Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acute otitis media (AOM) is the most common bacterial infection seen in pediatric patients, and treatment of AOM is the most common reason children receive antibiotics. Physician visits and antibiotic use for otitis media, however, have decreased in the last decade. AOM follows eustachian tube dysfunction, which is most often seen with a viral upper respiratory infection. Consequently, those organisms that are part of the normal flora of the nasopharynx are the major pathogens responsible for AOM. Although the cause has remained relatively constant over the last few decades, changes secondary to immunization and antibiotic pressure may now be occurring. Accurate diagnosis is essential for appropriate management. Of all the features associated with AOM, establishing appropriate therapy has recently undergone the greatest change; current guidelines now advocate that a substantial proportion of patients might appropriately be observed and not treated with antibiotics. These guidelines also now emphasize that more stringent criteria be applied for diagnosis, more attention must be paid to pain control, and patients must have access to antibiotics within 48 to 72 h if the patient fails to improve. This option is now recommended though only in the context of shared decision making and only in certain patients meeting very specific clinical criteria supported by the literature.
An 18-month-old white male was seen in the office of his primary care physician. He had recently had three episodes of AOM within the last 3 months. In his most recent episode he was treated with high-dose amoxicillin and he completed the amoxicillin one week prior to this current visit. He presented with irritability, low-grade fever of 100.8, and poor oral intake. Since his last visit he had lost 5 ounces. Physical exam revealed that both tympanic membranes were erythematous and mildly bulging. He was started on amoxicillin-clavulanate at 90 mg/kg/day in two divided doses. Close follow-up was recommended and 72 hours later he returned to the office without much improvement. He continued to sleep poorly and eat poorly. Physical exam revealed continued bulging of both tympanic membranes. The patient was then treated for 3 consecutive days with ceftriaxone, 50 mg/kg/day in a single daily dose. This was administered intramuscularly with lidocaine. At follow-up 1 week later the patient was markedly improved. The tympanic membranes were now normal and the patient was again gaining weight. Following completion of therapy quantitative immunoglobulins were obtained which were normal, the child’s parents were now able to have in-home childcare with only two other children, and referral was also made to otolaryngology for discussion of other options.
Virtually all children experience at least one middle ear infection during the first decade of life. AOM, however, is not limited to pediatric patients, and the disease seen in adults is similar to that seen in pediatrics with regard to pathogenesis, etiology, and treatment. In addition, at least in children, physician visits and antibiotic use for AOM have seen a decline in the last decade. This decline may be in part related to widespread use of pneumococcal conjugate vaccine (PCV) 7 and PCV 13 along with use of the influenza vaccine. The more stringent criteria advocated for the diagnosis of otitis media may also have contributed to this decline. However, AOM remains the most common reason children visit a physician, and it is also the second most common reason for a surgical procedure in the pediatric population, behind only circumcision. The persistent effusion seen in the middle ear after an episode of AOM is responsible for significant hearing loss and delay in development of language skills.
Recurrent and persistent disease is also more commonly seen now. There are several risk factors for acute and recurrent otitis media ( Box 32.1 ). By age 3, approximately one-third of children will have been identified as otitis prone, one-third as having no trouble with otitis media, and one-third as occasionally infected. Those with recurrent disease contribute greatly to antibiotic usage and development of antibiotic resistance.
Onset of otitis media in infancy
Male gender
Sibling with recurrent acute otitis media
Bottle feeding only
Parents who smoke at home
Daycare attendance
Craniofacial anomalies
Anatomic, physiologic, and immunologic factors all contribute to this epidemiology. Furthermore, the eustachian tube is shorter and more horizontally positioned in children ( Fig. 32.1 ). This makes it easier for nasopharyngeal flora to gain access to the middle ear.
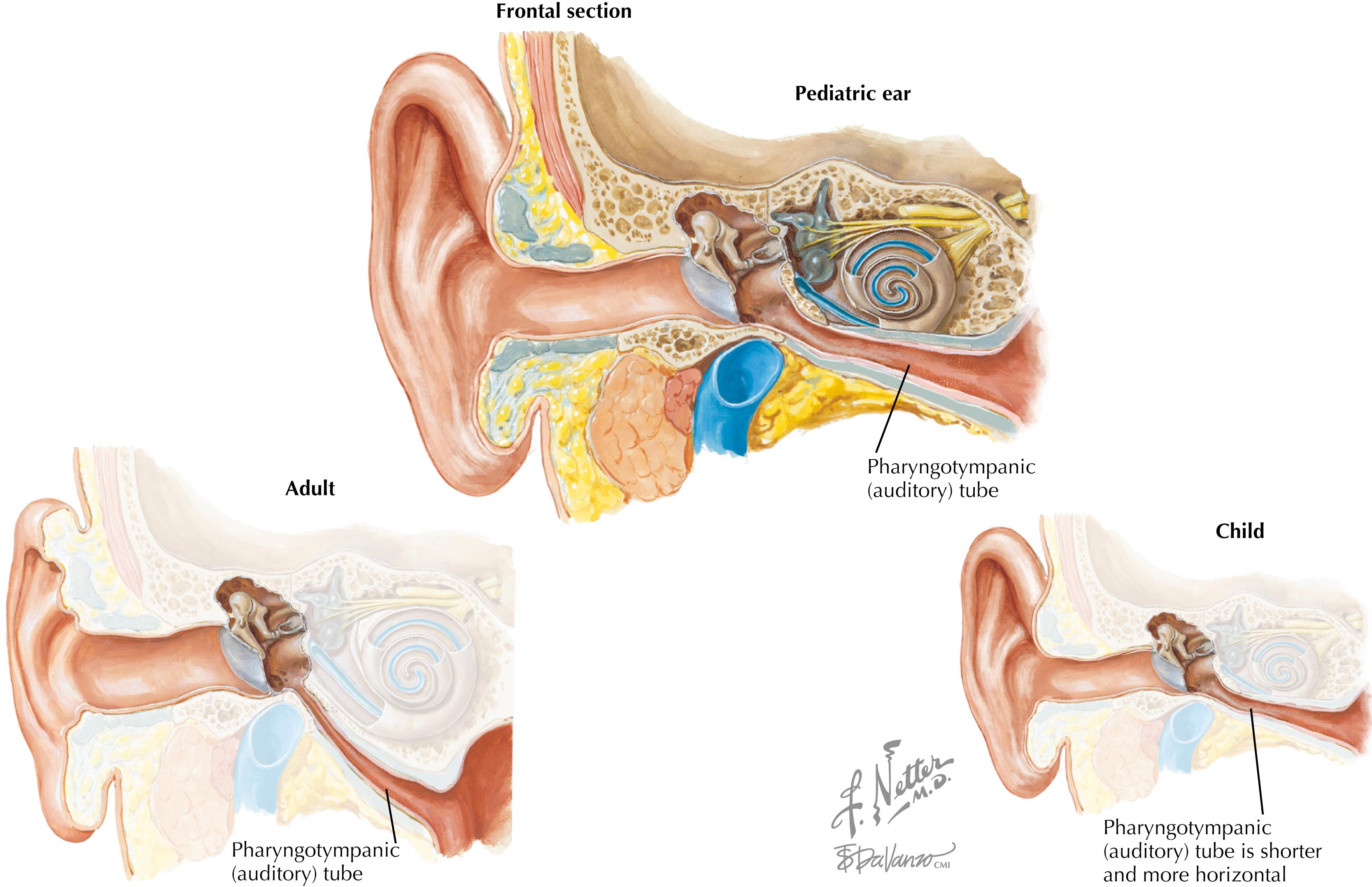
Eustachian tube malfunction is generally the final step that leads to nasopharyngeal organisms gaining access to the middle ear. Mucosal edema, which can lead to obstruction of the eustachian tube, impairs drainage of secretions of the middle ear. Bacteria that then gain access to the middle ear can readily multiply. Respiratory syncytial virus, parainfluenza virus, and influenza virus are the viruses most commonly responsible for causing impairment of eustachian tube function. Less commonly, other factors play a pivotal role in the development of AOM, including allergy, genetic factors (Native American or Eskimos), or immunologic factors. The role of daycare centers in the epidemiology of AOM and recurrent disease is a significant issue as well. Daycare attendance in the United States has increased substantially, and currently half of US children attend a daycare center regularly. The larger the number of children in attendance at the center, the greater the likelihood of exposure to a wide variety of viral pathogens. This can obviously lead to the increase in diagnosis of AOM seen in such children ( Fig. 32.2 ). Besides daycare attendance, several other factors appear to be associated with recurrent episodes of otitis media, otitis proneness. These associations include male sex, family history, atopic disease, age at first diagnosis (the younger the age the greater the risk), and non-Hispanic white race.
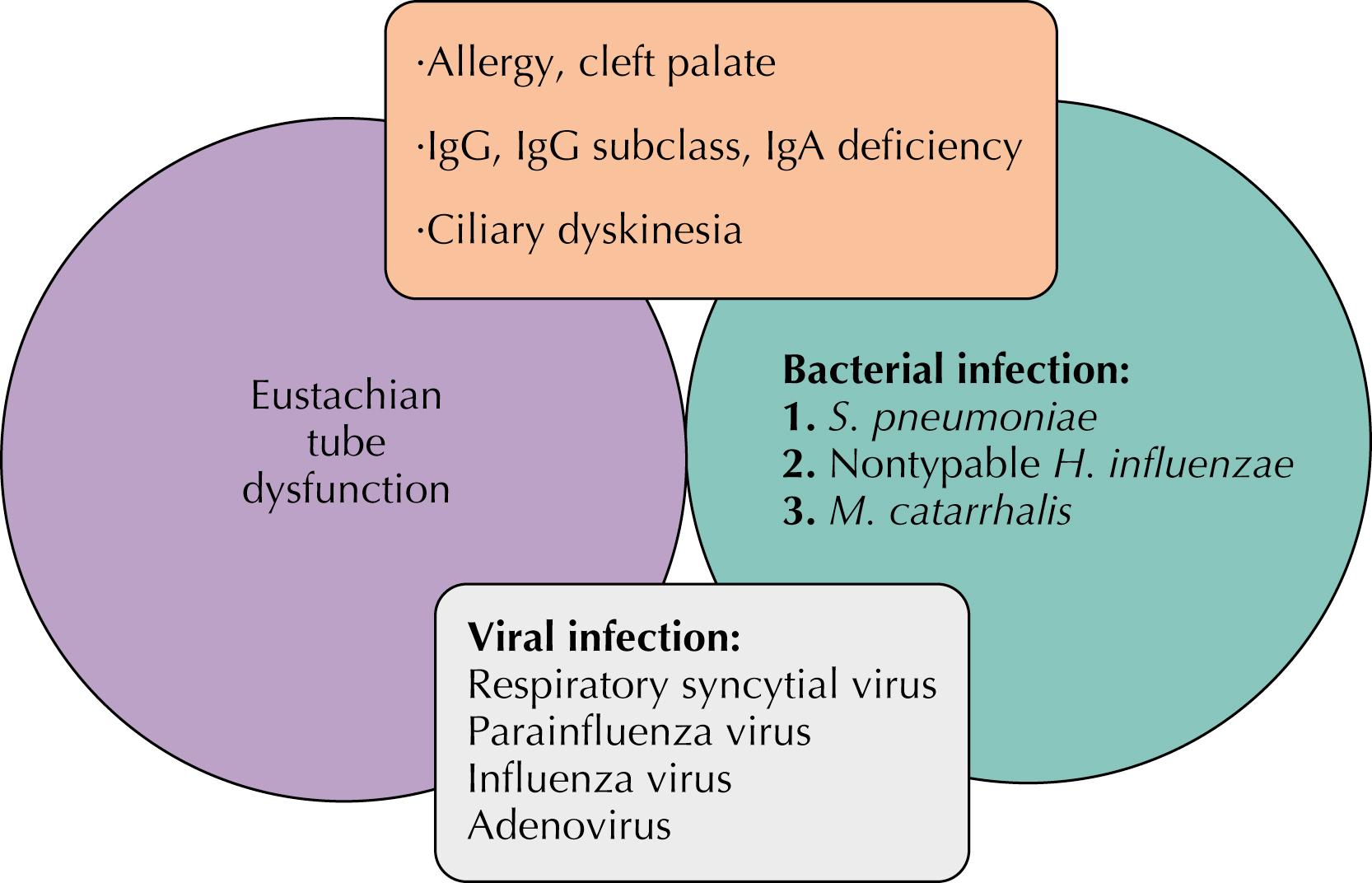
The cause of AOM naturally reflects the pathophysiology. Streptococcus pneumoniae , nontypable Haemophilus influenzae, and Moraxella catarrhalis are the leading pathogens. Whereas viruses play a pivotal role in predisposing the host, middle ear taps of children with AOM rarely yield a viral pathogen alone.
Since 2000, universal immunization of all infants with conjugated PCV has been recommended. Since the introduction of this vaccination, several changes in the epidemiology of AOM have been seen. There have been several benefits, although the reduction in AOM overall has been modest compared with the reduction in invasive disease caused by S. pneumoniae . Introduction of the 13 Valent conjugated pneumococcal vaccine (PCV-13) occurred in 2010. Subsequent to introduction of these vaccines, there appears to be some decline in the occurrence of otitis media due to vaccine serotypes. Vaccine serotypes continue to more likely be drug resistant. Replacement of these vaccine types with infections with nontypable H. influenzae or nonvaccine strains of S. pneumoniae has been reported.
Ear pain is the most specific finding associated with AOM. This finding occurs in approximately two-thirds of patients; however, it is less often seen in younger patients. This may relate to an inability to adequately verbalize this manifestation. In general, symptoms in younger patients tend to be less specific, as is the case in other pediatric infections. Patients younger than 1 year old are asymptomatic about half of the time. Likewise, otorrhea is a highly specific but infrequently occurring finding and is often associated with sudden relief of pain. Less specific symptoms include coryza, irritability, poor feeding, sleep disturbance, fever, hearing loss, “tugging” at the ears, and difficulty with balance.
The initial presentation is helpful in predicting the causative organism. Disease caused by S. pneumoniae or S. pyogenes is more likely to manifest suddenly, with high fever and severe otalgia. Spontaneous resolution is also less likely, and complications are more likely to occur with infection with these organisms. On the other hand, M. catarrhalis is associated with the greatest likelihood of spontaneous resolution and the mildest disease. Disease caused by H. influenzae falls between these two extremes. Recent studies have not consistently demonstrated a correlation between symptoms with the initial diagnosis of AOM. Ear pain, otalgia, is frequently associated with AOM. American Academy of Pediatrics (AAP) guidelines continue to emphasize the need to inquire about the presence of pain and consider options for symptomatic treatment of otalgia, including topical therapies.
Making the diagnosis of AOM can be challenging. The diagnosis is almost invariably confirmed in clinical practice by physical examination alone ( Fig. 32.3 ). Although the symptoms are often nonspecific, the patient may be very uncooperative, and adequately restraining such a patient is essential. Even with adequate restraint, additional difficulties with examination may arise. The canals may be occluded with cerumen, and removal is difficult. Moreover, the practitioner must have appropriate equipment, which means adequate illumination and a proper seal with the speculum on the otoscope. Disposable specula are not as satisfactory in producing an adequate seal. Only when all these conditions are satisfied is an adequate inspection and attempt at insufflation (pneumatic otoscopy) possible.
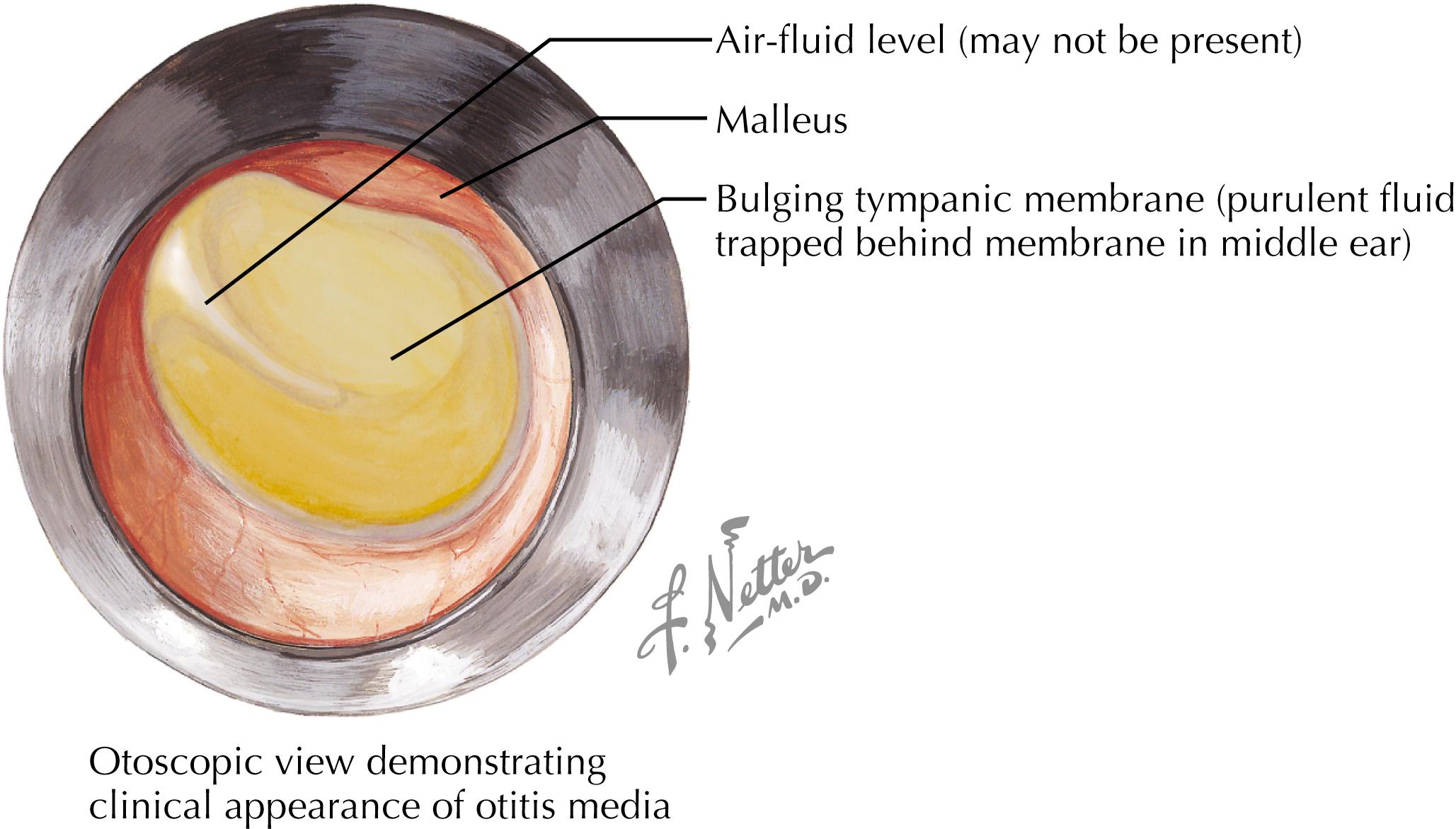
In 2019, the AAP adopted more stringent criteria for the diagnosis of AOM. More emphasis is placed on the physical exam especially with regard to the presence of a bulging tympanic membrane. The presence of moderate or severe bulging of the TM or the new onset of otorrhea not due to external otitis confirms the diagnosis of AOM. Mild bulging of the TM, and recent onset of ear pain or intense erythema of the tympanic membrane is a second method recommended for confirmation of the diagnosis.
Much of the difficulty associated with establishing the diagnosis of AOM results from the fact that a middle ear effusion that is not purulent can be seen as part of a viral upper respiratory infection. Such an effusion is referred to as otitis media with effusion (OME). This can also occur before AOM or after therapy for AOM. Antibiotic therapy is of no benefit for the patient with OME, and distinguishing OME from AOM can be especially challenging.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here