Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Anorectal suppurative disease may manifest itself in an acute or a chronic setting. Anal sepsis (abscess) represents the acute manifestation, and anal fistula represents the chronic form of the suppurative process. In its simplest form, an anal fistula represents a communication between an internal opening in the anal canal and an external opening through which an abscess has drained. A fistula and abscess may coexist or be associated with atypical internal openings and multiple tracts that result in a complex suppurative process.
Foreign bodies, malignancy, trauma, tuberculosis, actinomycosis, leukemia, postoperative infection, inflammatory bowel disease, and simple skin infections have long been associated with anal sepsis. Recently an association between anal abscess-fistula and history of concurrent or recent cigarette smoking has been demonstrated. This association diminishes as the history of cigarette smoking grows more remote. However, most anal sepsis is related to an infection of the anal glands and ducts. Fecal bacterial plugging of the ducts leads to obstruction and subsequent abscess formation. This process represents the cryptoglandular theory of anal sepsis. Robinson, Seow-Choen, and their associates have suggested that the description of the anal glands by Chiari in 1878 and the subsequent histologic studies of Parks in 1961 contributed to the acceptance of the cryptoglandular theory as the most common cause for anal sepsis.
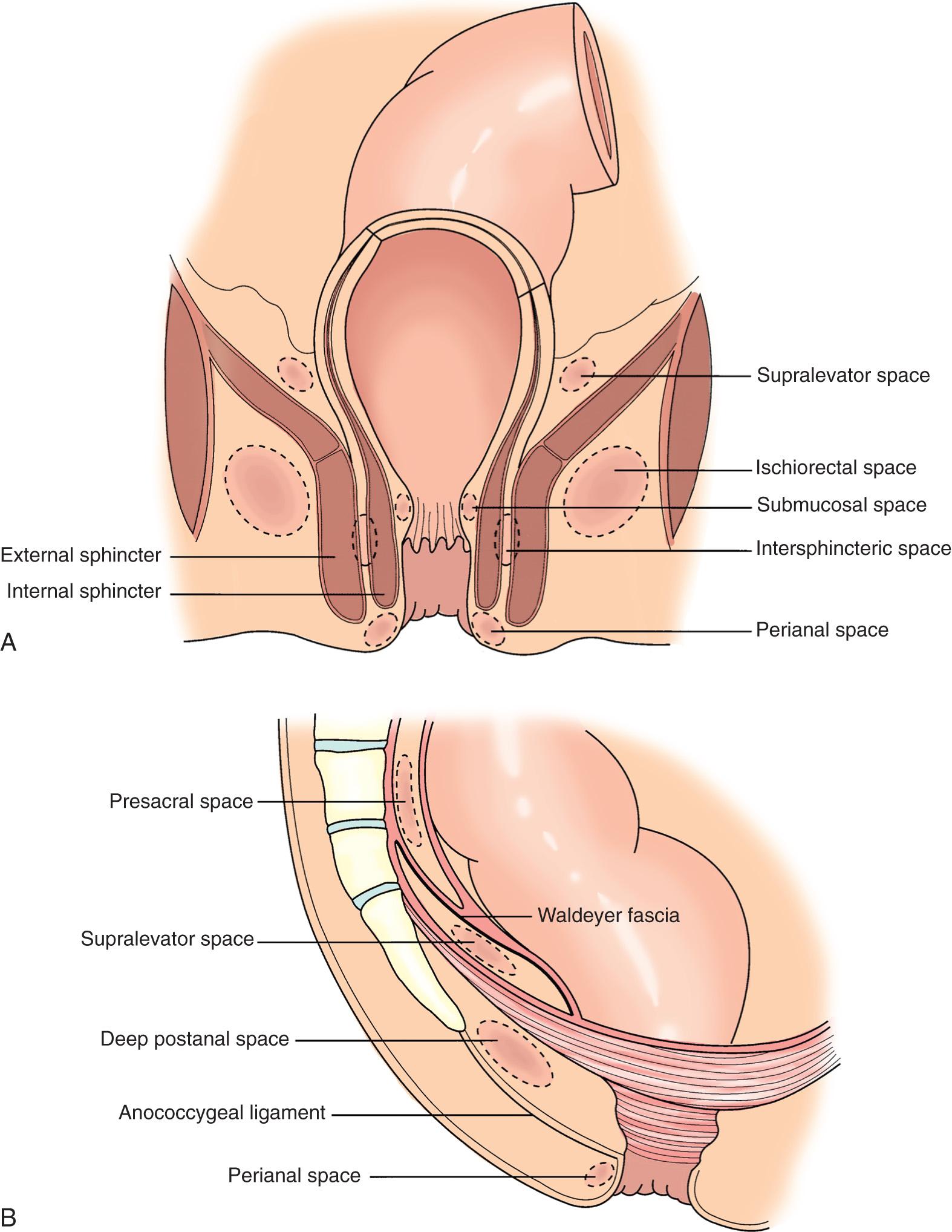
Anorectal abscesses are classified according to the perirectal space involved in the suppurative process; these include the perianal, ischiorectal, intersphincteric, submucosal, deep postanal, and supralevator spaces ( Fig. 160.1 ). A given suppurative process may involve multiple perirectal spaces. For example, the classic “horseshoe” abscess originates in an infected gland in the posterior midline extending through the intersphincteric and deep postanal spaces to one or both of the ischiorectal spaces. A condition known as “floating anus” may occur with circumanal spread of intersphincteric, supralevator, or ischiorectal collections.
It is difficult to accurately assess the incidence of various abscesses because of the numerous classifications and referral patterns reflected in large series. However, perianal abscesses account for the largest number in most series ( Table 160.1 ).
| Abscess Locations | NO. OF PATIENTS | TOTAL | |||||
|---|---|---|---|---|---|---|---|
| McElwain et al. | Scoma et al. | Vasilevsky and Gordon | Schouten and van Vroonhoven | Ramanujam et al. | No. of Patients | % | |
| Perianal | 456 | 174 | 20 | — | 437 | 1087 | 44.8 |
| Submucosal | 3 | — | — | — | — | 3 | 0.1 |
| Intermuscular | 541 | 30 | — | — | 59 | 630 | 26 |
| Intersphincteric | — | — | 18 | 28 | 219 | 265 | 11 |
| Transsphincteric | — | — | — | 30 | — | 30 | 1.2 |
| Ischiorectal | — | 14 | 63 | — | 233 | 310 | 12.8 |
| Supralevator | — | 9 | 2 | — | 75 | 86 | 3.6 |
| Retrorectal | — | 5 | — | — | — | 5 | 0.2 |
| Unclassified | — | — | — | 8 | — | 8 | 0.3 |
| Total | 1000 | 232 | 103 | 66 | 1023 | 2424 | 100 |
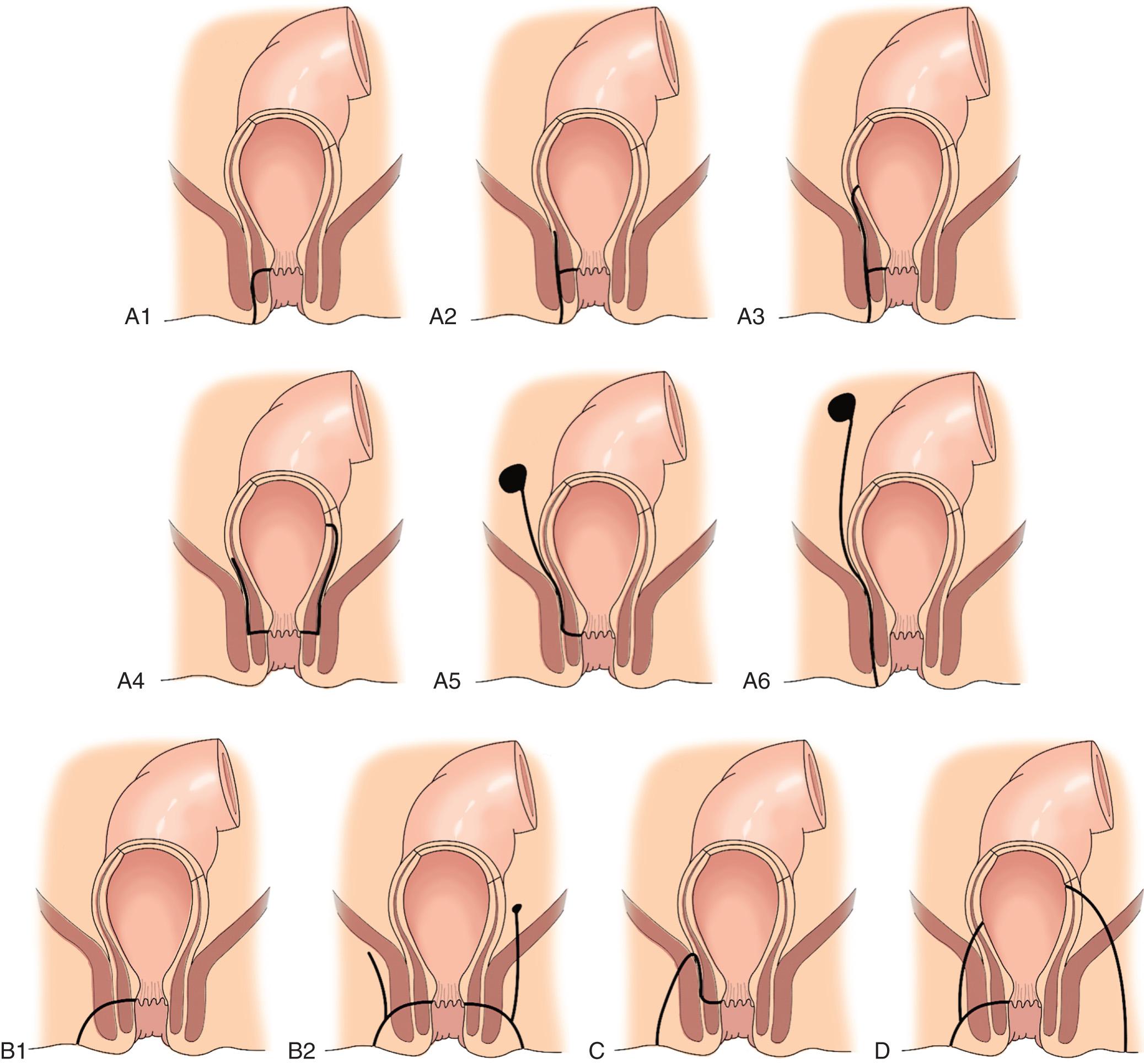
Historically, anal fistulas have been classified in many different ways. However, the Parks classification introduced in 1976 is the most comprehensive and widely used. It is derived from the cryptoglandular hypothesis and has therapeutic implications. Parks and Gordon classified fistulas into four main subgroups according to the course taken by the main tract: intersphincteric, transsphincteric, suprasphincteric, or extrasphincteric. Each category can be further subclassified based on associated secondary tracts and other anatomic details ( Fig. 160.2 ). As with abscesses, the incidence of various fistulas is difficult to quantify. However, overall, intersphincteric fistulas seem to predominate ( Table 160.2 ).
| Fistula Type | NO. OF PATIENTS | TOTAL | ||||
|---|---|---|---|---|---|---|
| Parks et al. | Marks and Ritchie | Vasilevsky and Gordon | Garcia-Aguilar et al. | No. of Patients | % | |
| Intersphincteric | 180 | 428 | 67 | 180 | 855 | 49.5 |
| Transsphincteric | 120 | 167 | 83 | 108 | 478 | 27.7 |
| Suprasphincteric | 80 | 24 | 3 | 6 | 113 | 6.5 |
| Extrasphincteric | 20 | 24 | 0 | 6 | 50 | 2.9 |
| Miscellaneous or unclassified | — | 150 | 7 | 75 | 232 | 13.4 |
| Total | 400 | 793 | 160 | 375 | 1728 | 100 |
Symptoms common to all abscesses include the slow, gradual onset of pain, increasing in intensity to the sensation of pressure and fullness. This is a constant, nonrelieving sensation. These symptoms should always lead to the consideration of an abscess even in the absence of obvious physical findings (hidden abscesses). Approximately 20% to 33% of all patients will report a history of a previous episode of anorectal sepsis.
The physical findings associated with anorectal abscesses vary depending on the anatomic location of the abscess. The presence of pus in any of the perianal and perirectal spaces may be confirmed with needle aspiration. An examination under general anesthesia may be necessary to confirm the diagnosis.
Localized swelling, hyperemia, induration or fluctuance, and tenderness are present adjacent to the anus. A purulent discharge may be present if spontaneous drainage has occurred. Although there usually are no systemic symptoms, the patient may have fever or malaise or be acutely ill.
Although small collections may present with discrete localized swelling, more commonly there is a large, erythematous, and indurated mass in the buttock. Large volumes of purulent material may accumulate in the ischiorectal space. Fever and leukocytosis are common but not always present. A large ischiorectal abscess frequently represents a horseshoe extension (see later). A source in the posterior midline should be sought.
The intersphincteric and submucosal abscesses usually present with no visible evidence of sepsis because these “hidden abscesses” are confined to the anal canal. Owing to the patient's discomfort, a digital rectal examination is not always possible. In this situation, an examination under general anesthesia is warranted to identify the abscess.
Supralevator abscess may occur as an upward extension of a collection in the distal anal canal, usually an intersphincteric abscess, or as a true pelvic abscess secondary to intraabdominal or pelvic pathology. Possibilities include appendicitis, diverticulitis, pelvic inflammatory disease, or ruptured viscus. The patient may be systemically ill. A pelvic mass may be identified by rectal or vaginal examination.
Transsphincteric extension of an intersphincteric abscess in the posterior midline leads to the accumulation of purulent material in the deep postanal space. This space is difficult to evaluate clinically, making these the second type of hidden abscess. Inspection does not reveal any inflammatory skin changes because the abscess is deep. There may be tenderness posterior to the anus but anterior to the coccyx. The collection may be apparent only by needle aspiration or with an examination under general anesthesia. A horseshoe abscess is the result of a direct extension of a postanal abscess into the ischiorectal space (see section Ischiorectal Abscess ). It may be unilateral or bilateral.
Most patients with a fistula-in-ano have a previous history of anorectal suppuration. The patient usually presents with complaints of intermittent or persistent purulent or serosanguineous drainage from an external opening in the perianal area. Symptoms classically consist of a buildup of pain, slight fever, and pain on defecation followed by mucopurulent drainage and abatement of the pain. Pruritic symptoms may be present because of skin irritation associated with the chronic discharge.
Fistula tracts are fibrous inflammatory tubes with a diameter of 3 to 7 mm. They are lined with infected granulation tissue. Many fistulas may be palpated during a careful digital rectal examination. Essential points that should be obtained from a clinical examination were described nearly 100 years ago by Goodsall and Miles ; they include the identification of the external and internal openings, the course of the primary and any secondary tracts, the tone of anal sphincters and an assessment for the presence of an underlying complicating disease.
Using an anoscope, systematic inspection and palpation can define most of these characteristics. The gentle use of a number of malleable anorectal probes and crypt hooks can help to delineate the fistula by attempting to pass these instruments via the internal or external opening. It is important not to force the passage of the probe because the development of false tracts can complicate evaluation and management. Secondary tracts may be present when induration is palpated or asymmetry is noted between the right and left sides of the anorectum. In some cases, such as recurrent, extensive, or complex fistulas, the use of sophisticated imaging techniques may yield additional information to guide successful therapy.
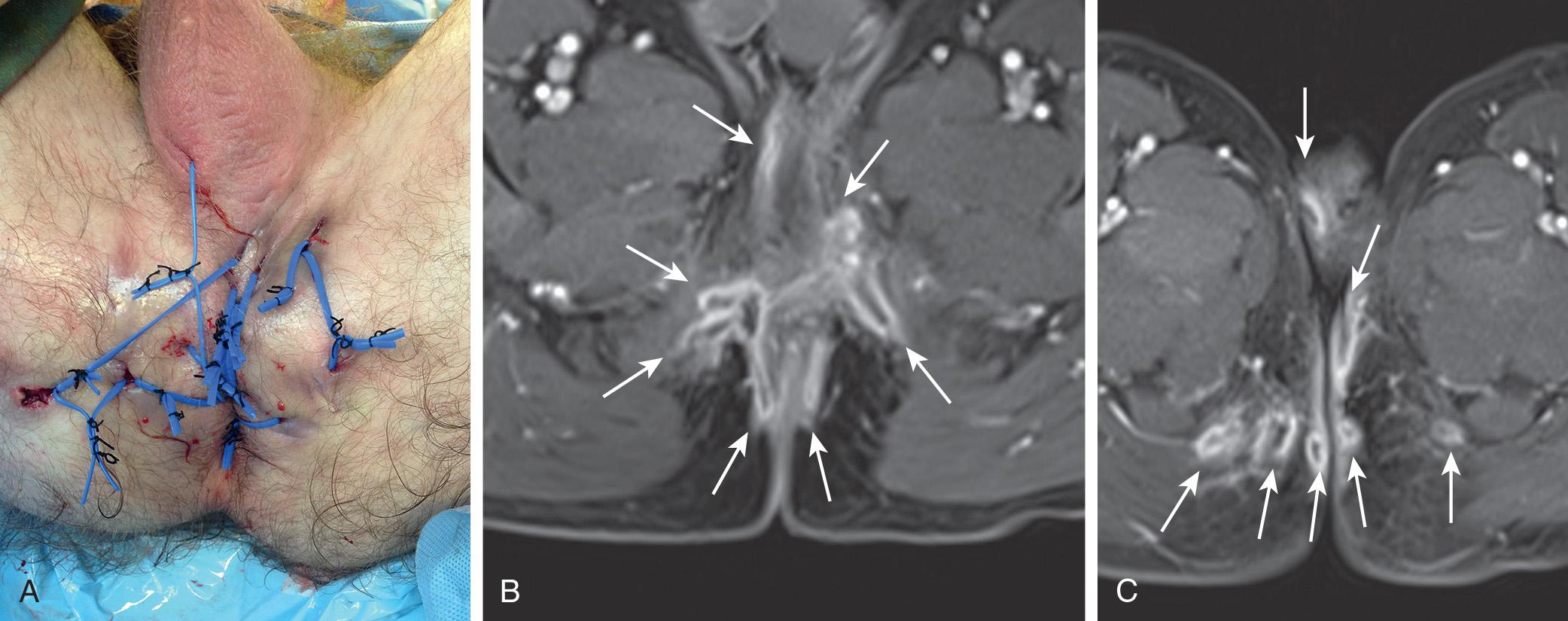
The external opening is identified as a small pit surrounded by scar or granulation tissue. Active seropurulent drainage may be present. Intersphincteric tracts usually open externally close to the anal verge; transsphincteric and other complicated tracts open farther away. Occasionally the external opening may be localized inside the anal canal or at the distal end of a fissure. Several external openings may be present because of multiple complex fistula tracts; this condition is known as watering can perineum ( Fig. 160.3 ).
The internal opening may be felt as an indurated nodule, most often at the dentate line. This is consistent with the cryptoglandular theory of anorectal sepsis. The use of saline, milk, dye, or dilute hydrogen peroxide as an injection into the external fistula opening has been made in an attempt to localize the internal opening. An enlarged papilla may be noted at this site. Because most of the anal glands are located in the posterior midline, it is not surprising that 61% to 69% of internal openings can be traced to this location.
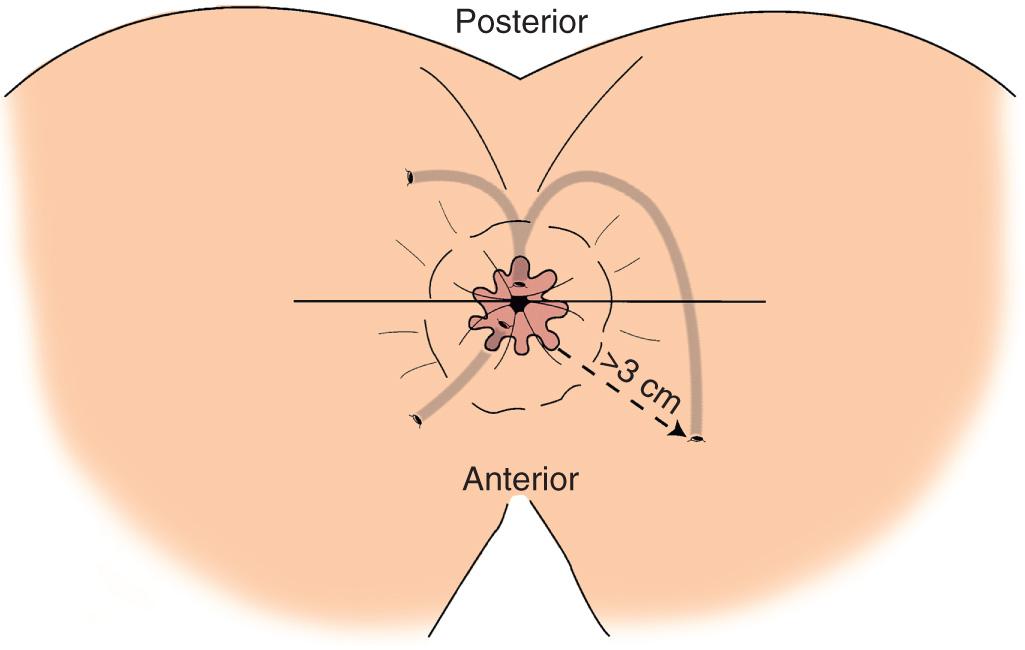
The Goodsall rule may be helpful in locating the internal opening. This rule states that an external opening anterior to an imaginary transverse anal line in the coronal plane most likely communicates with an internal opening lying at the end of a radial line drawn to the nearest crypt at the dentate line. If the external opening is posterior to this line, the internal opening will most likely be located in the posterior midline with the tract following a curved route to reach its source. Exceptions to this rule include anterior openings more than 3 cm from the anal verge and the presence of multiple external openings. In these cases, the internal opening will most likely be in the posterior midline ( Fig. 160.4 ). However, the predictive accuracy of Goodsall rule has been challenged, especially with anterior external openings or when Crohn disease or carcinoma is present.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here