Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Adherence to the principles of an airway management algorithm and widespread adoption of such a structured plan should result in a reduction of respiratory catastrophes and a decrease in perioperative morbidity and mortality.
Airway evaluation should consider any characteristics of the patient that could lead to difficulty in the performance of (1) face mask or supraglottic airway (SGA) ventilation, (2) direct or video-assisted laryngoscopy (VAL), (3) intubation, (4) invasive airway access, or (5) extubation.
In the anesthetized patient whose trachea has proved to be difficult to intubate, it is necessary to try to maintain oxygenation by mask ventilation between and during intubation attempts, whenever possible. The use of transnasal humified rapid insufflation ventilator exchange (THRIVE) should be considered when available.
Repeated attempts at difficult intubation (perseveration) can result in serious soft tissue injury and rapidly deteriorate into a cannot intubate/cannot oxygenate (CICO) situation that requires a cricothyrotomy as a potentially lifesaving procedure.
SGA devices are not helpful if there is complete airway obstruction located above, at, or below the glottic opening.
A well-selected number of alternative airway devices and techniques should be available and routinely practiced.
Extubation of the patient with a DA should be carefully assessed and performed, and the anesthesiologist should develop a strategy for safe extubation of these patients.
The presence and nature of the airway difficulty should be documented in the medical record.
Further research should address aspects such as adherence to national and local guidelines in emergency situations, the detailed experience with new and already established airway devices, and the specific role and limitations of new devices as they reach clinical practice.
As difficult airway (DA) guidelines and algorithms will continue to be modified, airway practitioners must keep abreast of new advances in both techniques and theory related to DA management.
The difficult airway (DA) remains one of the most relevant and challenging clinical situations faced by anesthesiologists due to the occurrence of major adverse consequences if airway patency is not established, such as brain injury and death. There is strong evidence that successful airway management in the perioperative environment depends on specific strategies. Suggested strategies from various subfields of medicine are now being linked to form more comprehensive treatment plans or algorithms. Many national anesthesiology societies have developed guidelines for management of the DA that are based on expert opinion and scientific evidence. Algorithms have been developed to assimilate these guidelines in a stepwise fashion to facilitate management of the DA and reduce the likelihood of adverse outcomes. Additionally, efforts are currently underway to develop a universal airway management guideline that can be applied across clinical disciplines, patient types, geographic regions, and contexts of care.
There has been tremendous growth in the literature on management of the DA in anesthesia practice. In order for DA guidelines to reflect the most current evidence, they should be reviewed regularly for their content and continued relevance. Some of the most significant changes in DA guidelines over the past two decades have been the incorporation of new airway devices or techniques. As the practice of airway management becomes more advanced, anesthesiologists must become both knowledgeable and proficient in the use of various airway devices and techniques in both the nonemergent and emergent setting. Nonetheless, there are also nontechnical factors involved when an anesthesiologist is confronted with an unexpected DA in either setting. Anesthesiology as a specialty must address the impact of environmental, technical, and psychological factors on the practitioner’s performance. A better understanding of the human factors involved in a DA crisis is crucial to ensure patient safety, and further research into their role in the cause of airway complications is needed.
The effectiveness of guidelines for airway management in daily practice is not straightforward, as indicated in several outcome studies. One of the largest outcome studies in airway management is the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society (NAP4), which analyzed 2.9 million anesthetics in the United Kingdom. Major complications occurred in 1:22,000 anesthetics leading to an airway-related mortality rate of 1:180,000 cases. However, as the number of cases may have been underreported, the true incidence of severe events might actually have been 4 times higher (∼1:5,500). From a more pessimistic point of view, the estimated number of critical airway incidents (near-misses) that do not lead to actual harm, such as failed intubation with mild or moderate hypoxic episodes, is considerably more common than 1:5,500.
The original Difficult Airway Society (DAS) guidelines were in effect during the time period the NAP4 survey was conducted. Thus, the actual positive impact of the airway guidelines may be questioned. On the other hand, results from the implementation of the guidelines from the American Society of Anesthesiologists (ASA) Practice Guidelines for the Management of the DA and from institutional guidelines suggest that routine application of an algorithmic approach to failed intubation was associated with much higher success rates once implemented. Unfortunately, results of the newest analysis of the Closed Claims Project in the United States with regard to difficult tracheal intubation have yielded worrisome figures as well. Compared to the period from 1993 to 1999, the latest figures from the years 2000 to 2012 show that the incidence of brain damage or death at induction was 5.5 times greater in the latter time period.
When considering the sobering results of the NAP4 study and the recent Closed Claims analysis, perhaps it is the nonobligatory use or the flexibility when using algorithms or guidelines in daily practice that is problematic. In fact, the practitioner may deviate from a predefined plan according to the actual clinical situation. This is very different from civil aviation, where “following the rules” is considered paramount in terms of safety. “The big difference is not so much the safety toolkit, which is similar for most industries,” as Amalberti and colleagues stated, “but in an industry’s willingness to abandon historical and cultural precedents and beliefs that are linked to performance and autonomy, in a constant drive toward a culture of safety.” From this point of view, it is conceivable that the nonobligatory nature to use airway algorithms/guidelines may be partly responsible for the disappointing result of NAP4. Thus, perhaps following such algorithms should be compulsory and considered standard of care, such as the use of basic monitoring (electrocardiography [ECG], pulse oximetry, capnography) when providing general anesthesia, regional anesthesia, or monitored anesthesia care.
The use of algorithms for patient care may be problematic for practitioners because of complexity and information overload, which makes it very difficult to distinguish between relevant and irrelevant information. To aid compliance in adhering to algorithms, flowcharts have been developed and successfully used by a range of practitioners. The classic flowcharts of this nature are the resuscitation algorithms that provide evidence-based guidance during cardiopulmonary resuscitation worldwide, such as the American Heart Association Life Support guidelines. Additionally, cognitive aids are increasingly being used during emergencies and have been demonstrated to improve anesthesia decision making in the DA setting. ,
Further consideration regarding the effectiveness of algorithms should include the quality of the evidence. Just because a guideline or an algorithm claims to be evidence based does not necessarily mean that it provides correct recommendations. On the other hand, if there is a requirement for only strong evidence to manage a DA, a decision may not be made at all. It is sometimes necessary, especially in the area of airway management, to sacrifice internal validity to achieve generalizability. In other words, even though randomized controlled trials provide high-quality evidence, these studies may have only limited relevance in clinical practice. A key question regarding the usefulness of airway algorithm guidelines is whether or not they actually reflect best clinical practice since they are primarily based on experience and expert opinion rather than strong evidence.
Nonetheless, airway guidelines do help guide clinicians and allow the community to improve standards, ensure that certain equipment is available, and ensure that training for the skills and processes required to follow such guidelines are in place. The pros and cons regarding the usefulness of algorithms and guidelines are shown in Table 11.1.
| Pro Arguments | Con Arguments | |
|---|---|---|
| Quality assurance (through activities that are proven to be effective); use in “high-risk” technology; support for rare but critical events , | “Cookbook” medicine; prevents innovation ; “what is best for patients overall may be inappropriate for individuals” | |
| Information and involvement of patients in decision-making by using guidelines | Questionable health effect and questionable sustained effect on long-term behavior | |
| “Use of standards makes sense” | Far away from practice ; risk for overruling | |
| Routine application of institutional guidelines is associated with higher success rates | Questionable effect on outcome because of a lack of obligation | |
| Simple and logical algorithms increase survival | Noncompliance due to information overload and high complexity | |
| Opportunity to improve standards and availability of equipment | Questionable value because guidelines are built on expert opinion and group consensus rather than on hard evidence, and because they are outdated due to a limited lifespan (new evidence, new technologies) , |
In the practice of anesthesiology, guidelines and standards have long been used. For instance, many anesthesia societies have implemented mandatory protocols for perioperative monitoring. , In airway management, numerous flowcharts, guidelines, and algorithms have been developed over time. Theoretically, there are differences between algorithms, guidelines, recommendations, standards, protocols, and so on, but in practice it is difficult to differentiate these terms. Table 11.2 contrasts the definitions and the degrees of obligation of the different terms. The main difference relates to the degree of obligation of the practitioner, which means that standards—such as the use of ECG, pulse oximetry, or capnography for monitoring purposes—are obligatory, whereas all others (algorithms, guidelines, protocols, etc) are, strictly speaking, voluntary. , Nonetheless, in the courtroom when there is an airway mishap, these terms are often used interchangeably.
| Terms | Definition | Degree of Obligation |
|---|---|---|
| Standards | Generally accepted principles for patient management; exceptions are rare and failure to follow is often difficult to justify | Mandatory |
| Strategy | A well-planned series of steps for achieving a goal | Voluntary |
| Guidelines | Systematically developed statements to assist the practitioner in specific clinical circumstances; incorporates the best scientific evidence with expert opinion | Voluntary |
| Practice policies | Describe present recommendations issued to influence practitioners in reaching decisions about interventions | Voluntary |
| Recommendations | Suitable and useful strategies; not as strict as standards and guidelines | Voluntary |
| Options | Different possibilities are available; neutral assessment | Voluntary |
| Protocols/Algorithms | Stepwise procedures or decision trees to guide the practitioner through the diagnosis and treatment of various clinical problems | Voluntary |
Many national anesthesia societies have published their own guidelines for management of the DA, including the ASA, the DAS of the United Kingdom, the Canadian Airway Focus Group (CAFG), , the Italian Society for Anesthesia Analgesia Resuscitation and Intensive Care Medicine (SIAARTI), the French Society of Anesthesia and Intensive Care (SFAR), the German Society of Anesthesiology and Intensive Care Medicine (DGAI), the Chinese Society of Anesthesiology, the Japanese Society of Anesthesiologists, and the All India Difficult Airway Association (AIDAA).
Similar to the ASA’s DA guidelines, the CAFG, SIAARTI, and AIDAA guideline methodologies include a systematic review of the literature with classification of the level of evidence. Guidelines published by the other national societies include literature reviews but do not aggregate and classify evidence in a systematic fashion. The DGAI’s guidelines grade the organization’s statements into “strongly recommend,” “recommend,” and “unclear recommendation.” With the exception of the DAS and the AIDAA guidelines, which only focus on the management of unanticipated difficult intubation, all other national guidelines also include recommendations for management of the anticipated DA.
All national societies regard awake flexible scope intubation (FSI) as the technique of choice to manage the anticipated DA, and all societies have incorporated cricothyrotomy for management of a “cannot intubate/cannot oxygenate” (CICO) scenario.
Thus, training and subsequently retaining skills with these techniques remain crucial. This has been impressively confirmed by the recent Closed Claims analysis of the United States. One of the modifications is the addition of video-assisted laryngoscopy (VAL). However, there is still debate as to whether VAL should be a routine, first-line technique or whether it should be reserved for those patients who are predicted or found to be difficult to intubate. , Even though there is a range in the various guidelines for the number of intubation attempts, most algorithms strictly limit the number of intubation attempts to a maximum of three attempts. Many guidelines place increased emphasis on communication (e.g., declaration of failure), situational awareness, strategy, and planning, rather than on tools and devices, which is regarded as an important step toward the improvement of safety. , ,
The ASA Task Force on Management of the DA developed the original ASA Difficult Airway Algorithm (DAA) over a 2-year period. The task force included both academic and private anesthesiologists and a statistical methodologist. This algorithm was introduced by the ASA as a practice guideline in 1993. In 2003, the ASA Task Force presented a revised algorithm that essentially retained the same concept but recommended a wider range of airway management techniques than was previously included, based on more recent scientific evidence and the advent of new technology. In 2013, this revised algorithm was further modified, taking into account additional updated evidence obtained from scientific literature and technology since the last revision and findings from new surveys of expert consultants as well as randomly selected ASA members. ,
The ASA DA guidelines were most recently revised and published in 2022 ( Fig. 11.1 ) . Their intended use has now broadened to all airway management and anesthetic care delivered in inpatient (e.g., perioperative, nonoperating room, emergency department, and critical care settings) and ambulatory settings (e.g., ambulatory surgery centers, office-based surgery, and procedure centers performing invasive airway procedures) and applies to anesthesiologists and all other practitioners who perform anesthesia care or airway management. As in the past, the guidelines are intended for all patients with either an anticipated or unanticipated DA, including but not limited to obstetric, intensive care, and critically ill patients. Of note, the 2022 ASA DA guidelines include separate DA algorithms for adult and pediatric patients, and each algorithm is accompanied by an infographic that can be utilized in real time or for educational purposes.
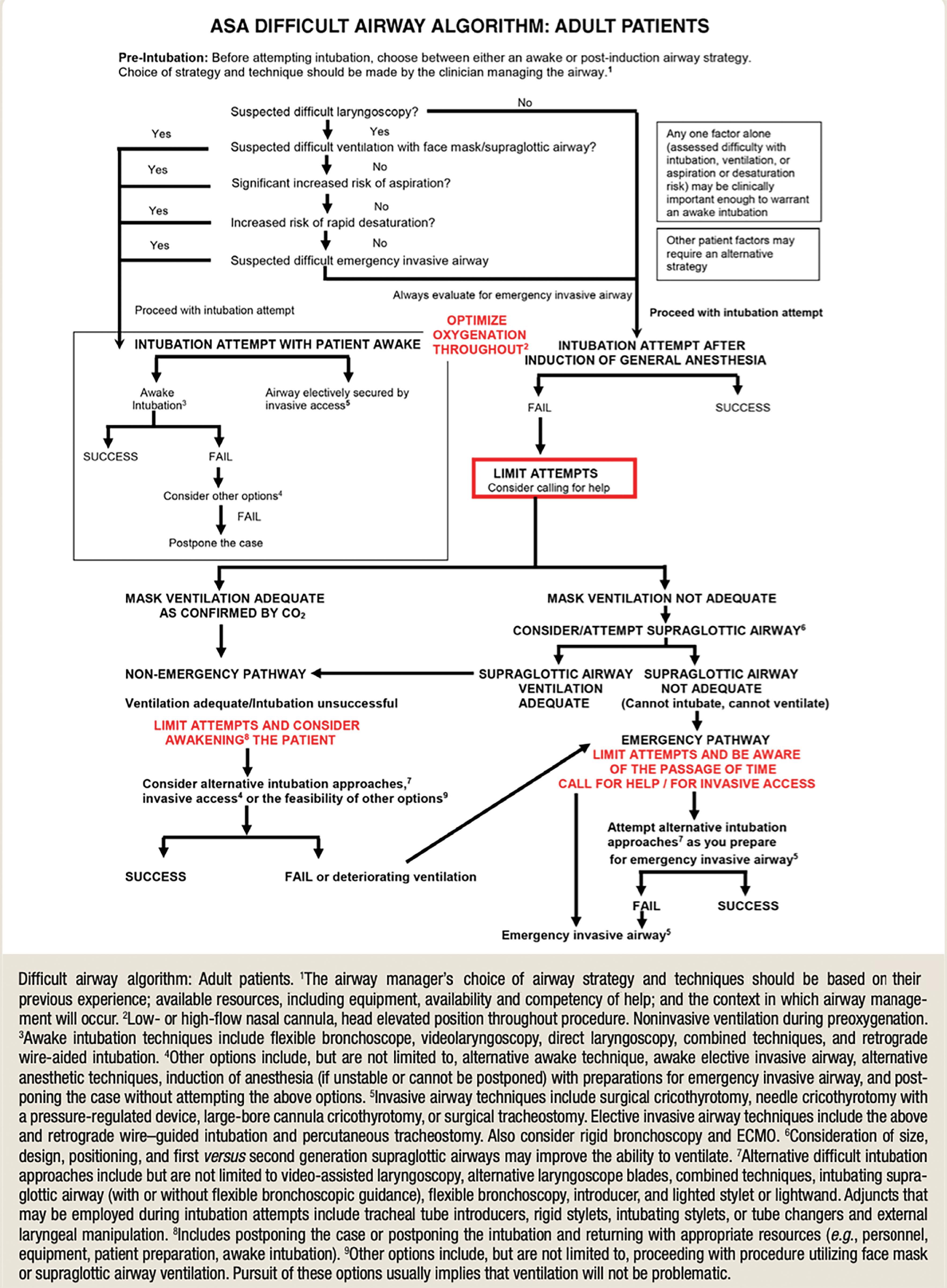
The 2022 ASA DA guidelines for adult patients differ from the 2013 DA guidelines in the following significant ways:
Developed by an international task force of anesthesiologists representing several anesthesiology, airway, and other medical organizations;
Broadens the intended use of the guidelines to all individuals who perform anesthesia care or airway management, both anesthesiologists and non-anesthesiologists;
Provides considerations for the development of a difficult airway management strategy, including considerations for awake airway management and assessments to predict risk of aspiration;
Provides guidance for entering the awake intubation vs. airway management after the induction of anesthesia pathways based on assessment particular to the airway practitioner, context, and resources;
Provides recommendations for managing failure in the awake intubation pathway;
Broadens its descriptions of the difficult airway to include inadequate ventilation, difficult or failed tracheal intubation, extubation of the difficult airway, and difficult or failed invasive airway;
Recommends optimization of oxygenation before initiating and throughout difficult airway management, including the extubation process;
Specifies limiting initial attempts at intubation, limiting intubation attempts if ventilation is adequate but intubation is unsuccessful, and limiting attempts at placing an SGA in a “cannot intubate, cannot ventilate” scenario;
Explicitly mentions awake intubation techniques, such as flexible bronchoscopy or combination techniques;
Provides an opinion-based recommendation to limit attempts at laryngoscopy and intubation or SGA attempts to three, with one additional attempt by a clinician with a high skill set;
Broadens noninvasive and invasive alternatives for difficult airway management to include the use of combination techniques, rigid bronchoscopy, and extracorporeal membrane oxygenation;
Provides updated recommendations for the contents of a portable storage unit, as well as recommendations for airway management items in all anesthetizing locations;
Provides more robust recommendations for precautions during extubation of the difficult airway and additional recommendations for follow-up care;
Includes consideration of human factors (including environmental factors, team behaviors, and individual performance) as part of airway preparation, management, and post-event airway care;
Provides new algorithms and infographics for adult and pediatric difficult airway management.
Unlike the ASA DA guidelines, which address both the anticipated and the unanticipated DA, the DAS guidelines focus on the unanticipated DA, an unpredictable problem. The new 2015 DAS guidelines differ from the original 2014 DAS DA guidelines in that they are more concise and more pragmatic, with considerable emphasis placed on preparedness and accountability of the practitioner, by optimizing conditions and minimizing patient morbidity in a DA situation ( Figs. 11.2 – 11.4 ). Training of physicians with alternative airway devices and techniques, including emergency invasive airway access, is considered not only essential but expected.
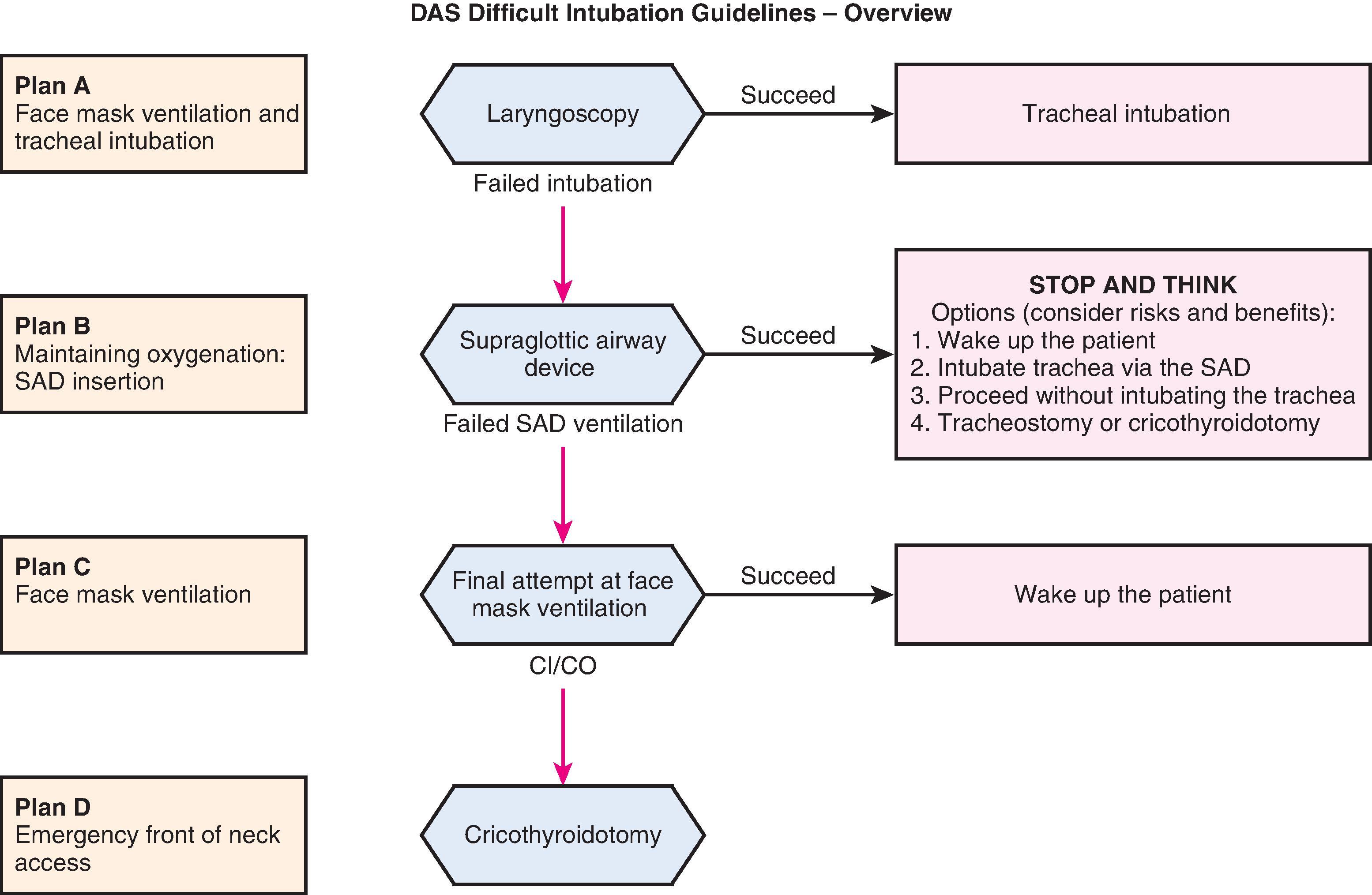
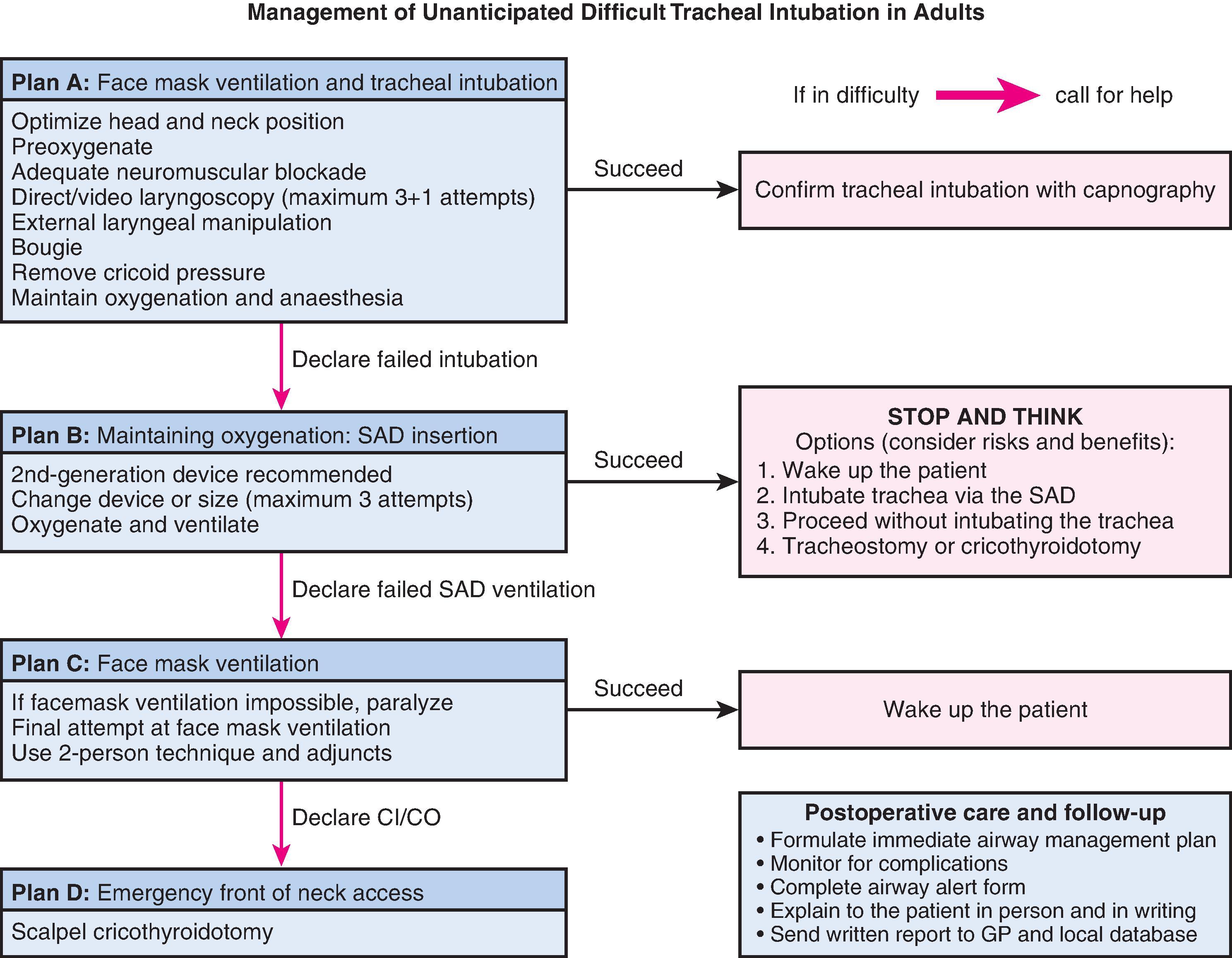
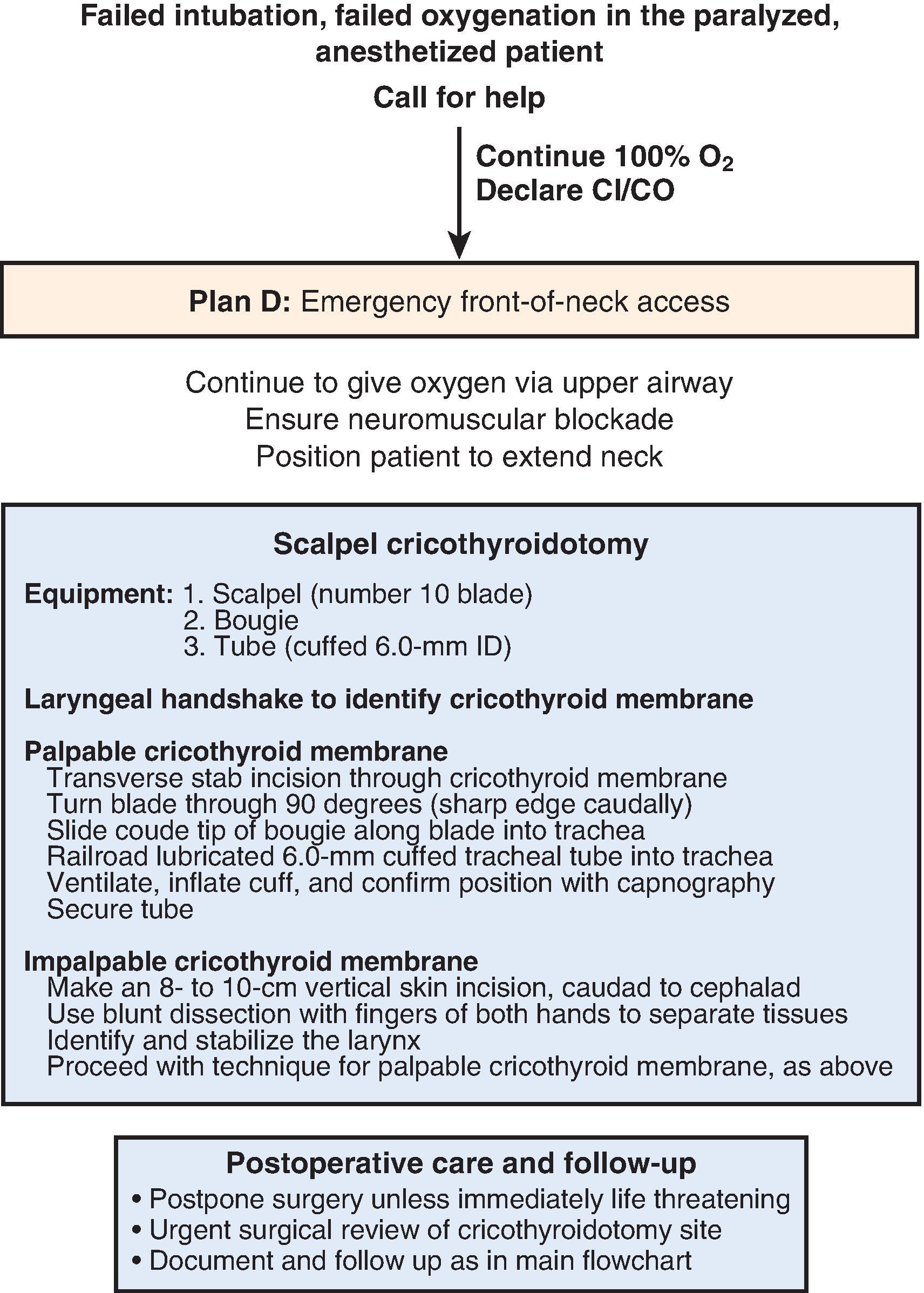
After an unsuccessful initial intubation attempt, restoration of ventilation is the priority, by either noninvasive (e.g., SGA) or invasive intervention, or by awakening the patient. Repeated attempts at intubation should not delay noninvasive airway ventilation or emergency invasive airway access. The new guidelines favor the use of second-generation SGAs in this situation, because they have specifically designed features to reduce the risk of aspiration and provide a better airway seal. Similar to recommendations by other national societies, the new guidelines incorporate the use of VAL for management of the DA. Although all anesthesia society guidelines incorporate the performance of a cricothyrotomy for management of the CICO situation, the new DAS guidelines no longer recommend the cannula technique, due to the findings from the NAP4 study that this technique was inferior to the surgical technique. The new guidelines recommend consideration of the technique of nasal oxygen during efforts securing a tube (NO DESAT) and transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) to relieve the time pressure of falling oxygen saturations during the decision-making process.
The new DAS DA guidelines provide valuable consensus from an expert panel that has drawn extensively on the experience of international experts. Nonetheless, they emphasize human factor issues at individual, team, and organizational levels for their optimization. They provide a structured approach to a potentially life-threatening clinical situation and consider current practice and recent developments. They do not constitute a minimum standard of practice, nor should they be regarded as a substitute for good clinical judgment. Separate DAS guidelines exist for pediatric and obstetric patients, for extubation of the DA, and for management of tracheal intubation in critically ill adults as well.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here