Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
An attractive upper face is a result of a permutation of skeletal and soft tissue relationships. This chapter will focus on the importance of adequate skeletal support of the midface soft tissue, the lid–cheek junction, and the globe–orbital rim relationships in utilizing the application of alloplastic implants.
Concave faces, perhaps because they are not as common, are often considered not as attractive as convex ones. Furthermore, the deficient midface skeletal projection intrinsic to concave faces poorly supports the midface soft tissues, resulting in premature lower lid and cheek descent, as well as visible bags. These faces are also “morphologically prone” to further lower lid descent after blepharoplasty. Finally, a concave midface also makes the eyes and nose appear more prominent. It is in this population that midface skeletal augmentation with multiple implants can simulate the visual effects of skeletal osteotomy and advancement.
The implants used to effect these changes include ones that augment the infraorbital rim, the piriform aperture, and the malar area. These implants are all modified so as to meet the specific needs of the patient. Multiple implants are used so that the infraorbital nerve is not compromised and the complex curvature of the midface skeleton can be mimicked.
Repositioning midface soft tissues has several benefits. It restores cheek fullness and recreates a cheek–lid interface with a relatively shortened lower lid, while narrowing the palpebral fissure shape by raising the lower lid margin.
This chapter presents the rationale and surgical technique for transforming a concave face into a convex one. It requires the use of multiple implants, together with a subperiosteal midface soft tissue resuspension.
Midface and orbital skeletal abnormalities have multiple etiologies: developmental, traumatic, oncologic, or iatrogenic. When evaluating a patient, it is important to obtain a thorough history to determine whether the patient is a candidate for alloplastic reconstruction.
When evaluating a patient with midface deficiency, it is important to be aware if there is an underlying syndrome or medical condition contributing to the midface hypoplasia. It is important to know if the patient has undergone previous surgery, which may alter the topical surface anatomy of the underlying skeletal bone. Airway problems, such as obstructive sleep apnea, must be investigated and evaluated, if suspected. It is important for the surgeon to know if the patient has previously undergone orthodontic treatment. In patients with midface deficiency, the occlusion may be normal or has been compensated by orthodontics. In patients with skeletal deficiency with normal occlusion or occlusion that has been previously normalized by orthodontics, skeletal repositioning would necessitate additional orthodontic tooth movement. Such a treatment is time consuming, costly, and potentially morbid. It is therefore appealing to few patients.
Craniofacial syndromes: Several craniofacial syndromes result in midface hypoplasia. These cases are typically severe, and these patients are usually monitored by craniofacial teams. The surgical approaches to this population tend to be more aggressive and are beyond the scope of this textbook.
Compensated class III malocclusion: These patients have had their malocclusion treated with orthodontics, yet the jaw discrepancy persists. These patients exhibit a normal occlusion, yet their midface deficiency persists.
Postorthognathic surgery: These patients have undergone orthognathic surgery to correct their malocclusion, and yet the midface hypoplasia persists. In spite of a high LeFort osteotomy, a postsurgical patient may exhibit improved, but persistent, midface deficiency after jaw surgery.
The relationship between the globe and the orbital rims will determine whether the eyes appear prominent or deep set. Because the upper midface skeleton, including the orbital rim, supports the lower eyelid and malar soft tissues, its projection will impact the position of the lower lid and cheek. On average, the soft tissues overlying the supraorbital rim lie 10 mm anterior to the cornea and the soft tissues overlying the infraorbital lie 3 mm anterior to the cornea ( Fig. 24.1 ). When the orbital rims have greater than average projection compared with that of the globe, the eyes can appear deep set. When the opposite is true, the eyes can appear prominent, which is usually considered less attractive. Globe-to-orbital rim measurements can be influenced by ethnicity, gender, and change over time with aging.
Using a Hertel exophthalmometer, which measures the projection of the anterior surface of the cornea in relationship to the lateral orbital rim, Migliori and Gladstone determined that the projection was, on average, 10 mm in white adults and 12 mm in black adults. In addition, male globes were on average 2 mm more prominent than those of females, and the globes in black males and females were 2 mm more prominent than those of white males and white females.
The globe–orbital rim relationship has also been found to change with aging, resulting in less attractive and more prominent eyes. In a youthful face, the cheek fat lies anterior to the cornea and the orbital fat slightly anterior to the inferior orbital rim. With aging, the cheek mass descends and deflates resulting in posterior-to-anterior position of the surface of the cornea. In addition, the orbital fat bulges more anteriorly, and the orbital rim recedes due to bone loss. Thus with aging, the result is a lower cheek mass, prominent orbital fat, and a more prominent globe-to-rim relationship. This is particularly noticeable in patients who have a tendency toward maxillary hypoplasia. ,
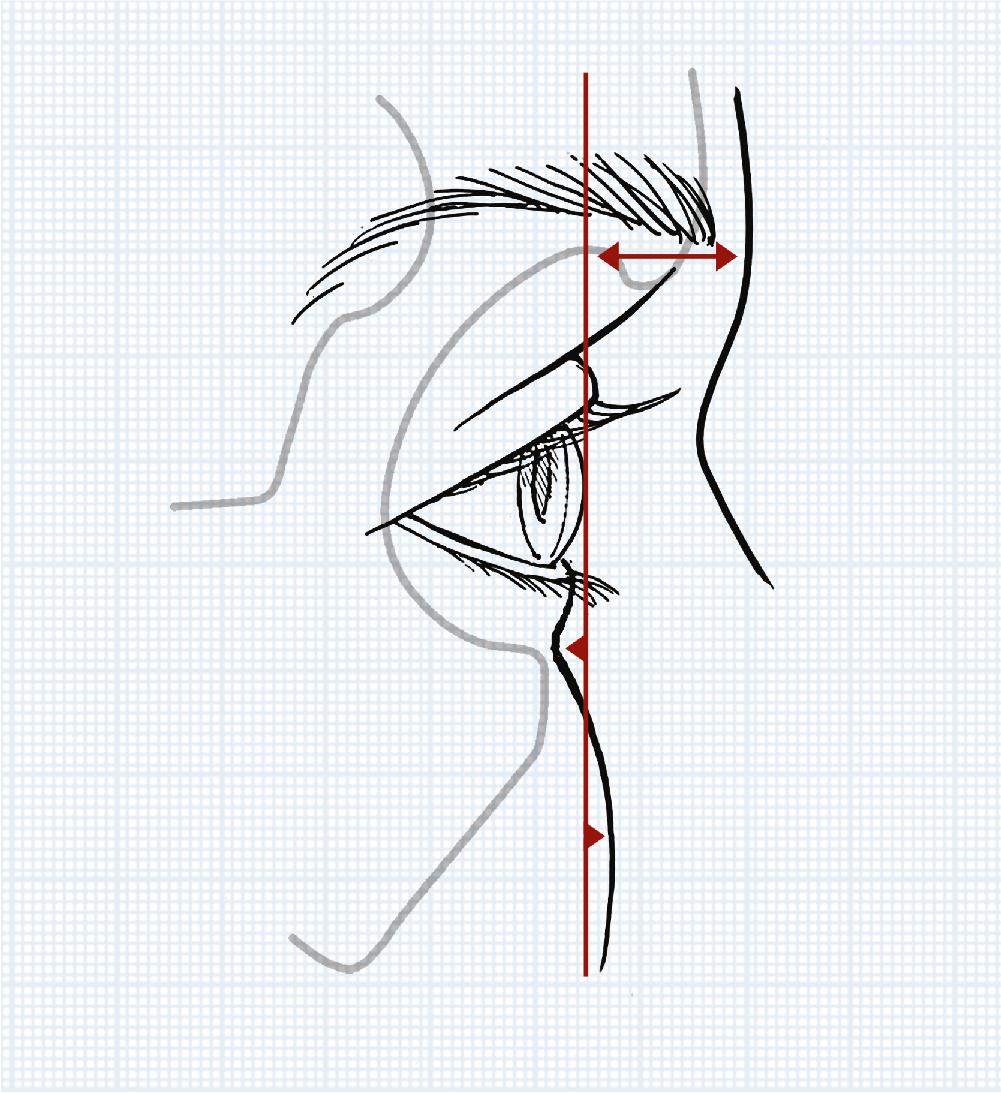
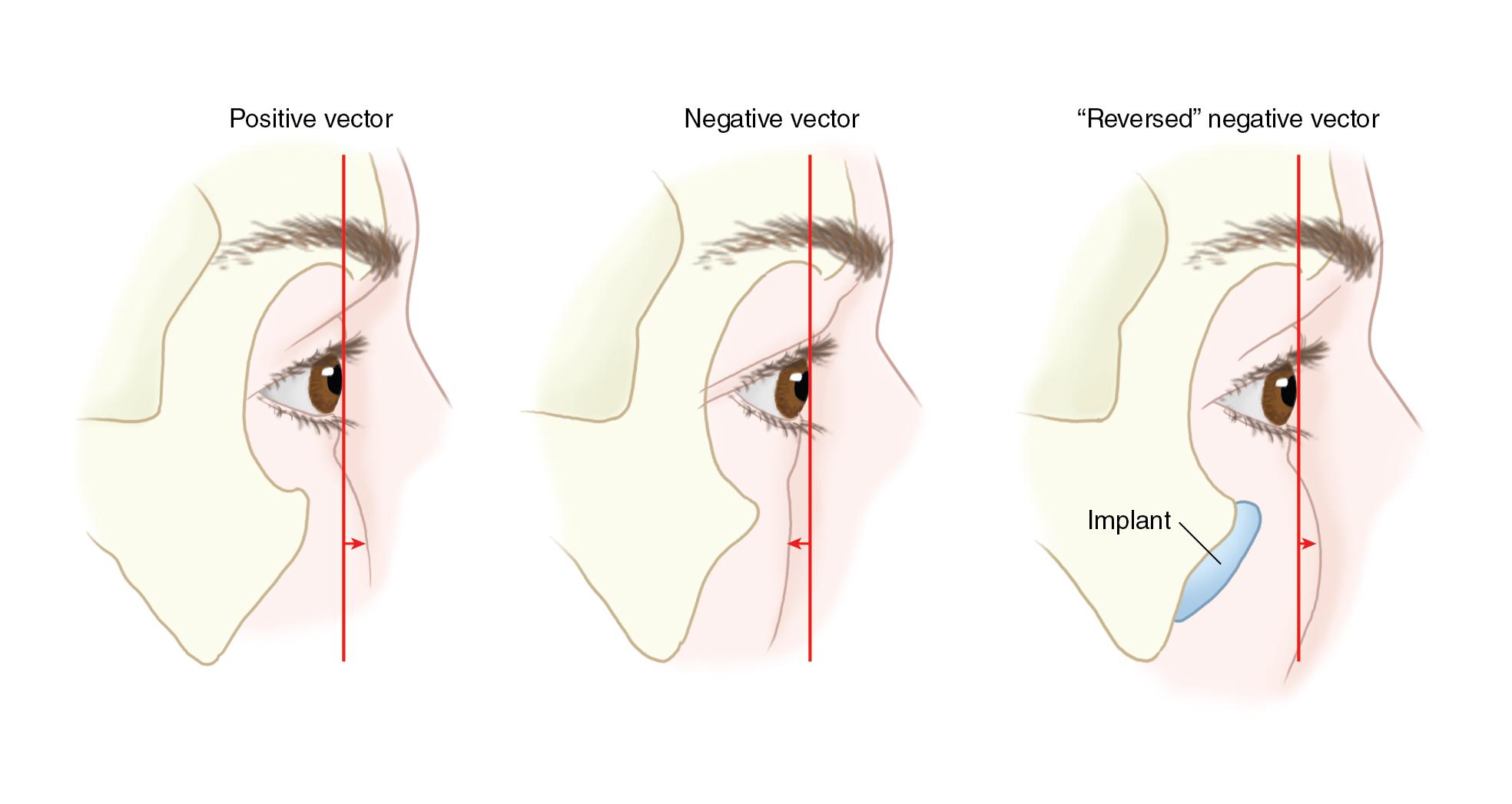
Patients with prominent eyes may be predisposed to developing symptomatic lower lid descent with scleral show. This is most likely due to lack of skeletal support of the lower lid and cheek pad. On sagittal examination of the patient, a vertical line can be dropped at the most anterior projection of the globe. A “positive vector” exists when the malar eminence and lower lid margin lie anterior to the globe. A “negative vector” is defined by the most anterior projection of the globe anterior to the lower lid and malar eminence ( Fig. 24.2 ). It is important to identify patients with a negative vector because these patients can be predisposed to lower lid malposition after blepharoplasty and can benefit from canthopexy, augmentation of the infraorbital rim, and/or midface lift at the time of lower lid blepharoplasty.
While prominent cheekbones are considered attractive, there is lack of anthropometric data to define malar prominence. The only anthropometric landmark for analysis of the malar area is the zygion (Zy), which allows measurement of the bizygomatic distance or width of the midface. Several landmarks lie adjacent to, or involve portions of the malar bone, but there are none defining an area of maximum malar prominence. Thus, malar augmentation is typically determined by the subjective judgment of the surgeon. This can result in patient dissatisfaction, implant asymmetry, and displeasing implant contours.
Several surgeons have suggested different approaches to identify the malar prominence as a guide to malar augmentation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here