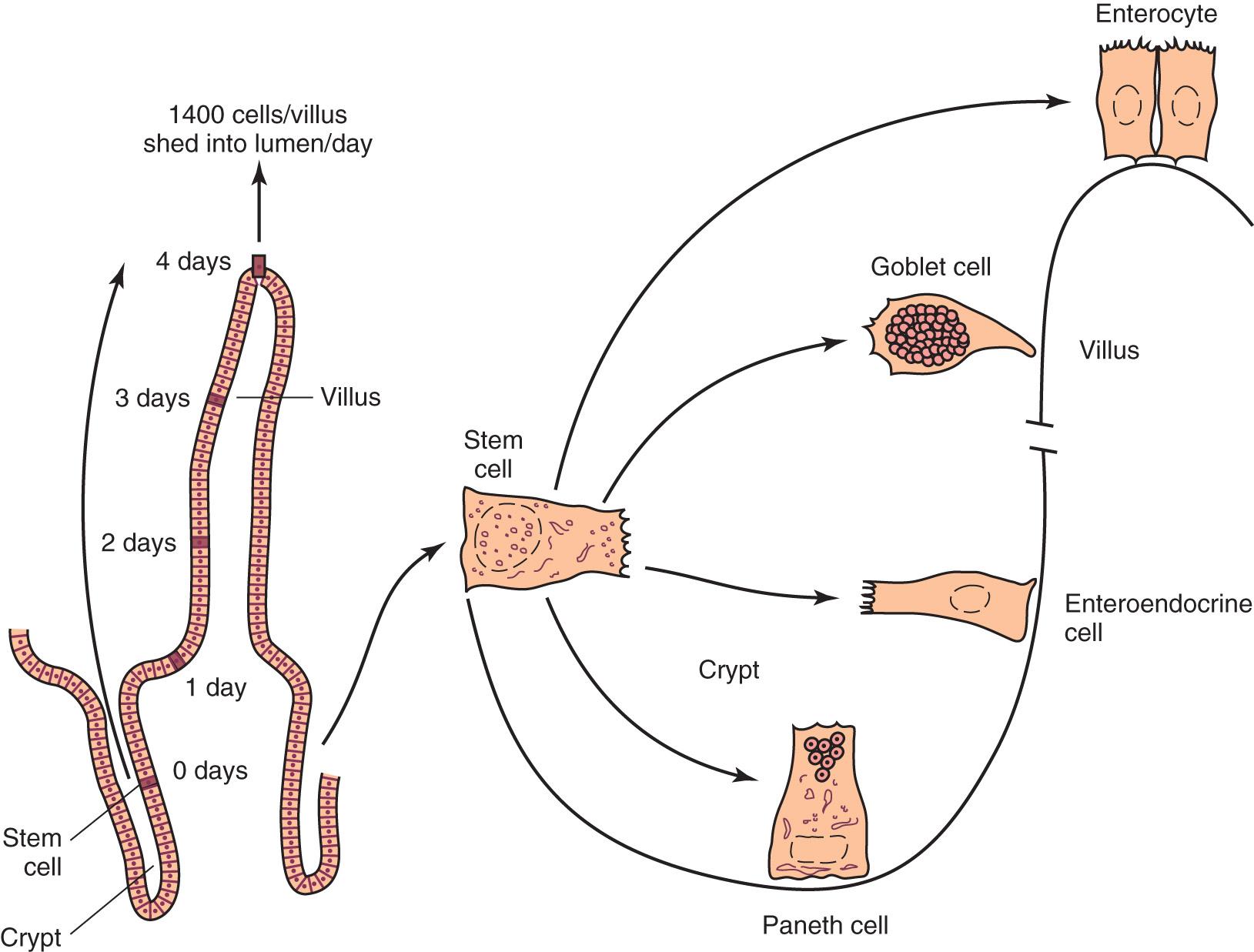
During the creation of the villi, pitlike intestinal crypts form at the base of the villi. Epithelial stem cells reside within the crypt and undergo a high rate of mitosis, which gives rise to the epithelial cells for the entire intestine. The epithelial cells within each crypt are of monoclonal origin. The stem cell divides into daughter cells, leaving one daughter cell anchored in the crypt, whereas the other continues to divide and migrate up the side of the crypt and onto the villus. This division and migration is responsible for renewing the intestinal lining in a rapid manner. While in utero, the stem cells will differentiate into one of the four major epithelial cell types: Paneth, enteroendocrine, goblet, or enterocyte (the function of each cell will be discussed in a later section) ( Fig. 71.2 ).
At 12 weeks of gestation, cell differentiation has begun but maturation will continue during the fetal period and through the first months of life. The cells will not develop digestive function until exposed to food. The first stool, meconium, is actually lanugo, a mixture of vernix caseosa from the skin, desquamated cells from the gut, and bile.
The small intestine is approximately 7 meters in length, starting at the pylorus and ending at the ileocecal valve (ICV). It is divided into three sections: the duodenum, jejunum, and ileum. The majority of the duodenum is located in the retroperitoneum, whereas the jejunum and ileum are intraperitoneal structures.
The lumen of the small intestine is a complex arrangement of structures that aid in nutrient absorption. Each structure is responsible for increasing the surface area of the intestine to enhance digestion and absorption of nutrients. The net result is a 600- to 1000-fold increase in surface area for a total of 250 to 400 m 2 . The epithelium of the small intestine is replaced every 3 to 6 days and can be influenced by a variety of factors. The rapid turnover and high mitotic rate of the cells makes the intestinal lining susceptible to the effects of radiation and chemotherapy.
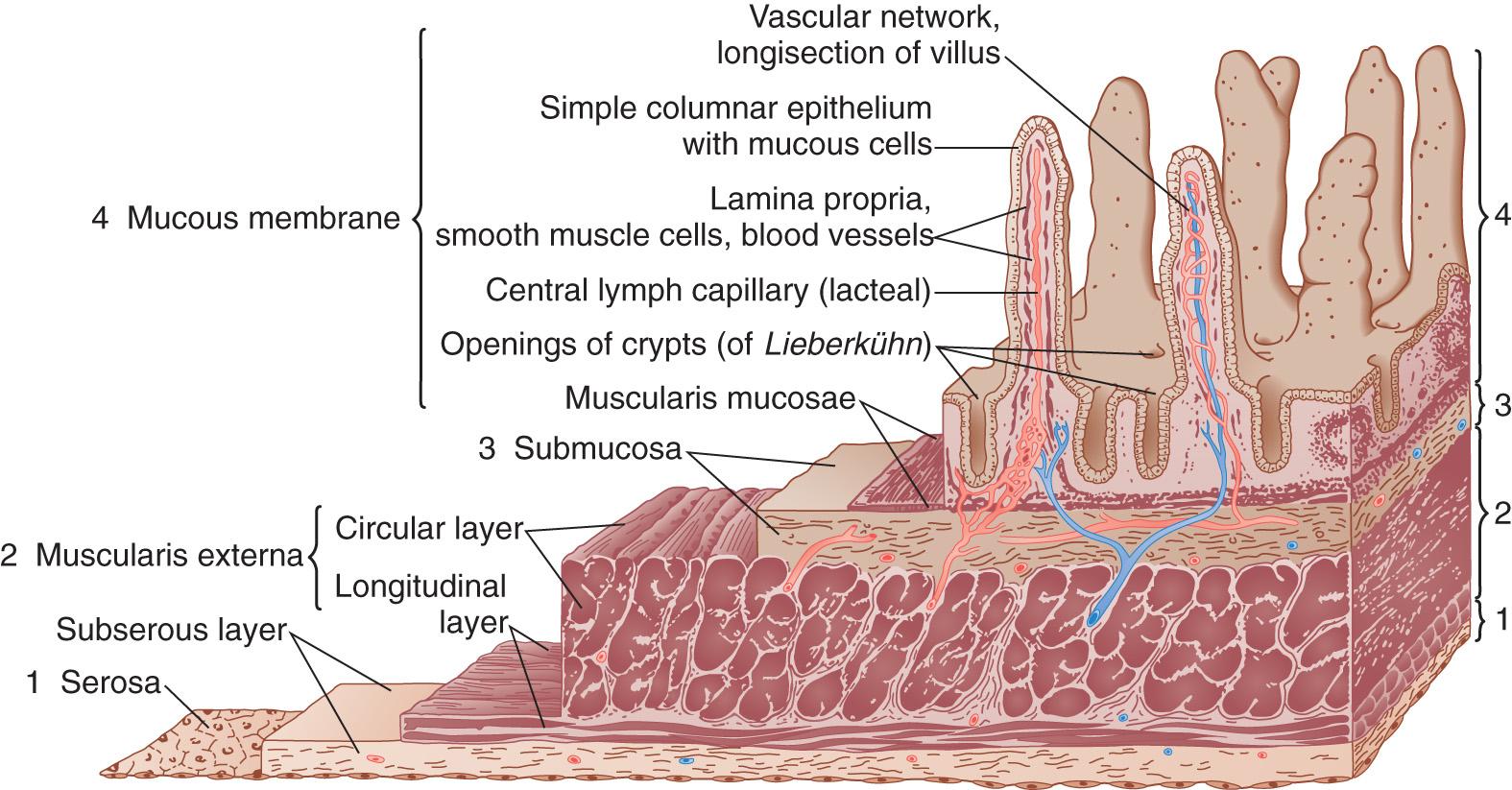
The wall of the small intestine is made up of four main layers: the mucosa, submucosa, muscularis propria, and serosa. The innermost layer is the mucosa. It is composed of three separate layers: epithelium, lamina propria, and muscularis mucosae. The mucosa is the site of absorption of nutrients and water from the intestinal lumen. The submucosa is the strength layer of the bowel wall and is composed of dense connective tissue. When completing a bowel anastomosis, it is important to incorporate suture through this layer of tissue to ensure integrity of the anastomosis. Blood vessels and lymphatics, including Peyer patches and Brunner glands, are found in this layer of the bowel wall. The Meissner, or submucosal plexus, is also located in the submucosa and is an integral component of the enteric nervous system (ENS). It is responsible for regulating bowel motility and secretion in the mucosal layer. The muscularis propria is composed of two smooth muscle layers, an outer longitudinal layer, and an inner circular layer. The myenteric, or Auerbach plexus, is situated between these two muscle layers and, like the Meissner plexus, helps control bowel motility and secretion. The serosa is the outermost layer of the bowel wall and is a single layer of mesothelial cells ( Fig. 71.3 ).
Plicae circulares are transverse folds of mucosa and submucosa that aid in absorption of nutrients by increasing the surface area of the small intestine threefold. These folds are deep and visible on gross inspection and on radiographic imaging, even when the small intestine is distended.
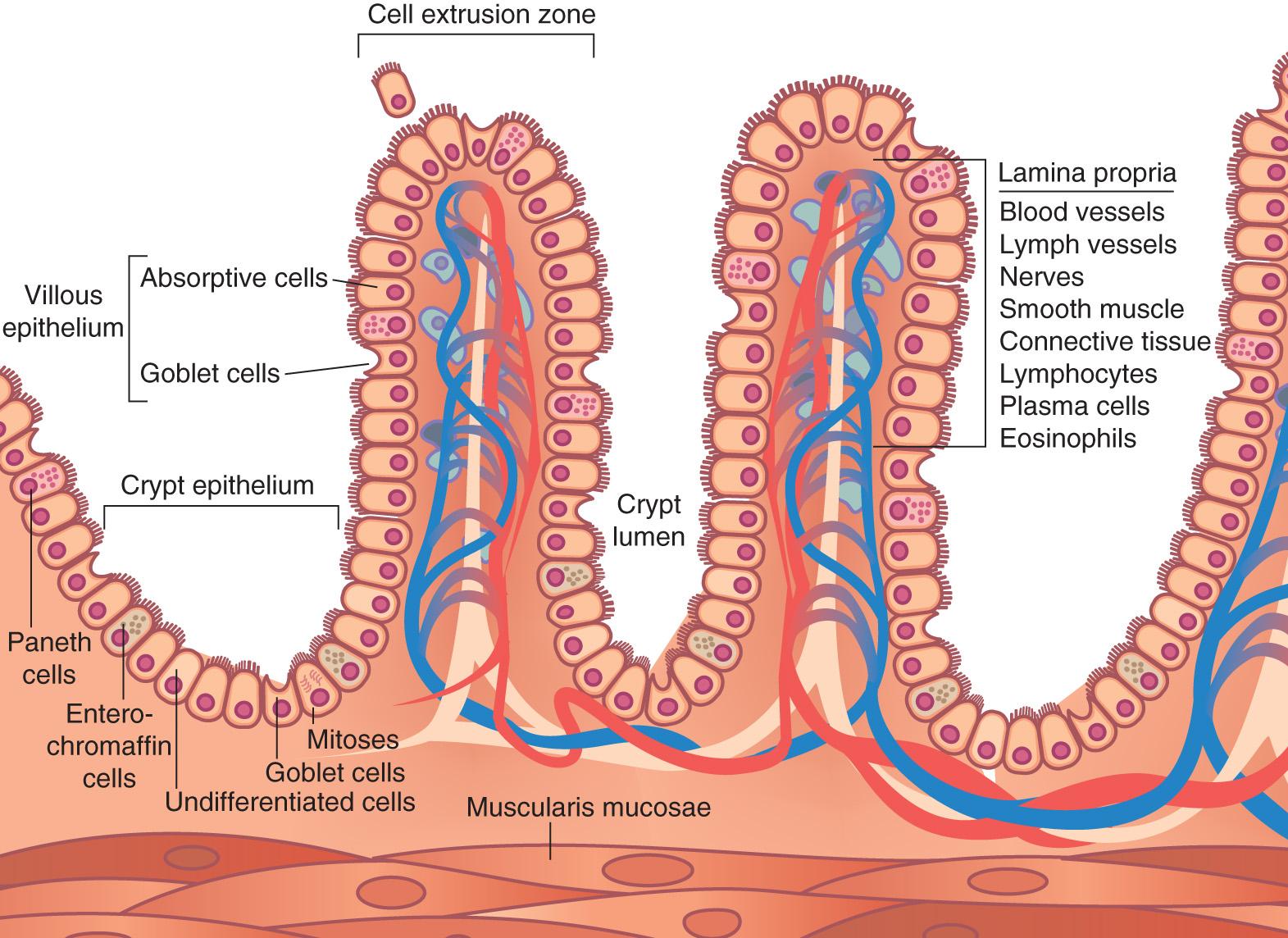
Villi are fingerlike projections of the mucosa that are present along the entire length of the small intestine. The villi are longest in the duodenum, where most of the digestion and absorption occurs, and shortest in the distal ileum. They increase the absorptive area 10-fold. The villus is coated with a single layer of columnar epithelial cells, called enterocytes. Between the enterocytes are goblet cells that secrete mucin. The mucin will lubricate and protect the intestinal wall as chyme and undigested food passes. Goblet cells become more prominent throughout the length of the small intestine.
At the base of each villus are 0.3- to 0.5-mm invaginations of intestinal mucosa called intestinal crypts or crypts of Lieberkühn. Crypt cells are responsible for mitosis and secretion of fluid and electrolytes. Each crypt is monoclonal and contains only one stem cell type. The stem cell divides into daughter cells, leaving one daughter cell anchored in the crypt, whereas the other continues to divide and migrate up the side of the crypt and onto the villus. On the villus, the daughter cell may differentiate into a goblet cell, an enterocyte, or an enteroendocrine cell. The enterocyte will continue to mature as it migrates toward the apical end of the villus and take on increased digestive and absorptive ability. Enteroendocrine cells produce hormones that modulate the digestive process by altering secretion and motility. Other cells may migrate to the bottom of the crypt to become Paneth cells. The purpose of the Paneth cell is discussed in detail in the immunology section.
Within each villus is a rich vascular supply from an arteriole and a venule that contribute to a network of capillaries. There is also a lacteal, a lymphatic capillary that runs the length of the villus. The lacteal can absorb larger particles containing lipids and lipid-soluble vitamins ( Fig. 71.4 ). These particles are known as chylomicrons, which are generated by neighbor enterocytes as they absorb and process lipid.
Microvilli are tiny projections of the plasma membrane that line the apical border of the enterocyte. The microvilli are coated with a thick glycocalyx that aids in nutrient absorption and serves as a protective barrier. In addition, many enzymes necessary for digestion and absorption, collectively referred to as the brush border enzymes , are released within this layer. These enzymes include nucleosidases, peptidases, and disaccharidases. Millions of microvilli make up the brush border and function to increase the surface area of the intestine another 20-fold.
Brunner glands are acinotubular glands found mostly in the proximal two-thirds of the duodenum. They secrete an alkaline mucus-like substance that protects the duodenum from the acidic chyme produced by the stomach. The substance also lubricates the intestine and provides an alkaline environment essential for the activation of enzymes important for digestion and absorption. Many protective factors have been identified within Brunner gland secretions including human epidermal growth factor (beta urogastrone), an inhibitor of gastric acid secretion. Lysozyme and pancreatic secretory trypsin inhibitor (PSTI) have been identified in these secretions as well.
Peyer patches are specialized aggregates of lymphoid follicles in the lamina propria. They are found along the antimesenteric border and are most abundant in the ileum. Peyer patches play an important role in mucosal immunity by recognizing and processing antigens. The germinal centers contain B lymphocytes, and T lymphocytes are in the interfollicular area. A specialized immune cell, the microfold cell or M cell, can be found in the epithelium overlying the lymphoid follicles. These cells are important in passive immunity by transporting antigens from the luminal surface to antigen-presenting cells into the lymphoid follicle.
The duodenum is the first section of the small intestine. It begins at the pylorus and ends at the ligament of Treitz and is approximately 25 cm in length. The duodenum is largely retroperitoneal and has an intimate anatomic relationship with the pancreas. It is divided into four sections: first (bulb), second (descending), third (transverse), and fourth (ascending).
The first section, or the bulb, begins at the pylorus, which is demarcated by the prepyloric vein, and is approximately 5 cm in length. The posterior wall of this portion of the duodenum is in direct contact with the gastroduodenal artery (GDA), common bile duct, and portal vein. The superior border of the first segment of the duodenum is attached to the porta hepatis by the hepatoduodenal ligament, which envelops the portal triad. This portion of the duodenum begins the C-loop around the head of the pancreas ( Fig. 71.5 ).
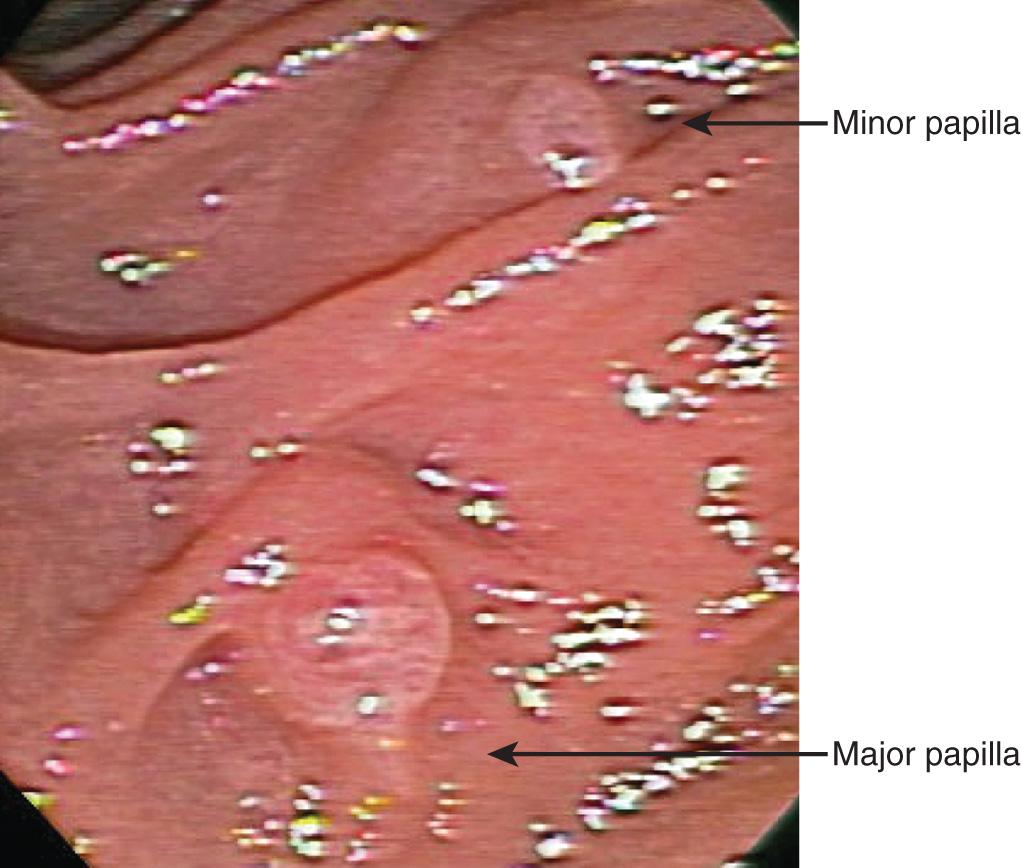
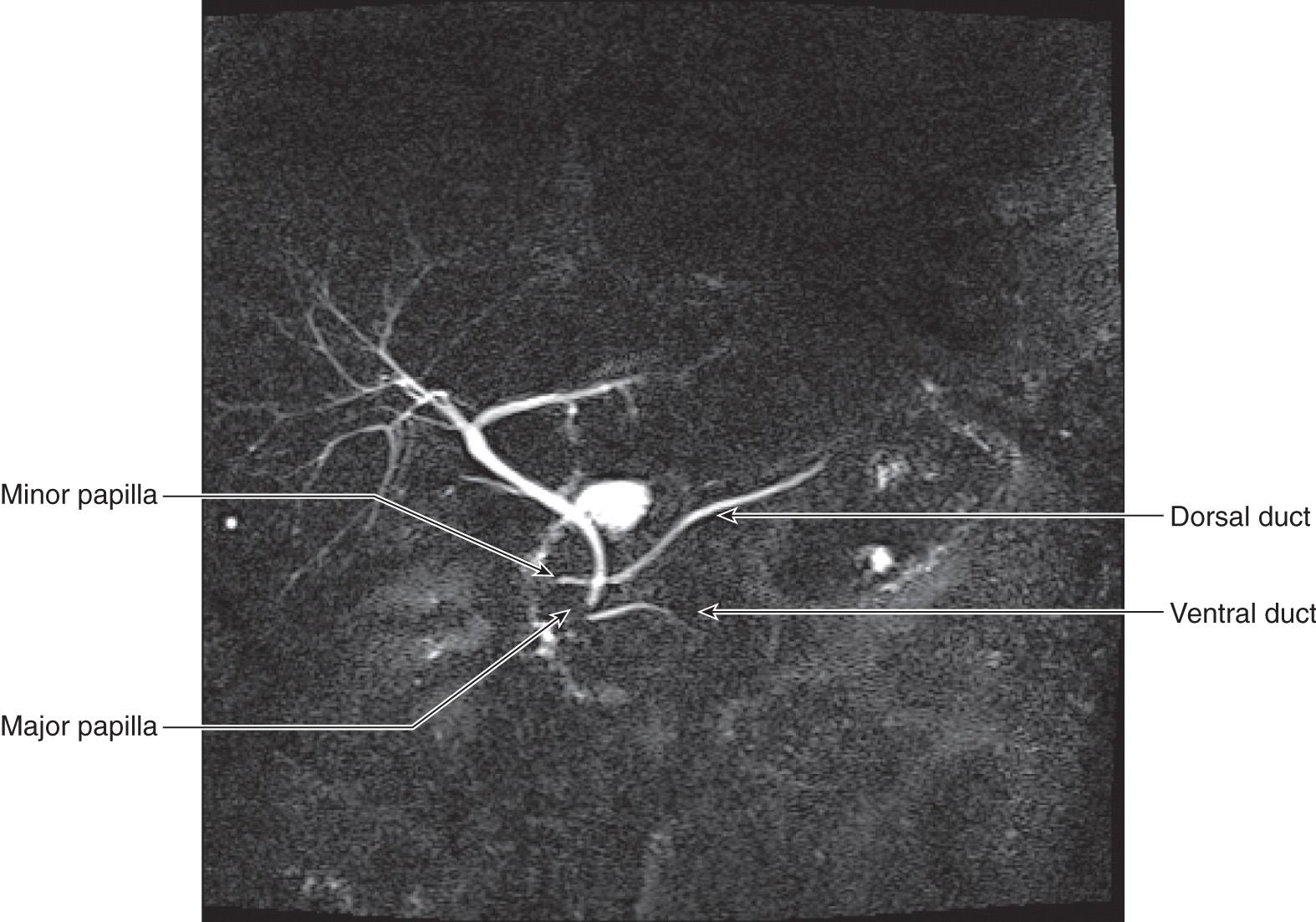
The second, descending, section is retroperitoneal and is approximately 10 cm in length. This segment is anterior to the right kidney and ureter and the lateral border of the inferior vena cava. The medial border is in direct contact with the head of the pancreas. Evaluation of the posterior surface of the descending duodenum, the posterior surface of the pancreatic head, and the common bile duct requires medial rotation of the descending duodenum using the Kocher maneuver. The main pancreatic duct, the duct of Wirsung, and the common bile duct join and empty into the posteromedial wall of the midportion of the descending duodenum. This opening is known as the ampulla of Vater. The minor pancreatic duct, the duct of Santorini, may also empty into the duodenum as the minor papilla ( Figs. 71.6 and 71.7 ).
The third, transverse, section is also retroperitoneal and is bordered by the uncinate process of the pancreas superiorly and the hepatic flexure of the colon anteriorly. The relationship of the duodenum to the colon is important during mobilization of the hepatic flexure during colon resection. Care must be taken to avoid injury to the duodenum. The superior mesenteric vessels run anterior to the transverse duodenum. The right ureter, right gonadal vessels, inferior vena cava, and aorta are posterior to the transverse duodenum.
The fourth portion of the duodenum courses in a cephalad direction to the left of the aorta and inferior to the neck of the pancreas. The end of the fourth portion is marked by the ligament of Treitz. The ligament serves as a point of fixation during intestinal rotation and runs from the right crus of the diaphragm and attaches to the intestinal wall at the duodenojejunal flexure.
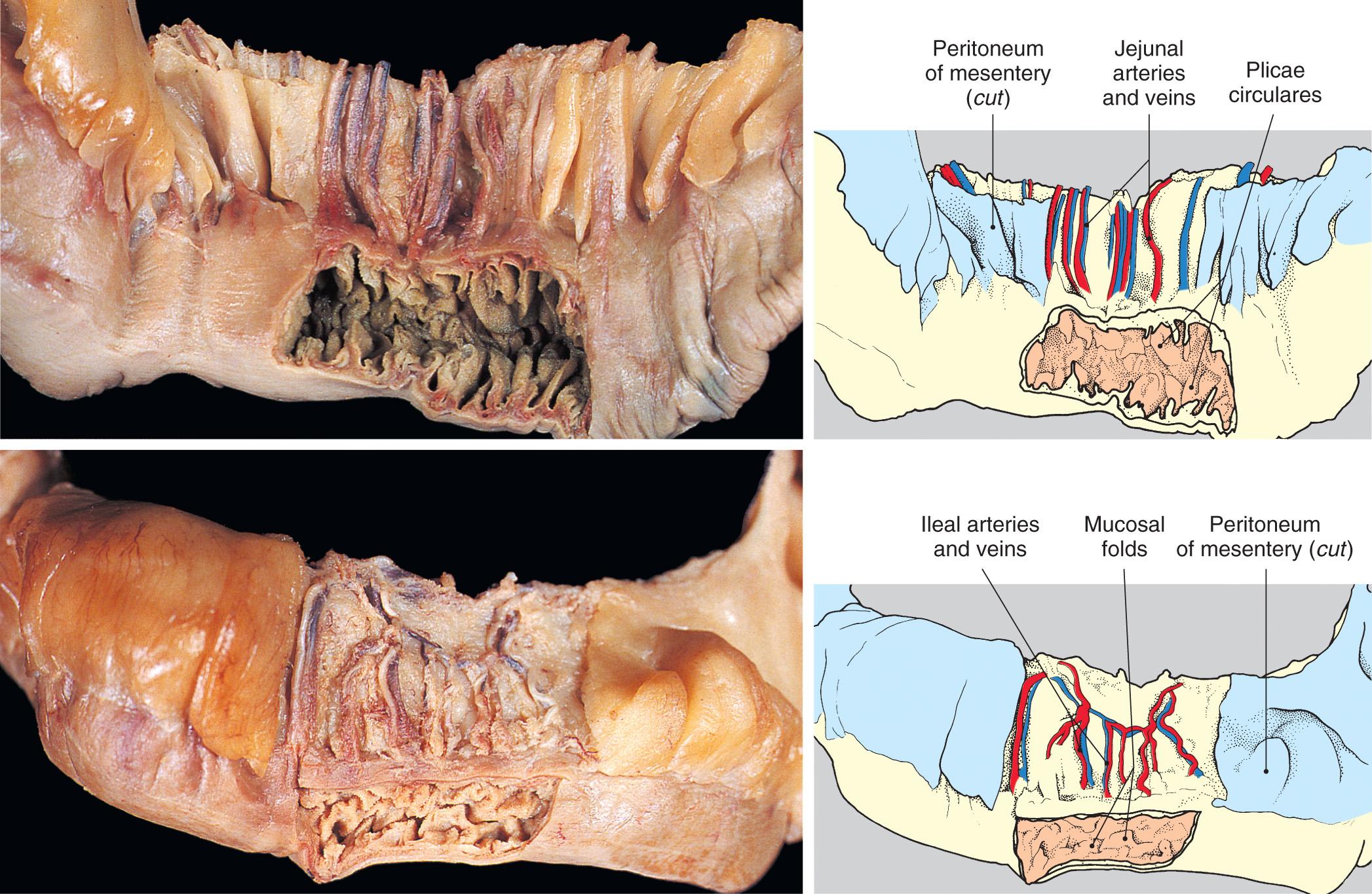
The jejunum and ileum lie within the peritoneal cavity and are anchored to the retroperitoneum by a broad-based mesentery. The average length of the jejunum and ileum is 5 meters: 40% jejunum, 60% ileum. The jejunum begins at the ligament of Treitz and the ileum ends at the ICV. The jejunum is located centrally in the abdomen, whereas the ileum lies mostly in the hypogastric region and pelvic cavity. There is no clear anatomic landmark that marks the transition from the end of the jejunum to the beginning of the ileum; they are instead distinguished by other anatomic characteristics. The jejunum has a thicker mucosal lining, thicker wall, larger diameter, less fatty mesentery, and longer and straighter vasa recta. Another distinguishing feature is the plicae circulares, also known as the valvulae conniventes, in the mucosa. Plicae circulares are transverse folds of mucosa and submucosa that aid in absorption of nutrients by increasing the surface area of the small intestine. These folds are deep and are visible on gross inspection even when the small intestine is distended ( Fig. 71.8 ) . They are prominent in the proximal intestine and diminish throughout the length of the small intestine. The plicae circulares are also visible radiographically, thus differentiating the small intestine from the large intestine, which is devoid of this feature.
The ICV is a distinct feature of the small intestine and operates independently of the ileum or colon. It prevents the fecal contents in the colon from entering the small intestine and controls the flow of contents from the small intestine into the colon. The ability of the ICV to control the flow of digested contents may also help to prevent malabsorption and diarrhea. The valve is triggered by distention in the small intestine or the colon. If the ileum becomes distended, the valve will relax and allow the passage of contents from the small intestine into the colon. If the colon becomes distended, however, the valve will close by increasing its tone to prevent the passage of contents from the colon into the ileum.
The structure and neural control of the ICV are still being investigated. Recent work suggests that the valve forms from an intussusception of the ileum into the cecum and that the myenteric and submucosal plexuses are present within the valve along with interstitial cells of Cajal. Three muscle layers, an external circular, inner circular, and a longitudinal muscle layer, are continuous between the ileum and cecum, suggesting the mechanism for the propagation of motor activity from the ileum into the cecum.
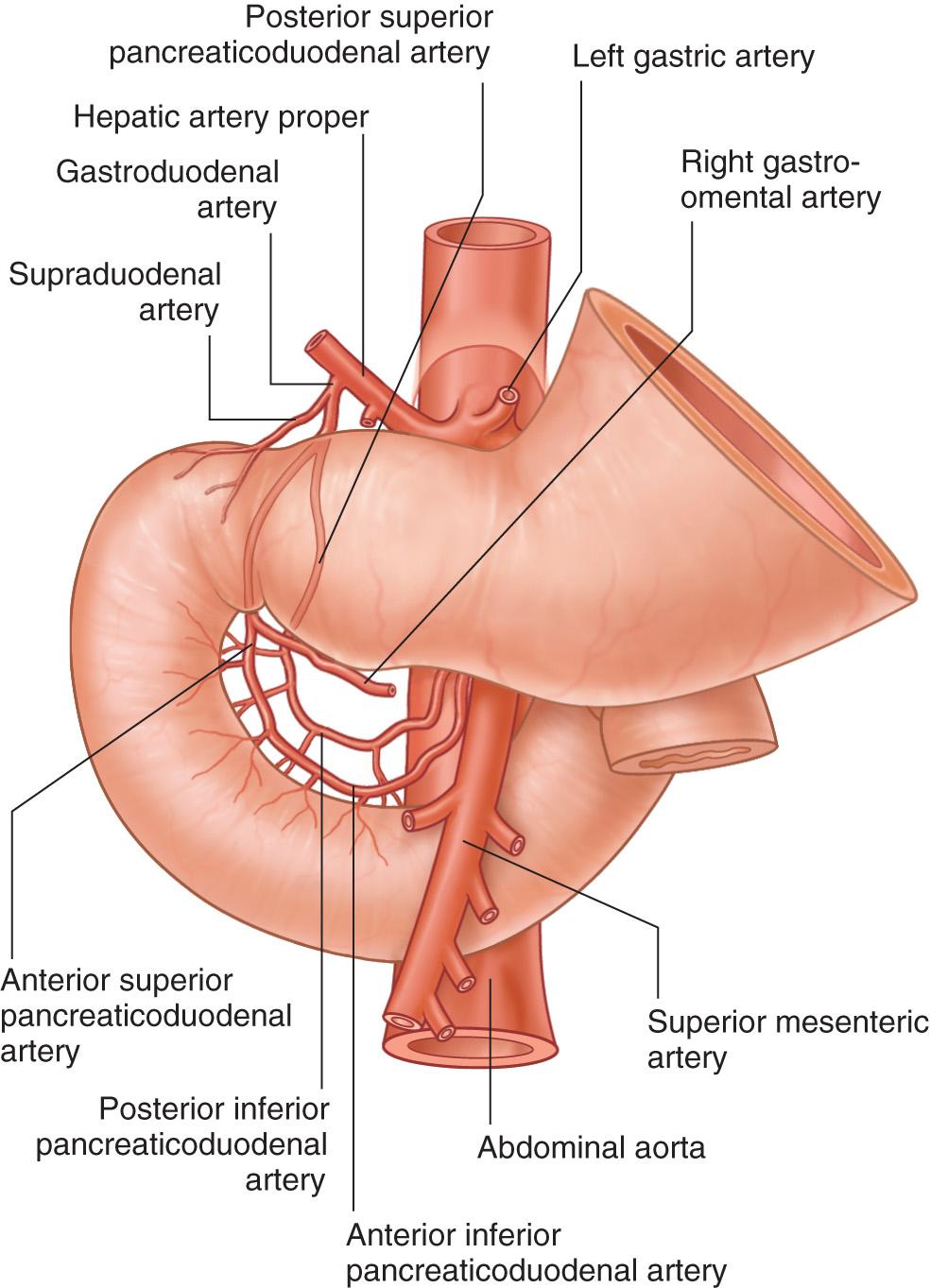
The small intestine is derived from the embryonic gut tube regions of the foregut and midgut. The celiac artery supplies the foregut and the superior mesenteric artery (SMA) supplies the midgut. The duodenum is both a foregut and midgut structure and thus receives dual blood supply. The jejunum and ileum are midgut structures and receive arterial blood from the SMA only ( Fig. 71.9 ) .
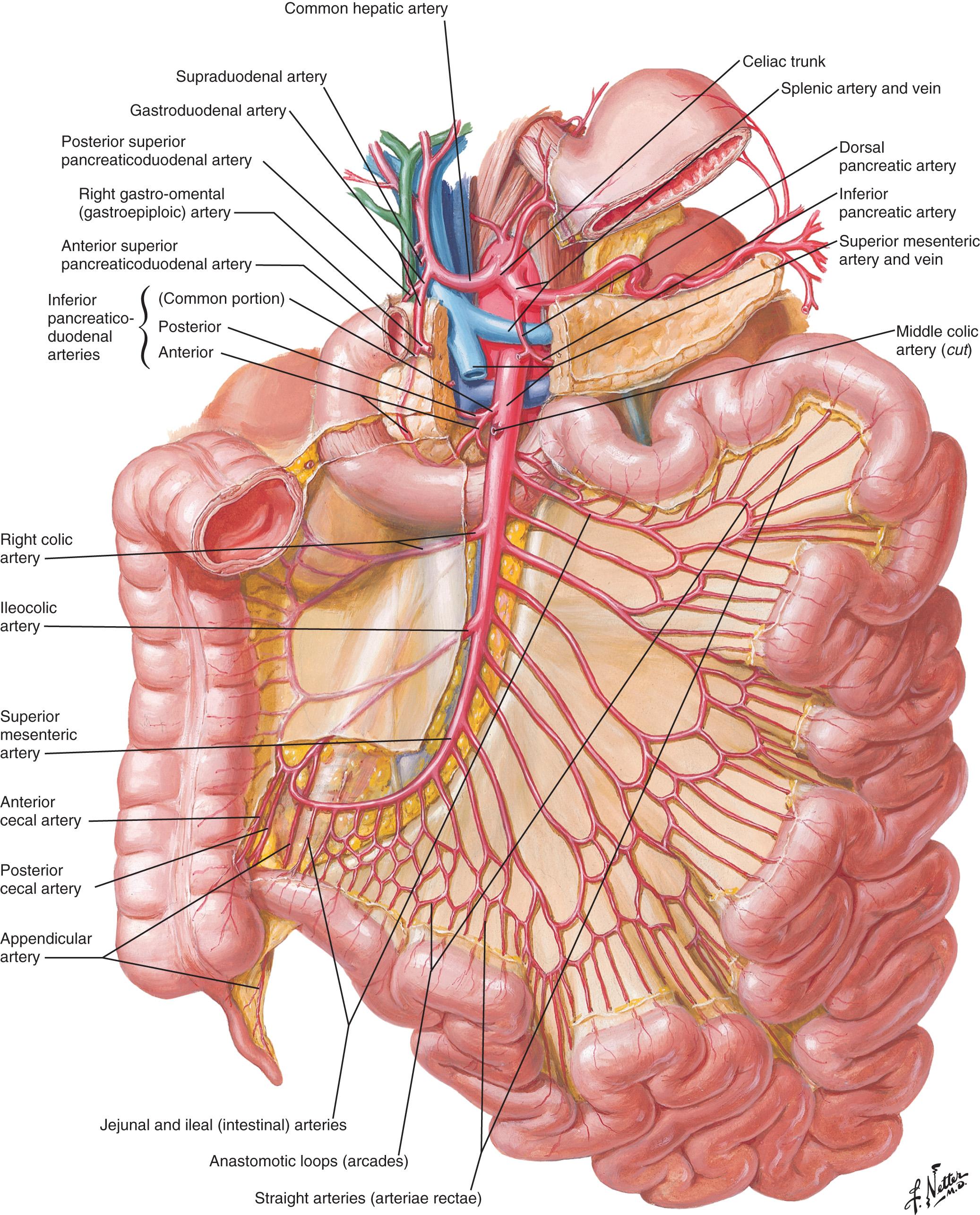
The celiac trunk gives rise to the common hepatic artery, which divides into the proper hepatic artery and the GDA. The GDA supplies branches to the duodenum, stomach, and pancreas. The anterior superior and posterior superior pancreaticoduodenal arteries arise from the GDA and supply blood to the second and third portions of the duodenum as well as the pancreas.
The SMA branches directly off of the aorta and supplies blood to the pancreas and to the second half of the duodenum to the mid transverse colon. The SMA gives rise to several branches that are important surgically. The posterior inferior and anterior inferior pancreaticoduodenal arteries anastomose with the superior pancreaticoduodenal arteries from the GDA to supply blood to the duodenum and pancreas. The intestinal arteries are branches from the SMA that create a unique network of arteries known as an arcade that supply the jejunum and ileum. Arterial branches known as vasa recta course from the arcade to the intestinal wall. These arteries then bifurcate and travel along the intestinal wall to provide adequate blood flow. The vasa recta represent another anatomic variant to help distinguish the jejunum from the ileum. The vasa recta of the jejunum are straight and long, whereas those supplying blood to the ileum are arborized and short (refer to Fig. 71.8 ). The ileocolic artery supplies blood to the ileum, cecum, right colon, and appendix.
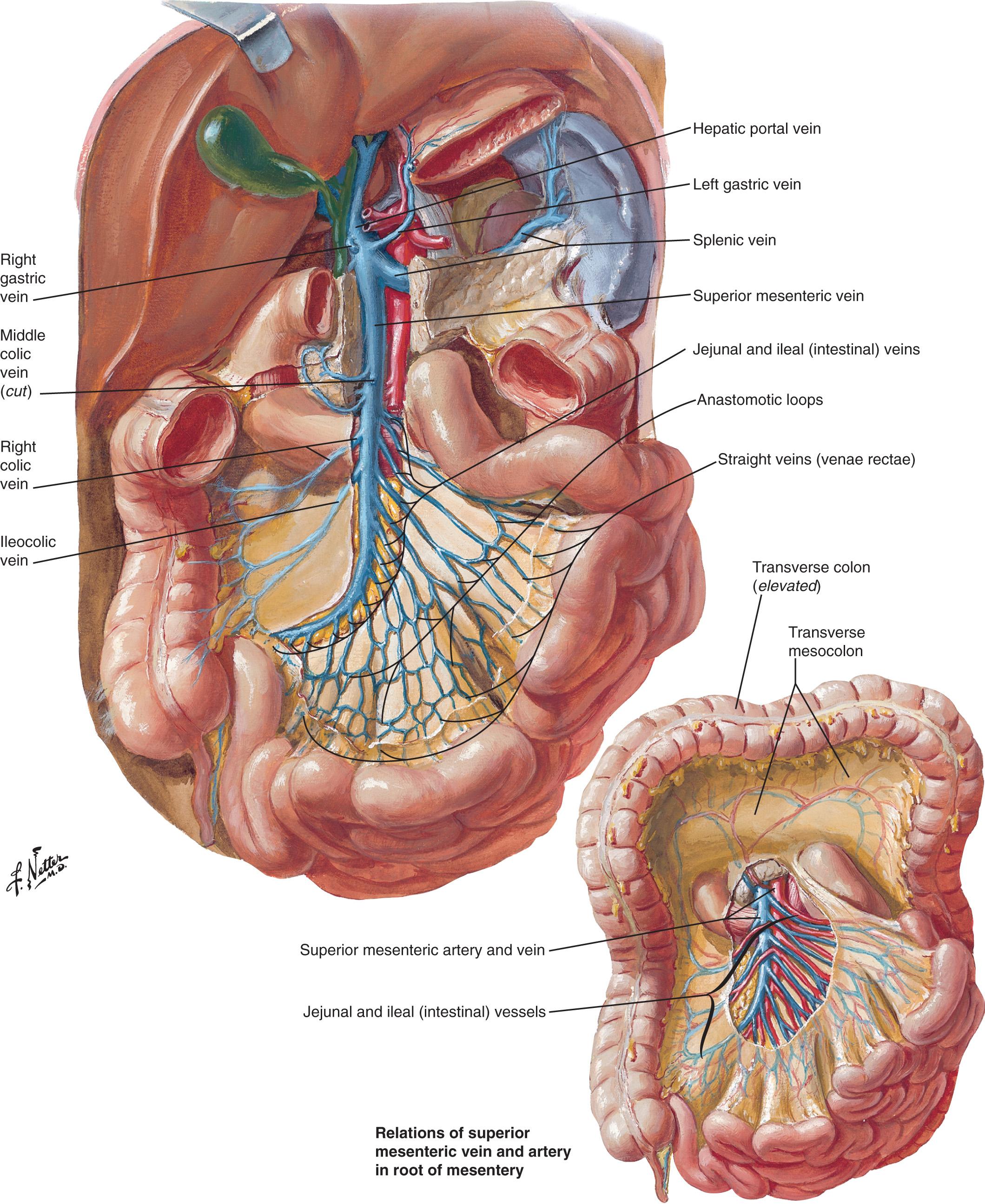
The venous drainage of the small intestine mirrors the arterial supply. The duodenum empties into the pancreaticoduodenal, the right gastroepiploic, and the portal vein. The jejunum and ileum are drained by the superior mesenteric vein, which joins with the splenic vein to drain into the portal vein ( Fig. 71.10 ).
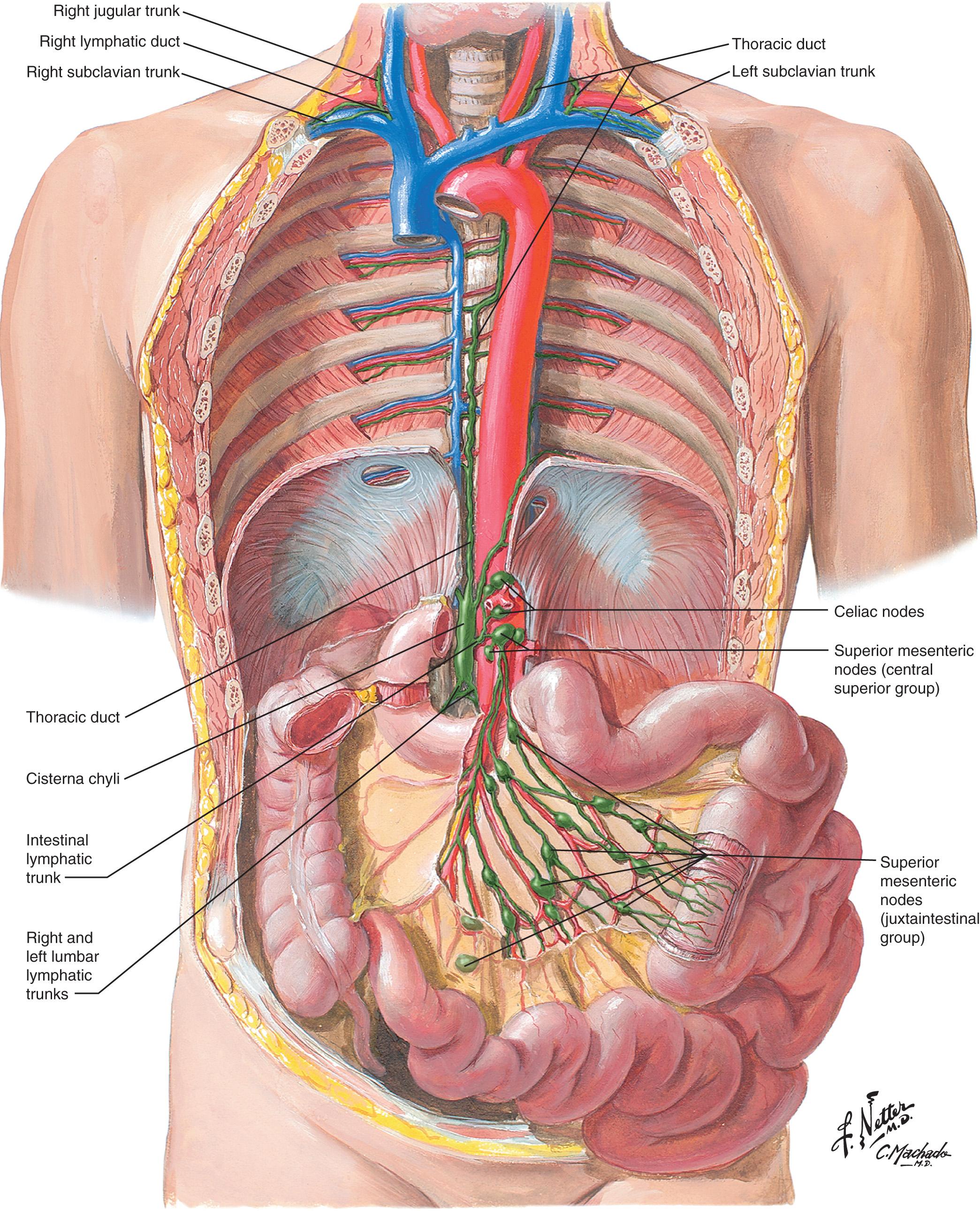
There are several levels of lymphatic drainage of the small intestine that follow the vasculature. The lymph drains into the nodal chain adjacent to the bowel wall and then into the nodes of the mesenteric arcade. From there the lymphatic vessels follow along the trunk of the SMA and join with the two lumbar lymphatic trunks to drain into the cisterna chyli. The cisterna chyli is located below the level of the diaphragm at the end of the thoracic duct anterior to the lumbar spine and posterior to the aorta. Once lymph collects in this dilated sac, it will then pass through the aortic opening of the diaphragm and flow into the main thoracic duct. The thoracic duct runs parallel with the aorta and empties into the left subclavian vein where it joins the jugular vein ( Fig. 71.11 ) .
The innervation of the small intestine is composed of two separate systems that function independently. The autonomic nervous system (ANS) is derived from the central nervous system (CNS). The ENS is a specialized nervous system found only in the GI tract. This system is composed of neurons that lie within the bowel wall that respond to local and systemic stimulation. Parasympathetic and sympathetic nerve fibers connect the ENS to the CNS and can modulate the activity of the ENS in response to external stimuli. The ENS also functions independently, regulating its own function in response to intrinsic stimuli. There are also sensory neurons in the bowel wall that provide feedback to the ENS, the sympathetic system, the spinal cord, and the brainstem.
The ANS is composed of sympathetic and parasympathetic nerve fibers. The sympathetic innervation to the intestine is derived from nerve fibers located in the thoracolumbar spinal cord between segments T5 and L2. The paravertebral ganglia are located along either side of the vertebral column and span the length of the spinal cord. The prevertebral ganglia include the celiac, mesenteric, and hypogastric ganglia and are located along the aorta and its branches. The sympathetic innervation travels via preganglionic and postganglionic fibers. The sympathetic system secretes norepinephrine, which results in a direct inhibition of the smooth muscle. It also works indirectly by stimulating an inhibitory response from the ENS. Stimulation of the sympathetic system results in decreased intestinal motility, decreased secretion, and vasoconstriction.
The parasympathetic system is composed of nerve fibers that leave the CNS via the cranial nerves and the sacral spinal nerves. The paired vagus nerve (cranial nerve X) provides parasympathetic innervation to the thoracic and abdominal viscera, which includes the pyloric sphincter and small intestine. The parasympathetic nervous system, like the sympathetic system, has preganglionic and postganglionic neurons. The length and location of these nerve fibers and neurons is a distinguishing feature between the parasympathetic and sympathetic systems. The preganglionic parasympathetic fibers are relatively long and often pass uninterrupted from the CNS to the viscera. In the small intestine, the postganglionic neurons are located within the bowel wall as part of the myenteric and submucosal plexuses. The postganglionic nerve fibers are very short because they have only a minimal distance to travel to innervate the surrounding tissue. When the intestine is under the influence of parasympathetic stimulation, there is increased intestinal motility and secretion.
The ENS is an independently functioning system that can affect motility, secretion, vascular tone, and hormone release in the small intestine. The system, derived from the neural crest, is made up of more than 100 million neurons. The vagal neural crest is the source of the precursors that give rise to the ENS. Sacral neural crest cells also play a role in populating the distal gut; however their purpose is less well understood. Neural crest cells populate the gut via two main pathways: the RET/GFRα1/GDNF pathway and the EDNRB/Endothelin-3 pathway. This is significant because while loss-of-function mutations in the RET gene are associated with Hirschsprung disease, gain-of-function mutations are associated with neuroendocrine neoplasms. The cell bodies lie within the bowel wall and reside within two named plexuses. The myenteric, or Auerbach, plexus is located between the longitudinal and circular muscle layers. The submucosal, or Meissner, plexus is located in the submucosa of the bowel wall between the circular muscle layer and mucosa. Once the myenteric plexus is populated with neural crest cells, they migrate inward to populate the submucosal plexus. This process is driven by netrins.
The myenteric plexus runs the entire length of the intestinal wall and provides innervation to the muscular layers. Its main function is to control motor activity of the intestine. Stimulation of the myenteric plexus can result in excitatory or inhibitory effects. Excitatory effects include increased intestinal wall tone, increased intensity and rate of rhythmic contractions, and increased velocity of excitatory waves resulting in increased peristalsis. When inhibitory peptides are released, they act at the pyloric valve and ICV.
The submucosal plexus provides innervation to intestinal glands, endocrine cells, and blood vessels. It works at a local level to control the secretion, absorption, and contraction within each segment of the intestine.
Small intestinal motility is regulated through a combination of myogenic, neural, and hormonal factors. Of these three, myogenic factors are the most important. Neural and hormonal factors act to modify myogenic-initiated motor patterns. Intestinal motor activity can persist even with complete blockade of neural signals.
Intestinal motor activity exists in two phases: a fed state and a fasting, or interdigestive, state. During the fed state, food is moved along the intestine via segmentation and peristalsis. Segmentation is characterized by a pattern of pressure waves traveling short distances that serve to mix chyme and enhance its contact with the villous surfaces. The peristaltic pattern moves food along the intestine by a muscular contraction proximal to the food bolus and relaxation distal to the bolus.
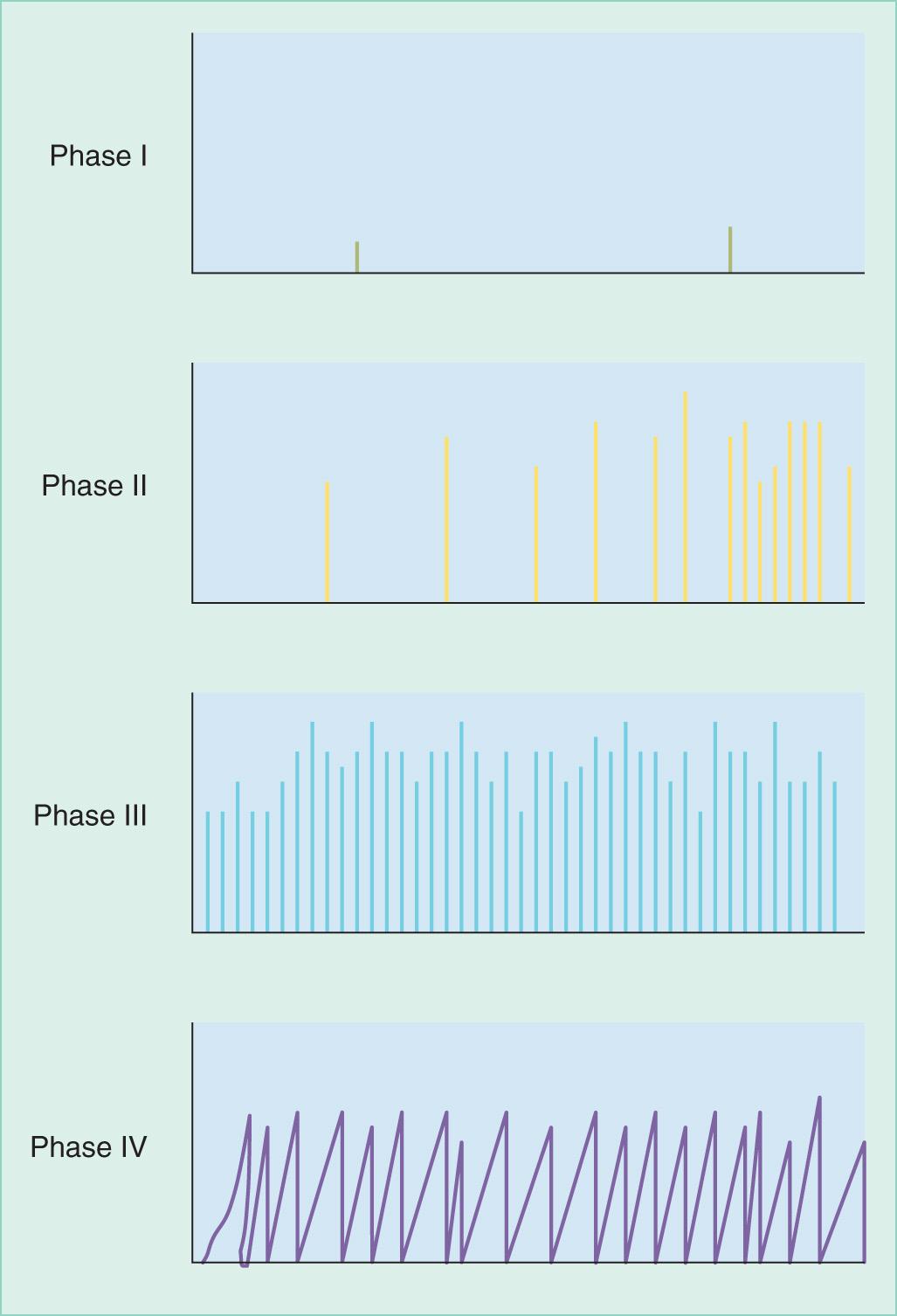
Motor activity continues during the interdigestive state via the migratory motor complex (MMC). The purpose of this activity is to propel undigested material through the small intestine and into the colon. It also prevents reflux of bacteria from the colon into the terminal ileum. The MMC begins in the stomach and moves distal. Peristalsis occurs when these MMC electrical spikes are superimposed on intrinsic pacemaker potentials. There are three phases of the MMC. Phase I is characterized by an absence of motor activity, phase II consists of disorganized high-pressure waves that are accelerating in rate and occur intermittently, phase III is characterized by a continuous high rate of rhythmic contractions, and in phase IV the contractions once again become intermittent. This cycle repeats every 1.5 to 2 hours ( Fig. 71.12 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here