Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Most foreign bodies occur in boys under the age of 3. Common airway foreign bodies are peanuts, seeds, and vegetable matter. Most common esophageal foreign bodies are coins and pins.
A reliable history and a witnessed aspiration or ingestion are the most important factors in diagnosing an aerodigestive foreign body. Esophageal foreign bodies are twice as common as bronchial foreign bodies, but most of these pass on to the stomach and do not necessarily require removal.
Frontal and lateral radiographs are helpful as initial radiographic studies of choice, but false-negative imaging is not uncommon. Classically, coins appear with a single rim on radiography, whereas button batteries have a double rim or “halo.”
A reasonable suspicion of an airway foreign body mandates an urgent bronchoscopy, whereas esophageal foreign body removal depends on the timing of ingestion, location, and type of object.
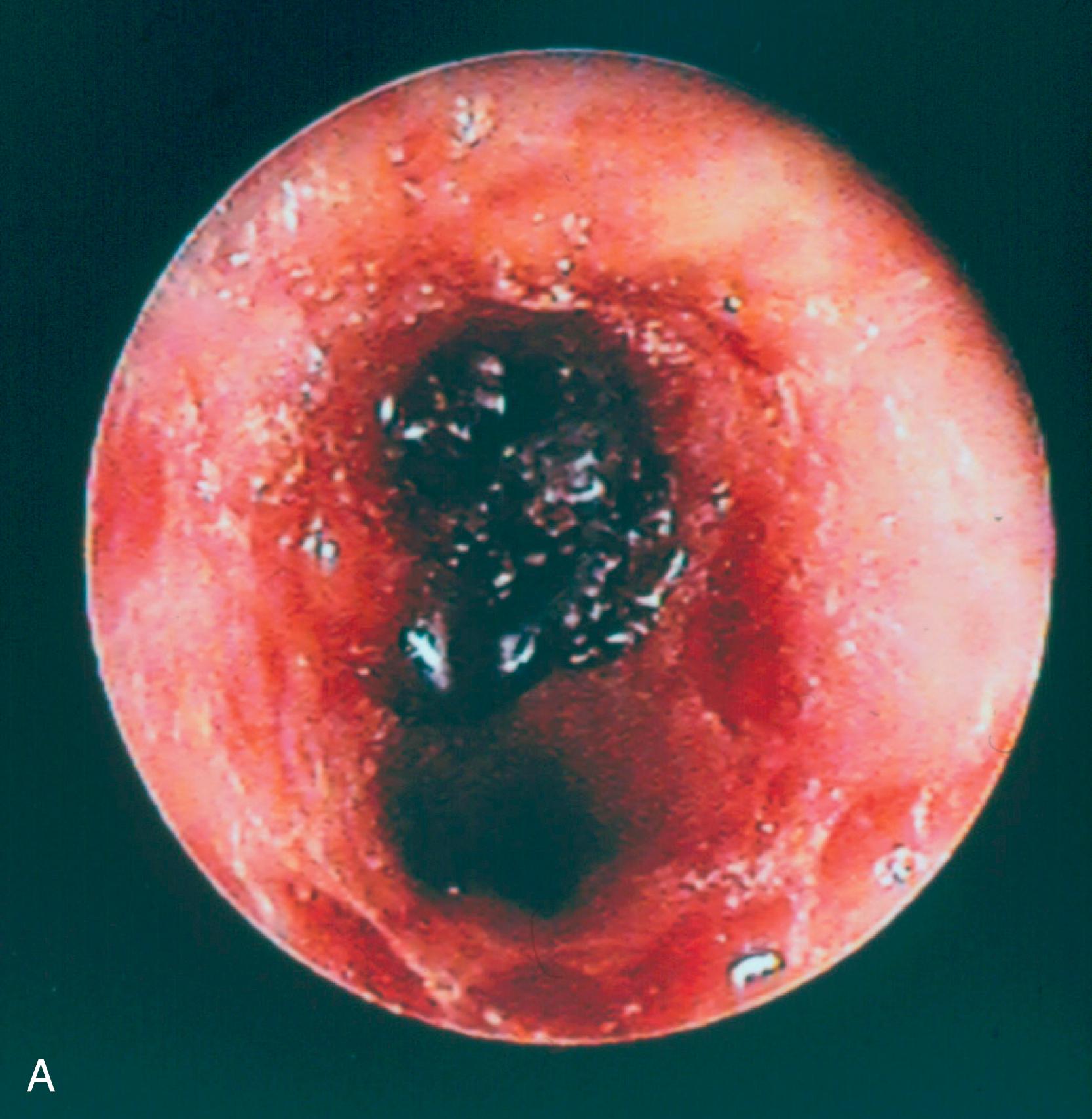
Intentional caustic ingestion typically leads to severe injury and death.
The presence or absence of oropharyngeal burns is not a predictive of esophageal injury. Endoscopy should be performed on a case-by-case basis.
Steroids are of unproven benefit in the treatment of caustic esophageal burns.
The late complications of caustic injury to the aerodigestive tract can manifest days to weeks later. A repeat radiographic or endoscopic examination is important to rule out permanent damage. Caustic ingestion may lead to carcinoma.
Aerodigestive foreign bodies and caustic ingestion are important causes of morbidity and mortality in the pediatric population. Aerodigestive foreign bodies account for approximately 150 pediatric deaths each year and 12,000 emergency department visits annually. Caustic ingestions are estimated at 250,000 annually. Choking accounts for 40% of all deaths in children under the age of 1. Foreign bodies and caustic ingestions present diagnostic challenges, as their presentation can vary from life-threatening airway compromise or sepsis caused by intestinal perforation to subtle symptoms that are often misdiagnosed. A high level of clinical suspicion can prevent delays in diagnosis and subsequent complications. This chapter will discuss the workup and treatment of aerodigestive foreign bodies and caustic ingestions.
Prevention is the most important intervention to reduce morbidity and mortality from aerodigestive foreign bodies and caustic ingestions. The 1979 Consumer Product Safety Act specified criteria for the minimum size of children’s toys to reduce the risk of foreign body ingestion or aspiration, but these regulations are not uniformly enforced. Objects must be less than 3.17 cm in diameter and less than 5.71 cm in length to be allowable for children; if an object can fit within the Small Parts Test Fixture (SPTF), it is considered a small part. Because the shape of a ball increases risk of ingestion or aspiration, balls are held to an even stricter standard, namely 1.75 inches or greater for children under 3 years of age. , Some suggest that adoption of even stricter dimensions for the small part cylinder (SPC) used to define potential choking hazards could potentially prevent at least 20% of the injuries and fatalities resulting from foreign body ingestions and aspirations in children.
The Consumer Product Safety Improvement Act of 2008 amended the Federal Hazardous Substance Act (FHSA) to include choking-hazard warnings in all media (e.g., websites and catalogs). In addition, for all toys intended for children under 3 years old, the batteries are required to be secured in compartments with screws. Unfortunately, manufacturers of routine household products are not held to those same safety standards. Battery manufacturers have not been able to redesign the 3.0-V lithium battery to provide the same shelf life and output while reducing the powerful electrical current discharge into living tissues. Ideally, manufacturers would be able to provide secure compartments and child-resistant packaging for all devices using lithium batteries. Individual wrapping of batteries is crucial; when multiple batteries are packaged together, removing one battery leaves the remaining batteries within easy reach of children for accidental ingestion.
In 2010 an American Academy of Pediatrics policy statement recommended that the U.S. Food and Drug Administration (FDA) establish a system of evaluating foods and providing warning labels for those foods that pose a high choking risk. General recommendations also encourage the training of health care and non–health care providers that interact with children regarding the signs of foreign body ingestion and resuscitative measures.
Although these laws and regulations may help prevent aerodigestive foreign bodies or caustic ingestions, the most important public health intervention is parental counseling. Public campaigns of the inherent dangers of common household items containing button batteries will also help raise awareness. Children should be seated and always supervised while eating. They should be encouraged to thoroughly chew their food into small pieces prior to swallowing and should be frequently reminded not to laugh or talk while eating. These recommendations are particularly pertinent for children with esophageal motility disorders or neurologic disorders, as they are at increased risk for choking. Small and hazardous objects should be safely stored so as not to be accessible to a newly mobile and curious child ( Box 34.1 ). Parents can purchase a small parts cylinder and test toys to ensure they are not too small.
Balloons
Button batteries
Coins
Marbles
Toys with small parts
Toys that can be squeezed to fit entirely into a child’s mouth
Small balls
Pen or marker caps
Medicine syringes
Single-use laundry detergent pods
Those clinicians familiar with the management of corrosive and caustic injury clearly understand the limitations of management and fully appreciate the need for preventative strategies in education, product labeling, and legislation to promote public safety to limit ingestion of these dangerous products.
Bronchotomy for foreign body retrieval was first described by Verduc in 1717. In 1854 the first study profiling and describing hundreds of cases of airway foreign bodies was published, advocating bronchotomy for any patient with symptoms of foreign body aspiration. However, given that bronchotomy had a higher mortality rate than observation (23%), bronchotomy then became reserved for severely ill patients at risk of imminent death. Killian demonstrated successful foreign body removal by passing a 9-mm endoscope into the bronchus. In 1905 Chevalier Jackson reported the removal of foreign bodies from the bronchi. Jackson ultimately designed, developed, and greatly improved instrumentation and brought laryngoscopy and bronchoscopy to its present state. He is well-deservedly considered the father of endoscopic aerodigestive foreign body removal.
Chevalier Jackson was also instrumental in the passage of the Caustic Act of 1927, which called for labeling of lye and 10 other caustic chemicals. After introduction of liquid lye products in 1967, the Poison Prevention Packaging Act of 1970 mandated childproof containers and restricted the concentration of liquid products to <10%. The Poison Prevention Packaging Act of 1970 also established the Consumer Product Safety Commission (CPSC). The National Poison Control Center was founded in 1980 and since then has served as an indispensable source of information for medical professionals and consumers on product composition, toxicity, and treatment; the 24-hour National Poison Control Hotline number is (800) 222-1222. In 1982 the CPSC mandated tamper-resistant packaging to further reduce inadvertent ingestion by children. The National Battery Ingestion Hotline number is (800) 498-8666.
Aerodigestive foreign body ingestions and aspirations occur more commonly in boys and in children under the age of 3 years. The high incidence of aerodigestive foreign bodies in children of this age is likely related to their increased mobility and their tendency to play and eat at the same time. Young children lack cognitive recognition of edible versus inedible objects, which contributes to their high propensity for placing objects in the mouth. In addition, they have incomplete molars that make chewing difficult, and an immature and underdeveloped ability to swallow. The most commonly aspirated foods in young children are listed in Box 34.2 .
Hot dogs
Nuts and seeds
Chunks of meat or cheese
Whole grapes
Hard, gooey, or sticky candy
Popcorn
Chunks of peanut butter
Raw vegetables
Fruit chunks, such as apple chunks
Chewing gum
Fortunately, most foreign bodies are expelled immediately by protective cough and spitting reflexes. Inhaled foreign bodies more commonly include organic materials such as nuts, seeds, vegetable matter, or dried fruits ( Fig. 34.1 ). , , , When aspirated, they frequently become lodged in the bronchial tree, with the right main bronchus being more common because of its wider lumen and more vertical path.
Esophageal foreign bodies are twice as common as bronchial foreign bodies, but most of these pass on to the stomach and do not necessarily require removal. , Between 10% and 20% of esophageal foreign bodies that come to medical attention require endoscopic removal, and less than 1% require an open operative intervention such as a thoracotomy. Foreign bodies are most likely to become lodged in the stomach (60%) followed by the esophagus (20%), oropharynx (5% to 10%), and intestines (10%). Coins and pins are the most commonly ingested items ; other common items include batteries, toy parts, bones (e.g., fish, chicken), and jewelry. , Food bolus impaction is uncommon in the pediatric population but can occur in children with eosinophilic esophagitis, esophageal strictures from esophageal atresia repair, or prior Nissen fundoplication. Magnet ingestion, particularly those composed of rare earth metals (e.g., neodymium, iron, and boron) should also warrant urgent evaluation and intervention. Single magnets can often be asymptomatic and pass without further complications. However, if multiple magnets or a combination of a magnet or metallic object is ingested, urgent management may be necessary to prevent significant sequelae such as intestinal perforation, volvulus, fistula, and sepsis. Fortunately, mortality is rare in foreign body accidents.
Button battery ingestions are responsible for more than 90% of major morbidity and mortality from foreign body ingestion since 2000. Ingestion injuries to children caused by batteries have been reported in the medical literature and by poison control centers for several decades. Since 2006, approximately 3500 battery ingestions are reported each year. Alkaline cylindrical batteries such as typical household AA or AAA batteries pass through to the stomach without injury to the esophagus. In contrast, button batteries are composed of several different chemical types, such as manganese dioxide, zinc air, silver oxide, mercuric oxide and lithium. Although lithium batteries represent only 18.6% of all ingested button cells, the vast majority of major injuries and deaths result from ingestion of the commonly used 3.0-V, 20 mm diameter lithium batteries. These cells have become so pervasive in our daily use that literally every household with children has multiple opportunities for unsupervised ingestion. The National Poison Control Center reported that from January 2009 to June 2012, the most common household items with ingested 20-mm lithium batteries were remote controls, games/toys, watches/stopwatches, and candles. Common myths still prevail ( Box 34.3 ). A study in 2018 suggest that early ingestion of sucralfate and honey may be of benefit to slow down tissue injury until battery removal can be achieved.
Dead batteries cannot cause injury. Even though a battery is no longer capable of powering a device, it still has enough current to cause esophageal injury.
The battery leaches caustic or corrosive fluid into the esophagus. The battery compartment remains intact. Injury occurs because of the powerful electrical current that discharges into the moist tissues, causing hydrolysis and injury.
Singing/musical greeting cards are dangerous. The greeting card industry addressed this problem several years ago. A few manufacturers abandoned use of lithium batteries and reintroduced alkaline batteries. Others have secured the battery compartments making it very difficult to pop out the battery.
Single-use laundry detergent pods (SULDPs), such as the popular detergent brand Tide Pods, are single-use packages containing concentrated liquid detergent within plastic wrapping that dissolves in contact with water, created as an alternative to powder or liquid-only detergents for laundry use ( Fig. 34.2 ). They were introduced in the U.S. market in 2010 after being commercially available in Europe a decade before. However, like any household cleaning product, SULDPs can be a safety hazard, particularly for children. Approximately 95% of SULDP ingestions are accidental or exploratory, occurring in children under the age of 5 years, and they are related to brightly colored packaging that may resemble candy or toys. Adult ingestion is nearly always intentional and accounts for less than 1% of exposures.

Between 2012 and 2013, more than 17,000 cases of exposures among children in the United States were reported by the United States Poison Control Center. In California alone, during a 14-month period from 2012 to 2013, there were 804 reported cases. Furthermore, the ubiquity of social media necessitates that health care providers understand the risks of SULDP to the upper aerodigestive tract. The “Tide Pod Challenge,” promoted among young adults, encourages the participant to bite into a laundry detergent pod or cook the pod before biting into it, to produce the effect of foaming at the mouth. The American Association of Poison Control Centers (AAPCC) reported 39 cases of intentional exposures among adolescents of this age in 2016 and 53 cases in 2017.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here