Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
For both primary and metastatic brain tumors, radiation therapy (RT) remains one of the standard treatment modalities. Although RT techniques using photons have greatly improved in recent decades, substantial concerns remain among both physicians and patients regarding the potential for long-term side effects after RT to the brain.
Adverse effects after RT to the brain are numerous. In consenting when patients give consent for therapy, potential damage to specific structures such as the optic chiasm, optic nerves, or spinal cord is often cited, which could result in vision impairment, paralysis, and so on. Thankfully, such side effects are relatively infrequent. However, subtler long-term side effects may be problematic for both patients and their families. This includes the potential for long-term cognitive deficiencies. Although deficits in memory formation are the most commonly studied in the field of radiation oncology, deficits in attention or other executive functions may be equally as debilitating. Remarkably little is known regarding the biological basis for the side effects. However, progress is being made in the pharmacologic prevention of side effects and with use of advanced photon techniques, such as hippocampal-sparing intensity-modulated RT (IMRT). Proton therapy may offer much greater normal tissue sparing and thereby further decrease the incidence of the side effects.
Particle therapy, including proton therapy, is hoped to expand the therapeutic index of radiation for primary brain tumors. Unlike photons, as the proton beam passes through tissue, protons continuously slow down, and the rate at which they deposit dose increases along their path. The point at which all energy is depleted is termed the Bragg peak. Past the Bragg peak, virtually no extra dose is delivered, and hence, normal tissues distal to the target should receive virtually no radiation exposure. Based on these principles, assuming target volumes are adequately covered, RT with protons should offer equivalent disease control but with superior normal tissue sparing and hence a reduction in long-term adverse effects.
Presently within the United States alone, nearly 30 proton centers are in operation, with many more in the planning or development stage. Although proton therapy has been used in the treatment of a variety of primary brain tumors, no published randomized studies exist to document its clinical superiority in comparison with advanced photon techniques. In the setting of increased scrutiny from insurance providers, this may limit patients’ access to proton therapy. In this review, we highlight the technologies used to deliver proton therapy as well as preliminary clinical studies of primary brain tumors, including gliomas, meningioma, and others. Finally, areas for additional study, including the use of advanced treatment planning techniques, are offered.
Gliomas have a broad spectrum of disease types with associated differences in outcomes. Our understanding of the molecular profiles of these tumors continues to evolve rapidly and is now informing us which patients may achieve long-term survival. Mutational profiling is now the standard of care for lower-grade gliomas, including the World Health Organization (WHO) grades II and III. Broadly speaking, patients may be grouped as those having or not having mutations in isocitrate dehydrogenase (IDH). Although a descriptor of grade II or III may be assigned by pathologists, evidence suggests little difference in outcomes based on grade, but the presence of an IDH mutation indicates favorable prognosis. , Conversely for patients with grade II or III tumors where no IDH mutation is identified, these tumors may be classified as a “molecular glioblastoma (GBM),” and patients may experience rapid disease progression similar to that seen with grade IV GBM.
RT has an integral role in the treatment of low-grade gliomas, and although mutational status is now influencing therapeutic decisions, historically, treatment decisions have been based on tumor grade. For WHO grade II gliomas, combined-modality therapy has contributed to improved survival rates, and early RT is associated with improved progression-free survival. , However, the timing of RT that is, whether it is delivered as adjuvant or salvage therapy, remains controversial. The existing controversy centers on the negative effects of radiation on cognitive function and quality of life, which are of special importance in patients with a long life expectancy. For patients with WHO grade III tumors, adjuvant RT is considered standard, although, as noted, mutational profiling allows the prediction of favorable outcomes for subsets of patients. In particular, grade III gliomas with an IDH mutation have favorable outcomes, and numerous patients will achieve long-term survival similar to that seen for patients with WHO grade II tumors. , , As such, these patients are at substantial risk for cognitive decline after RT.
Cognitive decline after cranial irradiation is especially problematic for brain tumor survivors, as it is associated with reduced quality of life. , Historically, the overwhelming majority of radiation treatments have been delivered using photon-based techniques. Douw et al. retrospectively evaluated patients with low-grade gliomas treated with or without RT and found RT use to be associated with impaired attentional functioning and executive function. Gondi et al. prospectively evaluated the effects of radiation on cognitive function in adult patients with low-grade brain tumors treated with advanced photon radiation techniques, including IMRT. The trial included both baseline and postradiotherapy assessments including formal neurocognitive tests. Exposure of the bilateral hippocampi to doses as low as 7.3 Gy was associated with long-term memory impairment.
Such evidence has led practitioners to believe that proton therapy may be ideally suited for the treatment of these tumors. In addition to compelling dosimetric studies, initial clinical studies of proton therapy have suggested efficacy. Investigators from Massachusetts General Hospital (MGH) first used mixed photon/proton treatments for dose-escalation studies including patients with WHO grades II and III gliomas. Investigators from the University of Heidelberg, which uses scanning beam proton delivery technology, have also reported on 19 patients treated for low-grade gliomas. Similar to photon-based treatments, their initial results suggest high rates of tumor control and acceptable toxicity rates. The group at The University of Texas MD Anderson Cancer Center has also reported on outcomes after IMRT or proton therapy for these tumors. Although the latter was a retrospective study, disease control outcomes were similar. However, patients with oligodendroglioma treated with protons developed pseudoprogression sooner than those treated with photons. Formal cognitive testing outcomes were unfortunately not available. In a recent study, Shih et al. reported results of a prospective trial that enrolled patients with grade II gliomas. In addition to reporting excellent disease control rates, they assessed cognitive function and quality of life after proton therapy. Twenty patients, all with supra-tentorial tumors, were enrolled. With a median follow-up time of 5.1 years, measures of cognitive function were stable to improved relative to baseline, with no patients experiencing cognitive failure. Sherman et al. reported that compared with normative practice effects, these patients exhibited less improvement in the domains of processing speed, executive function, and verbal memory. However, because this was an uncontrolled, noncomparative trial, it is unclear if this relative stability reflects the absence of an expected practice effect in this treated population.
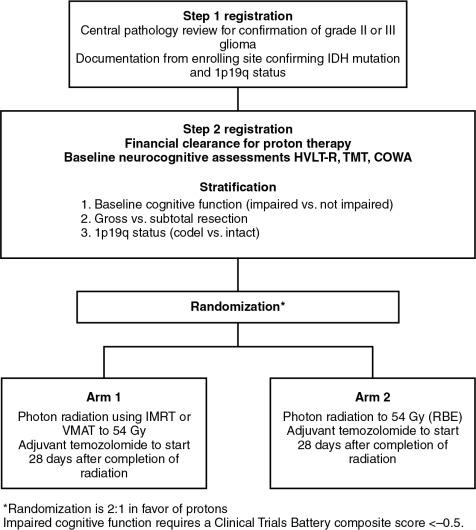
To provide the best evidence supporting the benefits of proton therapy in comparison with the best photon therapy (IMRT), randomized trials are needed. Historically, with a few exceptions, in the field of photon therapy, randomized trials have not been done to compare radiation techniques such as three-dimensional conformal versus IMRT. However, given that proton therapy is a fundamentally different form of radiation, it is not unreasonable that such trials be conducted. Currently, an ongoing randomized phase II trial is being conducted through the NRG Oncology Group, BN005 (clinicaltrials.gov identifier: NCT03180502). The schema for this trial is presented in Fig. 9.1 . Eligible patients include those with an IDH mutant grade II or III glioma and are randomized to receive protons versus photons. The central hypothesis is that the normal tissue-sparing offered by proton therapy will lead to superior preservation of cognitive function and reduced symptom burden relative to patients treated with photon-based therapy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here