Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Of all the components of our face, it is our eyes that define us. When the eyes and the orbits no longer have symmetry, the asymmetry involves the frontal region superiorly and inferiorly to the midface and the lower face as well. In addition to symmetry, the position of the orbits relative to each other and relative to the dominant central feature, the nose, often affects whether the face is perceived as normal or not. Equally, the position of the ocular globe relative to the skeletal framework of the bony orbit defines normality.
Of all the surgical procedures that require facial reconstruction, the hardest to master is the restoration of the human orbit because it involves (1) normalizing the position of the ocular globe within its skeletal orbital framework; (2) establishing orbital symmetry with its counterpart in all their planes (coronal, sagittal, and transverse); (3) positioning the orbits within normative facial proportions; and (4) finally, restoring the “normal anatomy” of the nose because it defines the mirror image line of symmetry. It is only after orbital symmetry and proportions are established that the remaining facial surgery (mid- and lower face) can be appropriately executed by using the orbit (horizontal axis) and the nose (vertical axis) as the reference axes.
The orbit is defined by seven bones: zygoma, maxilla, sphenoid, ethmoid, palatine, lacrimal, and frontal bones. Its overall shape approximates a “pyramid” with a rectangular base as the orbital rim and the apex as the optic foramen.
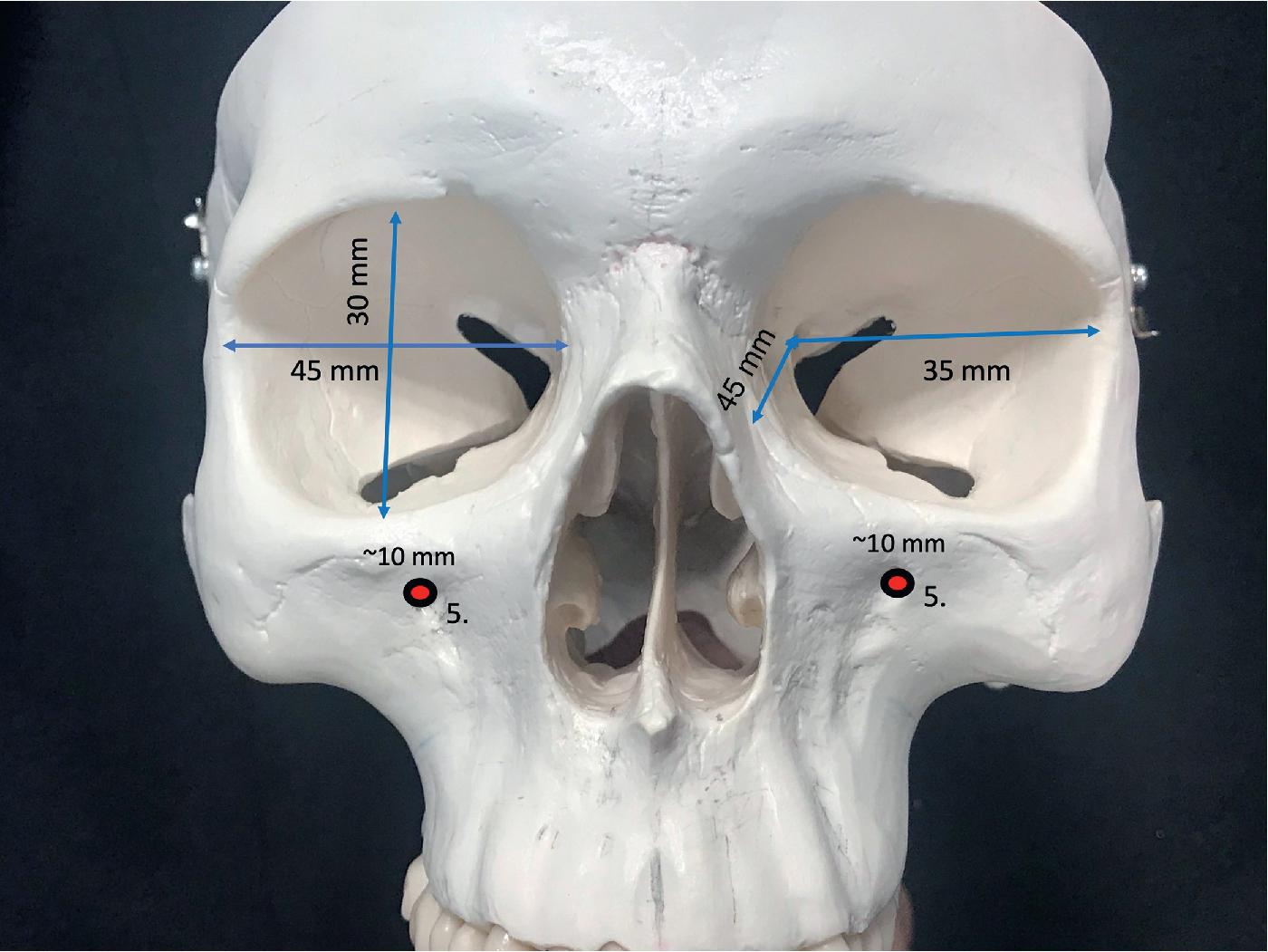
Although the orbit has a range of dimensions, it is important for the surgeon to have an understanding of approximate distances and angles that will be relevant for surgical planning and intraoperative guidance to critical landmarks ( Fig. 33.1 ). The orbital rim measures approximately 40 mm in length and 35 mm in height and has a lateral rotation in the transverse plane. From the medial orbital rim to the orbital apex, the depth of the pyramid is approximately 45 mm. From the lateral orbital rim to the orbital apex, the depth measures approximately 35 mm. The orbit expands at its widest circumference approximately 10 mm behind the orbital rim at the lacrimal recess. In the transverse plane, the medial orbital walls are parallel to the midsagittal plane, and the lateral orbital wall is approximately 45 degrees. Thus the left and right lateral orbital walls form a 90-degree angle. This lateral rotation places the lateral orbital rim approximately at the globe equator, exposing the eye. The medial orbital walls are separated by the paired medial ethmoid sinuses, and distance between the medial orbital walls is approximately 25 mm. The orbital volume is approximately 30 mL, and the volume of the globe that occupies it is approximately 7 mL.
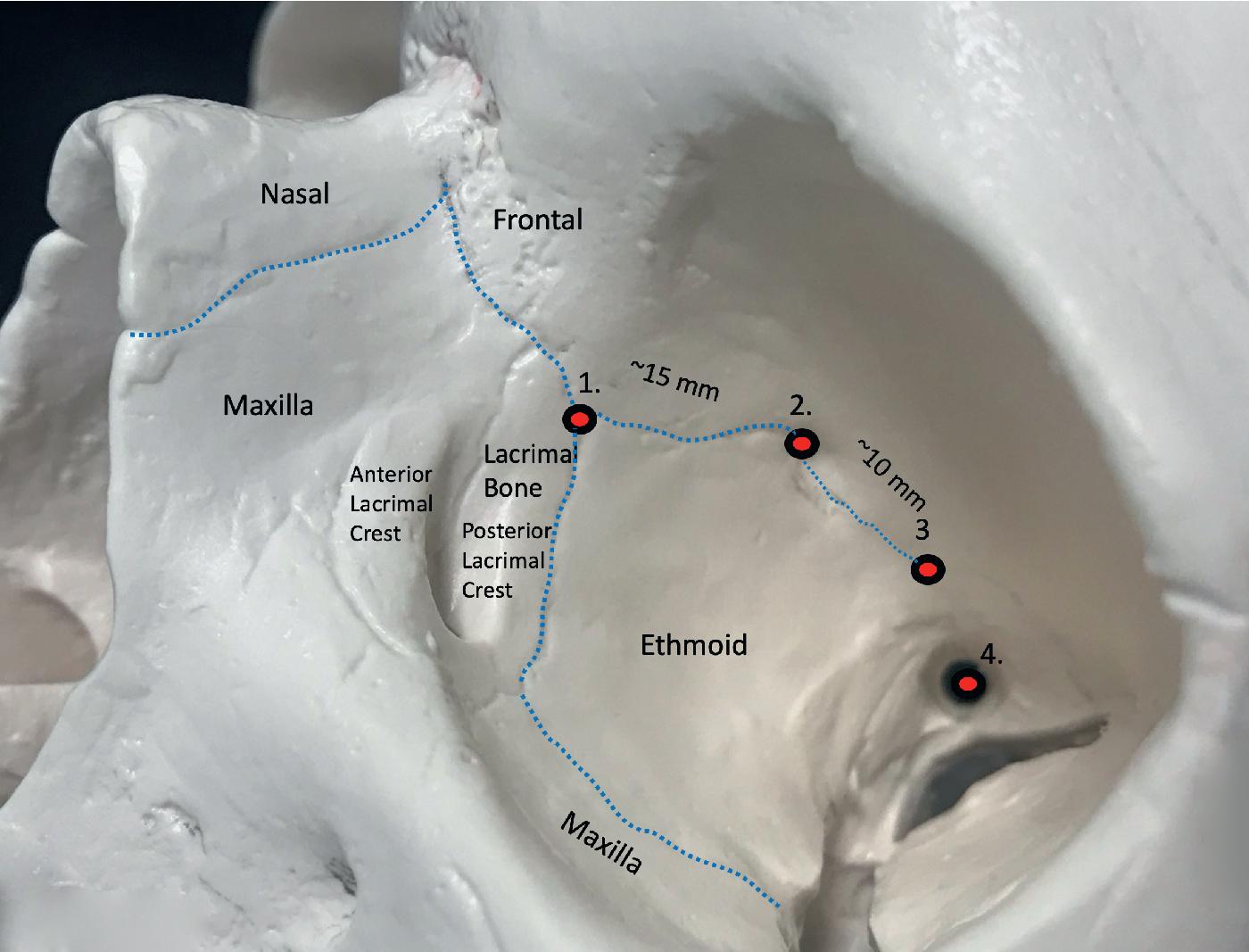
The medial orbital wall extends from the anterior lacrimal crest to the orbital apex. The anterior edge is demarcated by the lacrimal fossa, defined by the thick anterior and posterior lacrimal crest into which the medial canthal ligaments insert. Thereafter, the thin lamina papyracea separates the ethmoid sinus from the orbital contents. The medial orbital wall’s posterior edge is demarcated by the thick sphenoid bone that contains the optic canal. The area between the posterior lacrimal crest and the sphenoid, the lamina papyracea, is sectioned/fractured for the decompression procedure or for the medial wall osteotomy in translocation. The medial orbital wall’s upper edge is defined by the frontoethmoid suture that separates the intracranial cavities from the extracranial cavities. The anterior and posterior ethmoid foramen, through which the respective vessels course, are the intraoperative anatomic landmarks useful for the surgeon to visualize for the level of the osteotomy if the planned procedure is to remain subcranial ( Fig. 33.2 ). The vessels should be electrocauterized to prevent postoperative epistaxis and the foramen marked. Violation of the frontal bone via an orbital osteotomy above this suture carries the risk of cerebrospinal fluid leakage due to exposure of the dura of the frontal lobe.
The medial canthus consists of a tendinous attachment of the orbicularis oculi muscle and a ligamentous attachment to the tarsus. The attachment is primarily at the anterior lacrimal crest, which is located on the frontal process of the maxilla. The posterior or minor contributor to the attachment is the posterior medial canthus, known as the pars lacrimal muscle or Horner muscle. This posterior limb also represents the attachment of the orbicularis oculi muscle to the posterior lacrimal crest. The lateral canthus can be reliably resecured, but restoring the medial canthus can be problematic, and recreating the aesthetic position and contours of a natural medial canthus can be difficult if it becomes detached during the course of the procedure. Once detached, canthal symmetry between the left and right medial canthus is difficult to achieve. Any discrepancy in the medial contours and a difference in position that exceeds 2 mm are noticeable because of their proximity to one another.
Located between the lacrimal bone and wedged between the anterior and posterior tendons is the nasolacrimal canal. Just above the canal is the lacrimal sac, which receives contributions from the lacrimal canaliculi to the nasolacrimal duct (see Fig. 33.2 ). The nasolacrimal duct courses within the inferomedial orbital wall from the lacrimal crest to its opening beneath the inferior nasal concha. The periorbital osteotomy must be posterior to the lacrimal crest and inferior to the turbinate to avoid injuring the nasofrontal duct. In some instances, placing a nasofrontal duct stent just before the osteotomy can be beneficial if there is potential risk to the duct.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here