Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
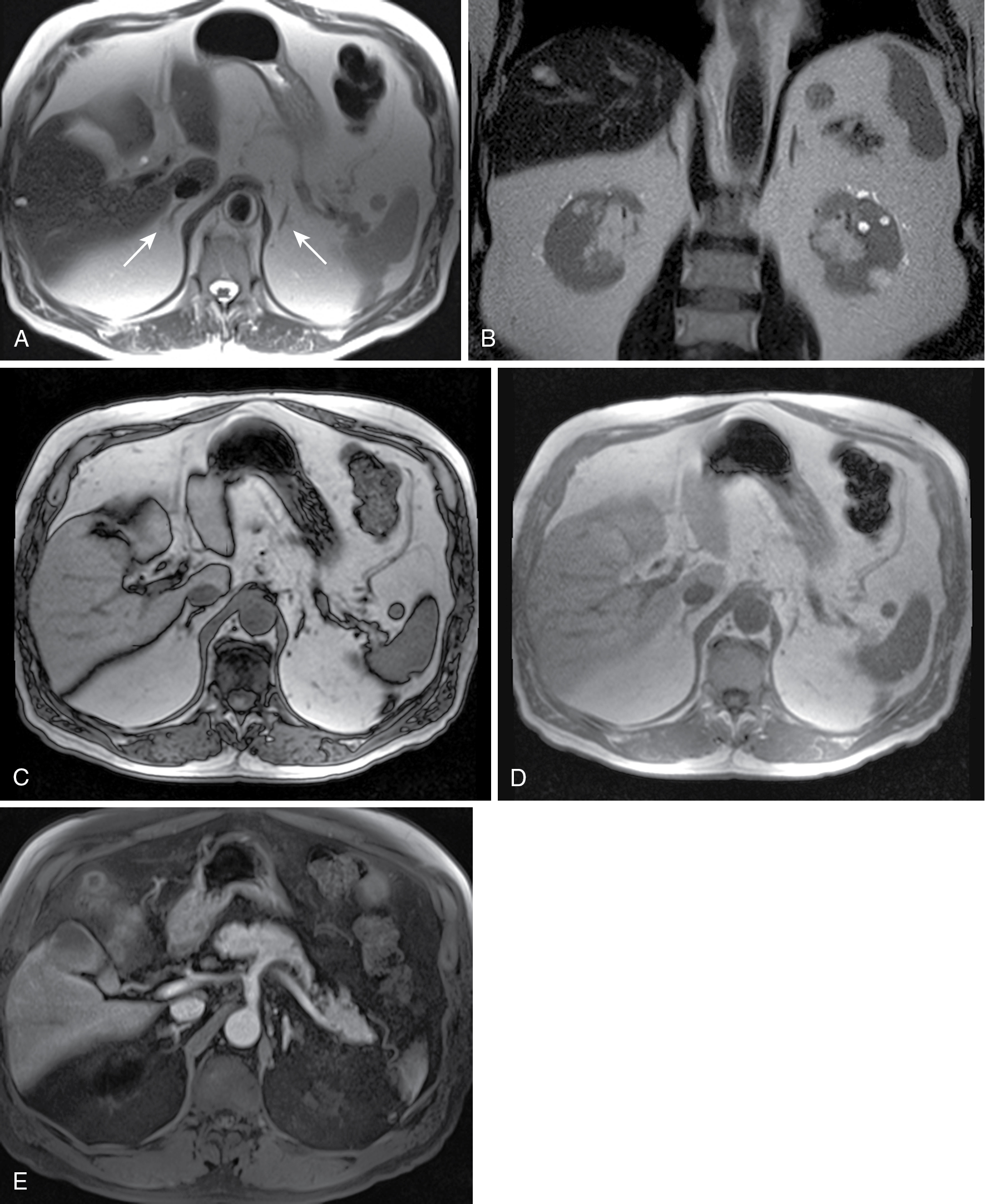
The adrenal glands are multifunctioning, inverted Y-shaped, retroperitoneal endocrine glands normally located superior to the kidneys in the perirenal space ( Fig. 28.1 ).
The adrenal glands mediate the stress response by releasing cortisol and are involved in secondary sex hormone synthesis and blood pressure regulation.
Absence of the Y-shape indicates development in the absence of an orthotopic kidney (i.e., agenesis or ectopia).
The histological zonal architecture of the adrenal gland is divided into two distinct components: the cortex, which is derived from mesothelium, and the medulla, which is derived from neural crest cells.
The adrenal cortex is composed of the zona glomerulosa, zona fasciculata, and zona reticularis.
The superficial zona glomerulosa is the primary site of aldosterone production.
The middle zona fasciculata synthesizes glucocorticoids (cortisol and corticosterone).
The inner zona reticularis produces androgens.
Adrenal cortical masses include adrenal adenoma, adrenal cortical carcinoma, adrenal myelolipoma, adrenal cysts, and metastasis.
Adrenal hemorrhage can involve the cortex.
The adrenal medulla is in the centermost portion of the gland and is responsible for catecholamine production.
Adrenal medullary masses include pheochromocytoma, neuroblastoma, ganglioneuroma, or ganglioneuroblastoma.
Arterial blood supply is via the superior adrenal artery (via phrenic artery), middle adrenal artery (via abdominal aorta), and inferior adrenal artery (via renal artery).
The left adrenal vein drains to the left renal vein and the right adrenal vein drains to the inferior vena cava (IVC).
Primary modality for evaluating adrenal adenoma
Adrenal glands enhance after iodinated contrast administration to approximately 50 to 60 Hounsfield units (HU).
Both unenhanced computed tomography (CT) and dynamic contrast-enhanced CT have a role.
Benign adenomas and malignant masses show rapid contrast enhancement, but adenomas demonstrate rapid washout of contrast.
Alternative to CT when contrast-enhanced CT is contraindicated.
Normal adrenal has low to intermediate signal on both T1- and T2-weighted imaging.
Chemical shift imaging with T1-weighted gradient echo (GRE) sequences can be used to evaluate for microscopic fat in nodules (see Physics Pearls box).
Frequency selective fat saturation can be used to determine presence of macroscopic fat in nodules.
Normal adult adrenal glands are not seen on ultrasound. Incidental masses near the superior renal poles may be adrenal in origin.
Can be used in pediatric evaluation.
Malignant adrenal lesions typically demonstrate 18-Fluoride deoxyglucose (18-FDG) uptake exceeding that of normal liver.
Whole body 123-Iodine scintigraphy with metaiodobenzylguanidine (MIBG) compounds can detect functional lesions and is superior to other modalities in the detection of extraadrenal lesions.
For patients with suspected pheochromocytoma (i.e., elevated urine catecholamine breakdown products) and negative MIBG scintigraphy, FDG-positron emission tomography (PET) or PET/CT may be useful.
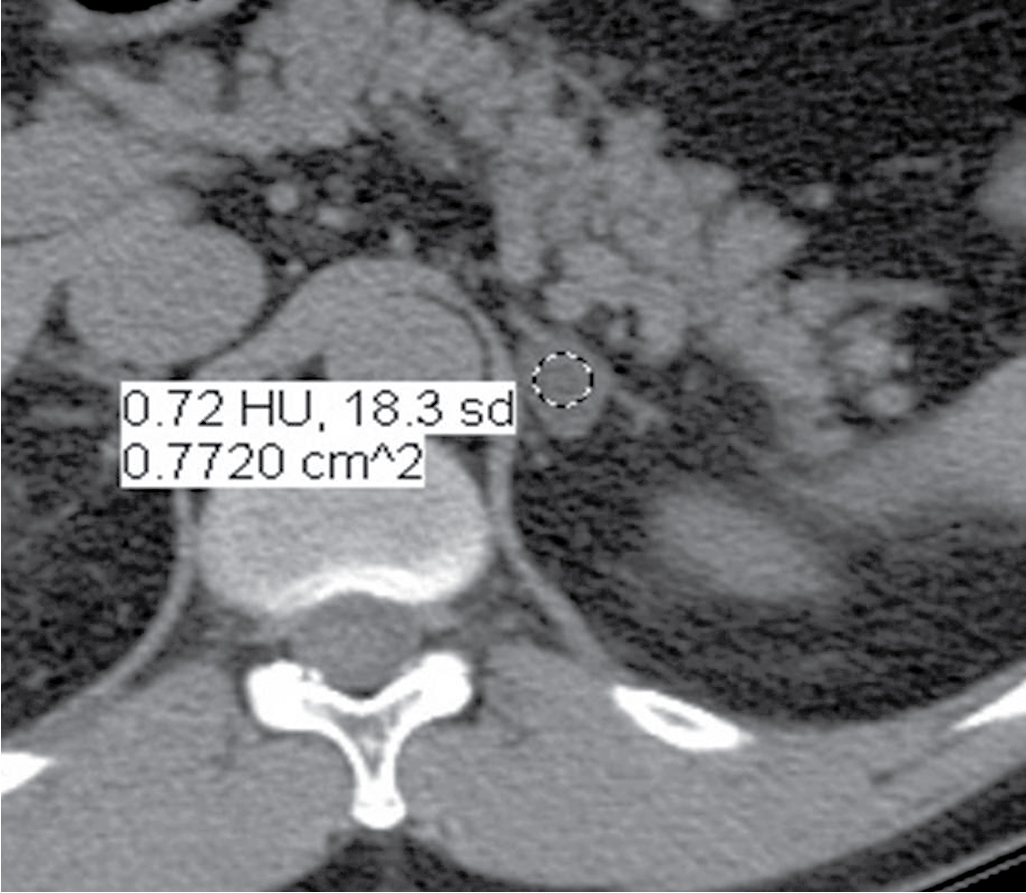
Unenhanced CT.
An adrenal nodule measuring less than 10 HU can be reliably diagnosed as a benign adenoma (98% specific), unless greater than 4 cm ( Fig. 28.2 ).
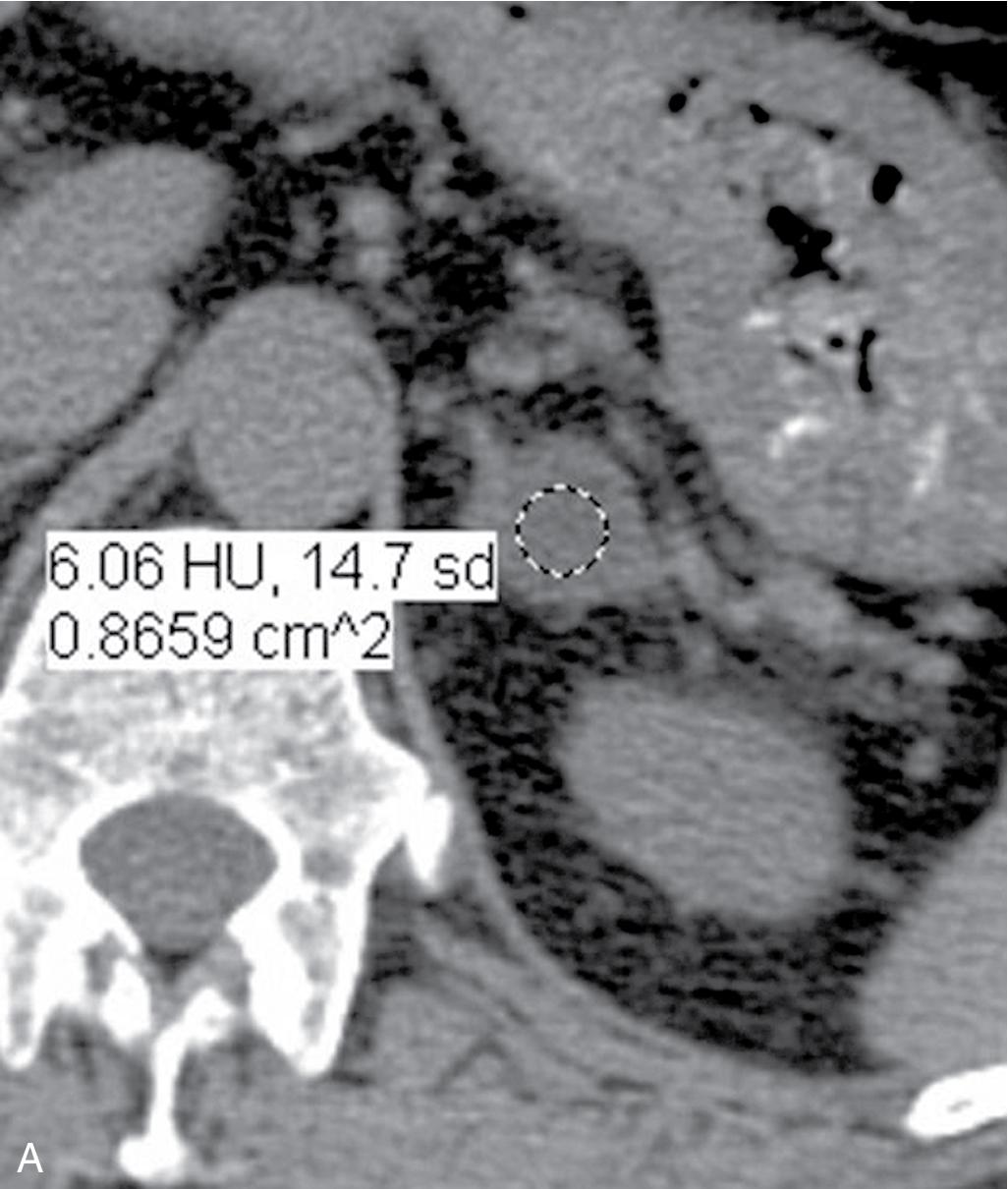
Adrenal washout CT.
Absolute washout protocol: noncontrast, venous phase, and delayed phase (15 minutes) imaging.
, where HU n , HU v , and HU d are the HU of an region of interest (ROI) in the nodule on noncontrast, venous phase, and delayed phase imaging, respectively.
Absolute washout over 60% is diagnostic of benign adenoma, unless greater than 4 cm in size ( Fig. 28.3 ).
Determination of benignity after noncontrast acquisition may negate need to complete postcontrast series.
Relative washout CT.
.
Relative washout over 40% is diagnostic of benign adenoma, unless greater than 4 cm in size.
This protocol can be performed if there is concern for radiation exposure.
Chemical shift imaging protocol.
Uses in-phase and opposed-phase T1-weighted GRE.
Adenomas will demonstrate signal dropout from microscopic fat.
Other lesions containing microscopic fat (e.g., well-differentiated adrenocortical carcinoma, clear cell renal cell carcinoma, and hepatocellular carcinoma) may also demonstrate signal dropout on opposed phase imaging.
Fat suppression can be used to demonstrate macroscopic fat as seen in myelolipoma.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here