Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acute thrombosis of the lower extremity deep veins is a significant public health problem affecting more than 350,000 people in the United States each year. Lower extremity deep vein thrombosis (DVT) is associated with a 6% mortality at 30 days and responsible for 100,000 to 300,000 deaths annually. , Its economic impact is substantial; in the United States, the annual cost of DVT was estimated to be 7.5 to 39 billion U.S. dollars in 2010.
Advances in risk prediction scores, diagnostic imaging, and medical therapy, specifically direct oral anticoagulants, have increased the safety and convenience of management of acute DVT, recurrent thrombosis, and DVT prophylaxis. Therapeutic anticoagulation remains the foundation of medical management of DVT and should be started in patients with high pre-test probability of acute DVT before confirmation or in patients with confirmed DVT, who do not have an absolute contraindication to anticoagulation. This chapter will present the diagnosis and management of DVT including optimal diagnostic and therapeutic approach to isolated distal DVT, duration of therapy for DVT, and appropriate indications for invasive treatment for acute DVT.
The clinical manifestations of acute DVT are nonspecific and presentations vary from asymptomatic to dramatic including phlegmasia cerulea dolens or venous gangrene. Common signs and symptoms of DVT include a dull ache or pain in the leg, tenderness, swelling, erythema, cyanosis of the leg, and fever. These symptoms cannot reliably distinguish DVT from hematoma, cellulitis, congestive heart failure or superficial thrombophlebitis. Concurrent edema, cyanosis, and pain are features of phlegmasia cerulea dolens. Venous gangrene, a rare complication of DVT characterized by thrombotic occlusion of superficial collateral veins and sometimes associated with phlegmasia, can result in limb loss with palpable arterial pulses. It most often occurs in patients treated acutely with warfarin for cancer-associated thrombosis, or heparin-induced thrombocytopenia with thrombosis. Venous gangrene is associated with warfarin-mediated protein C depletion in the setting of ongoing thrombin generation. ,
The diagnostic value of signs and symptoms of DVT and their combinations have been extensively studied. The most common symptom, calf pain, has a sensitivity between 75% and 91% and specificity between 3% and 87%. The sensitivity of calf swelling for DVT diagnosis ranges from 35% to 97%, and its specificity ranges from 8% to 88%. In part, such variability is due to the high prevalence of the same signs and symptoms in patients without DVT. In patients at high risk for DVT, the diagnostic value of clinical signs and symptoms is substantially higher. For example, in patients with cancer, the negative predictive value of the absence of swelling is as high as 97% for outpatients and 92% for inpatients. A valid alternative diagnosis, such as cellulitis or a musculoskeletal disorder that explains the presence of signs and symptoms, also improves the negative predictive value of the clinical examination.
High variability and lack of specificity limit the role of clinical examination in patients with suspected DVT. A meta-analysis of studies evaluating individual clinical features of DVT showed only past history of DVT and malignant disease are useful for diagnosis, and no individual clinical feature is useful for ruling out DVT. The delay in clinical presentation makes the clinical diagnosis of DVT even more challenging. On average, patients are seen by a medical professional more than 4 days after onset of symptoms, and in more than 20% of patients, more than 10 days after onset. , Withholding treatment until clinical evaluation in primary care settings leads to inadequate management of more than 10% of patients with DVT.
The concentration of D-dimer (DD) in plasma is a biomarker that is widely used for the diagnosis of DVT. DD is produced by degradation of cross-linked fibrin by plasmin. Elevated levels signify ongoing fibrin formation and degradation, which occurs as part of the physiologic response to injury in patients undergoing surgical procedures or trauma, the normal changes during pregnancy, and the pathophysiologic processes in patients with cancer, infection, inflammation or thrombotic disorders. The degree of DD elevation in patients with DVT varies with the size and extent of the thrombus, the time from DVT onset, and the use of anticoagulation.
Currently used DD assays differ in result type (qualitative versus quantitative), the specificity of antibody to various binding sites on the DD molecule, units of measurements, reference values, speed and cost of testing. Quantitative point-of-care tests are more sensitive and may be superior to exclude DVT in these patients. In general, use of point-of-care DD testing remains limited.
For the aforementioned reasons, DD assays are difficult to standardize and results are not comparable across laboratories. In addition, assay sensitivity for DVT diagnosis ranges from 60% to 96%. , Enzyme-linked immunosorbent or immunofluorescent assays (ELISA or ELFA) and latex agglutination assays are the most sensitive assays. ,
Low specificity limits the use of DD in a subset of patients with suspected DVT, including those who have a high pre-test probability of DVT, who are pregnant, have cancer, have had recent surgery or trauma, or who are hospitalized. However, concentration of DD below a cutoff value in low or intermediate pre-test probability cases indicates a very low probability of DVT. Recent adjustments of negative DD values based on age or pre-test clinical probability have increased the diagnostic value of DD testing in these patients. The value of DD testing for evaluation of DVT is further population specific as it does not exclude DVT with sufficient accuracy in cases of distal thrombi, with use of anticoagulation, or of long duration between the initiation of thrombosis and testing. , , Similar to clinical evaluation, the use of DD as a single diagnostic tool may result in inadequate management of more than 15% of patients with suspected DVT. DD is best integrated with a clinical risk assessment of the patient (see below) and when used as a diagnostic test in the correct clinical context.
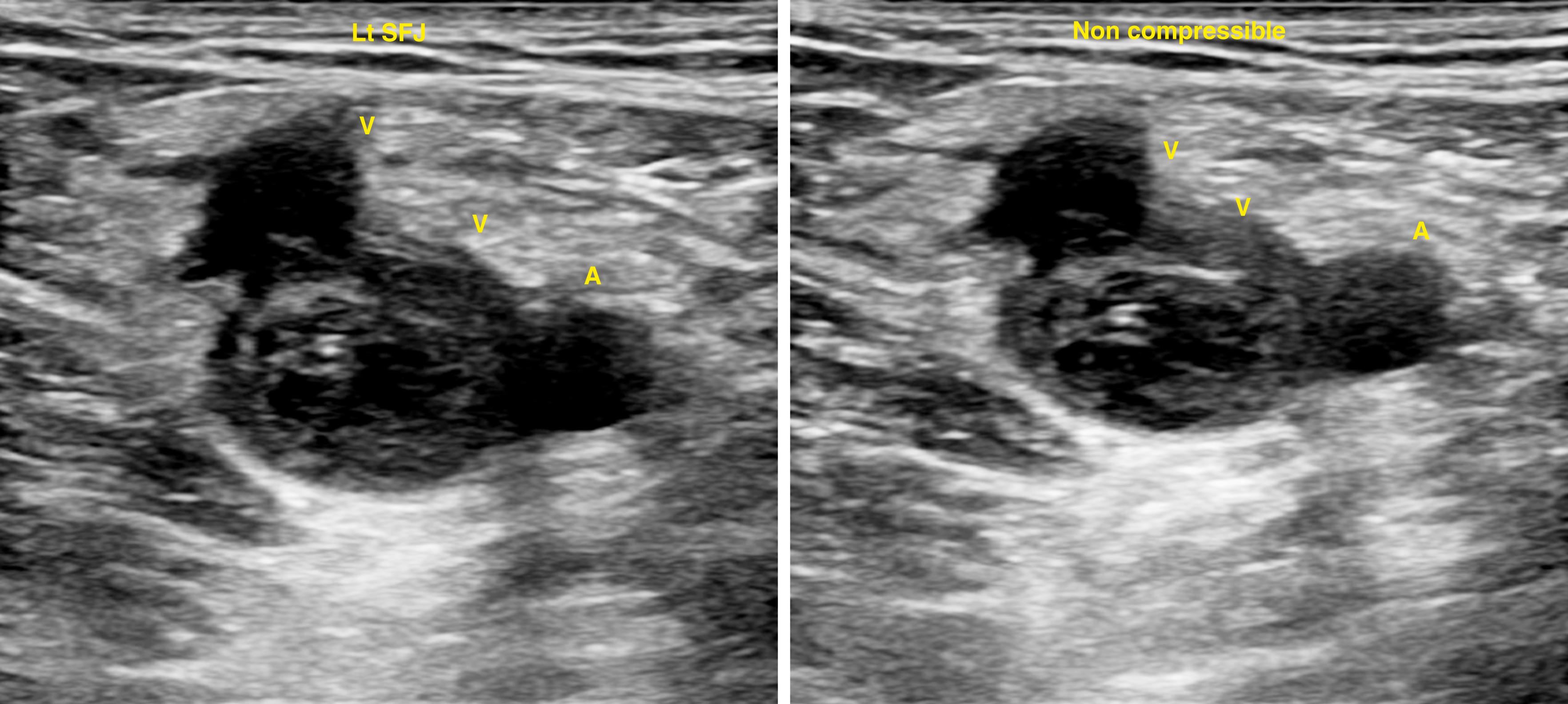
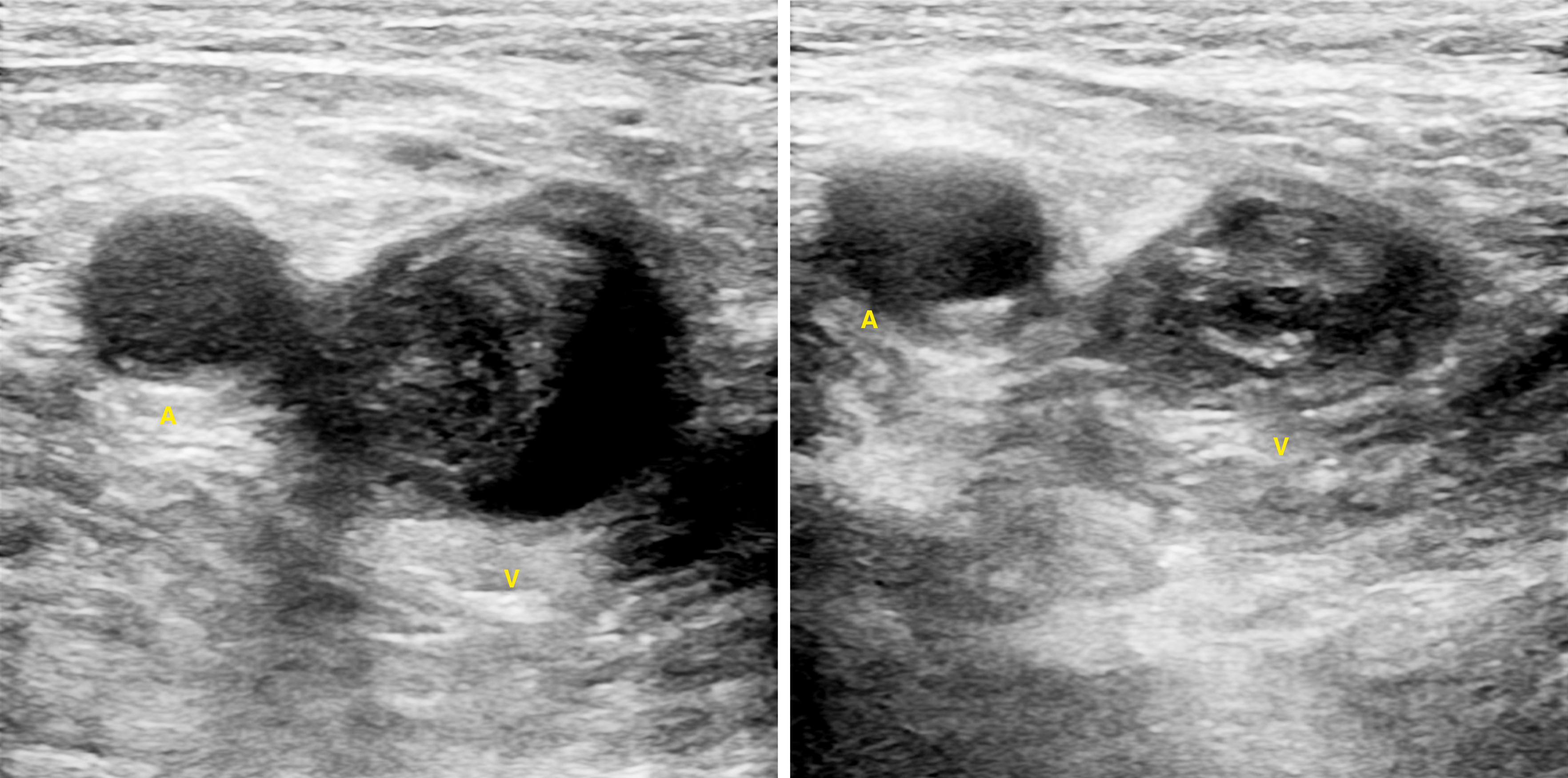
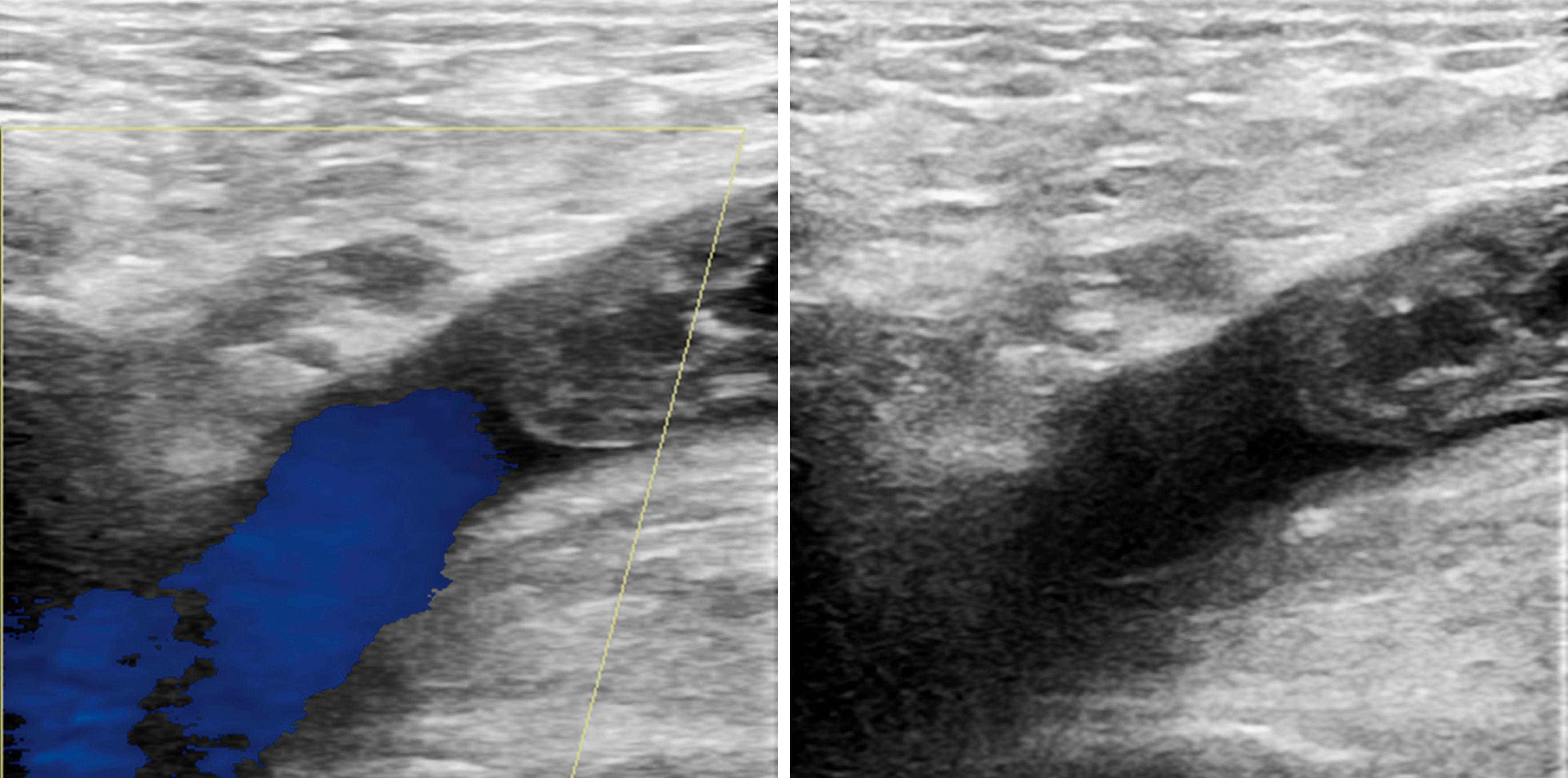
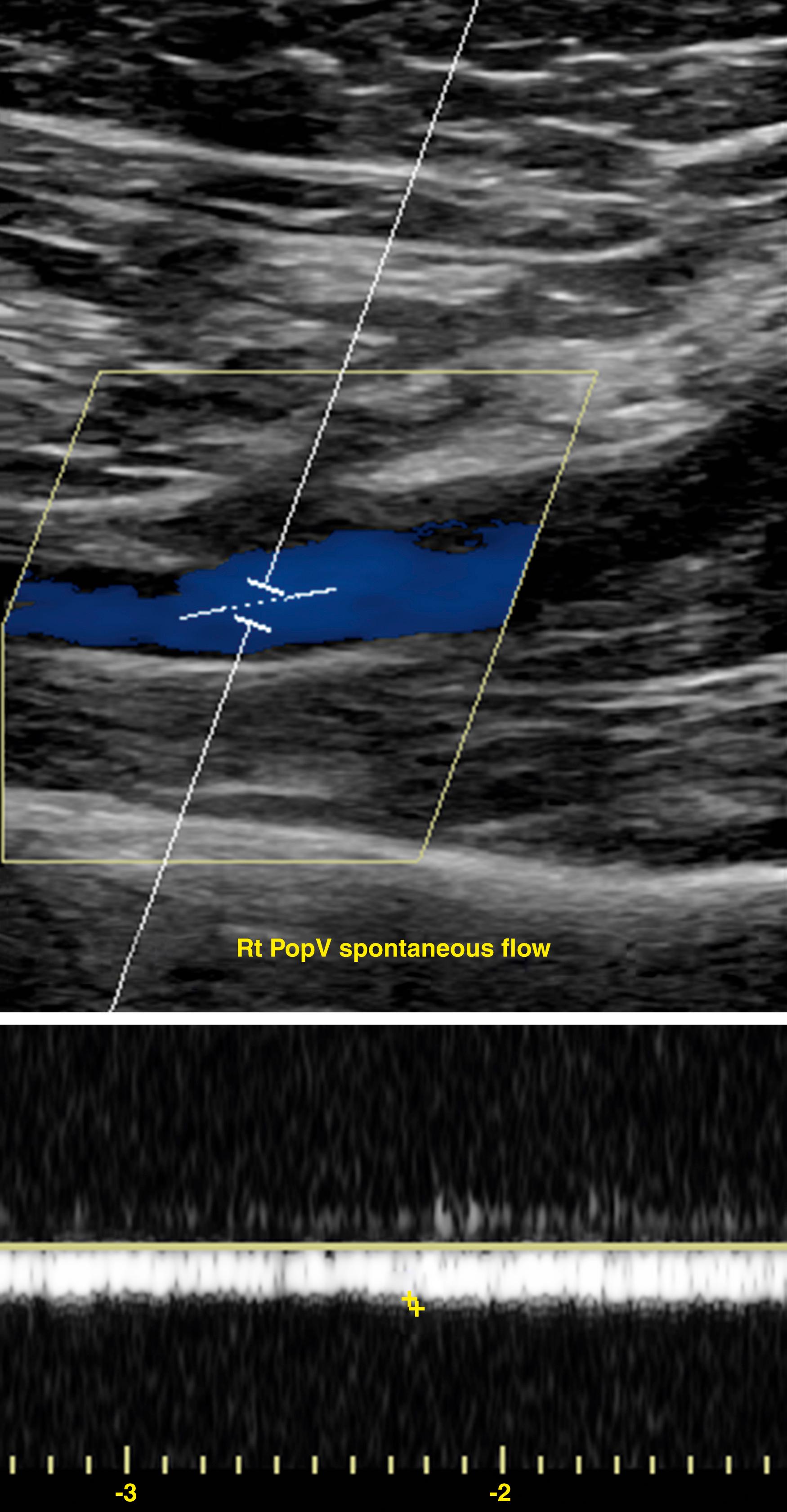
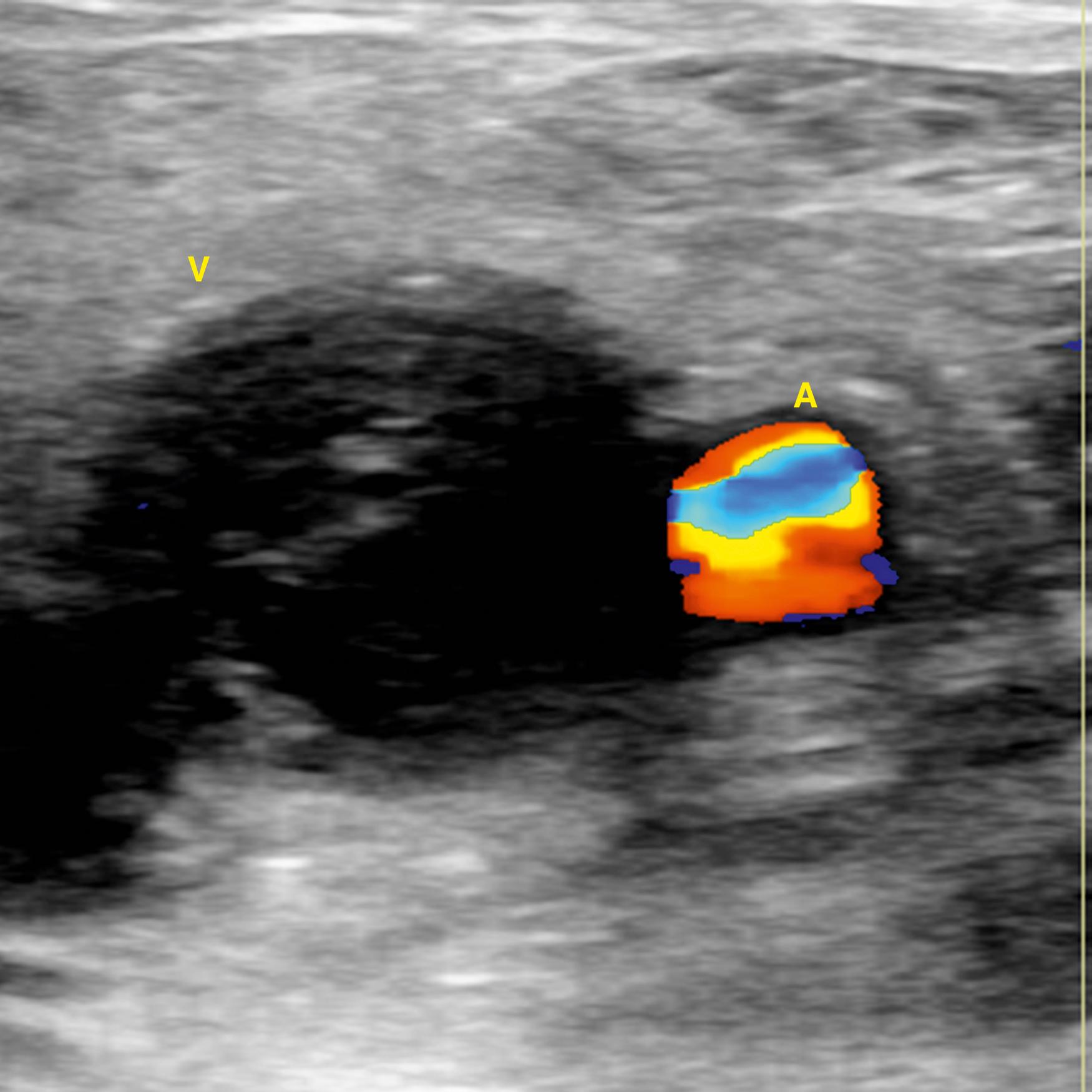
Duplex ultrasonography is the first-line imaging modality for evaluation of DVT and has almost completely replaced venography because of its accuracy, lack of radiation, portability, noninvasiveness, and relative cost-effectiveness (see Ch. 25 , Vascular Laboratory: Venous Duplex Scanning). In addition, ultrasound can distinguish among nonvascular pathologic processes such as inguinal adenopathy, Baker cyst, abscess, and hematoma. The primary diagnostic criteria of duplex ultrasound for DVT is non-compressibility of the vein under moderate pressure from the transducer with secondary criteria including increased intraluminal echogenicity, increased venous diameter, absence of spontaneous blood flow, and absence of flow augmentation with distal compression ( Figs. 148.1–148.5 ). Noncompressibility has excellent test characteristics for the detection of proximal DVT, with sensitivity and specificity of 97% and 94%, respectively.
Limitations of compression ultrasound are its decreased accuracy in the evaluation of calf veins, fresh thrombi, and small segmental thrombi as well as limited use in patients with obesity, significant edema, overlying bandages or casts, and recent DVT with recrudescent symptoms. Additional pitfalls in venous duplex imaging include misidentification of veins, missing or duplicate venous systems, systemic illness, or hypovolemia resulting in decreased venous distention, and areas not amenable to compression such as the iliac veins, the femoral vein at the adductor canal, and the subclavian veins. As with most ultrasound-based imaging studies, the quality of the examination depends on the skill of the individual performing the study.
There are a number of ultrasound strategies used for detection of DVT including single limited (popliteal veins and proximal vessels), serial limited, and whole-leg ultrasonography. The serial limited strategy includes a repeat ultrasound approximately one week after an initial negative study if no alternative diagnosis is identified and assesses for proximal extension of distal DVT. Whole leg ultrasonography images both distal and proximal veins, eliminating the need for repeat imaging; however, it may identify distal DVTs that do not require anticoagulation. The risk of venous thromboembolism (VTE) with negative studies using either the whole-leg or serial limited strategy is less than 1%. , There is some controversy regarding the most appropriate diagnostic algorithm and the clinical importance of identifying and treating distal DVTs (isolated calf vein thrombi). The American College of Chest Physicians (ACCP) Guidelines for diagnosis of VTE are equivocal regarding use of serial proximal leg or whole-leg ultrasound in patients with moderate or high pre-test probability of DVT. However, the ACCP guidelines suggest whole-leg imaging for patients who are unable to return for serial imaging or with severe symptoms consistent with calf DVT. Guidelines from other professional societies are similarly equivocal regarding the optimal initial ultrasound technique or favor whole-leg ultrasonography. Studies to date have not found differences in the test performance characteristics of limited versus whole-leg strategies, although many institutions favor whole-leg imaging for comprehensive venous assessment. ,
Ultrasound is not sufficiently accurate in all patients and test characteristics are affected by pre-test probability and location of thrombus. In contrast to the 94% sensitivity of ultrasound for detection of proximal DVT, the sensitivity is only 63% for distal DVT. This results in overall sensitivity of 90% and specificity 94% for detection of both proximal and distal DVT. The diagnostic properties of ultrasonography are also substantially different among subpopulations of symptomatic outpatients. In patients with a high Wells score ( Table 148.1 ), sensitivity of proximal ultrasound is 91% for proximal and distal DVT and specificity approaches 100%; whereas sensitivity and specificity are 61% and 99%, respectively, in patients with an intermediate Wells score; and 67% and 98% in patients with a low Wells score. In asymptomatic patients, sensitivities of ultrasound for detection of proximal and distal DVT are 66.7% and 39.0%, respectively, with an overall specificity of 96.5%. These data indicate that the use of ultrasound alone for evaluation of DVT in low pre-test probability or asymptomatic patients may result in a significant number of false positives and is not recommended. However, in symptomatic patients or patients with intermediate or high pre-test probability, ultrasound can reliably rule out proximal DVT.
| Clinical Characteristic | Points |
|---|---|
| Active cancer (treatment within last 6 months or palliative) | +1 |
| Paralysis, paresis, or plaster immobilization of lower extremity | +1 |
| Bedridden 3 days or major surgery within past 12 weeks requiring general or local anesthesia | +1 |
| Localized tenderness along deep venous system | +1 |
| Entire leg swollen | +1 |
| Calf swelling 3 cm compared to asymptomatic side | +1 |
| Pitting edema isolated to symptomatic leg | +1 |
| Collateral superficial veins (nonvaricose) | +1 |
| Previous DVT | +1 |
| Alternative diagnosis at least as likely as DVT | −2 |
Contrast venography for the sole purpose of diagnosing DVT is largely of historical interest. Diagnostic use of contrast venography has declined dramatically due to its expense and inconvenience, the potential for patient discomfort, and in light of the utility, accuracy, and safety of ultrasonography. , Venography may be helpful in cases when ultrasound suggests the presence of proximal obstruction by demonstrating a loss of the flow phasicity but fails to visualize the thrombus in iliac veins. Several historical studies found contrast venography was more accurate in the diagnosis of acute calf DVT, although ultrasound techniques have since improved and the clinical significance of this is uncertain. , Because of its high sensitivity and specificity, contrast venography can be used as the “golden backup” when the diagnosis of acute DVT remains in question after an ultrasound or in patients with previous DVT and non-diagnostic ultrasonography.
While computed tomographic arteriography is an excellent technique for the diagnosis of PE, its venous counterpart, computed tomographic venography (CTV) has yet to gain traction in the diagnosis of acute DVT in the lower or upper extremities. CTV is as accurate as ultrasound in the diagnosis of proximal DVT with a sensitivity and specificity of 98% and 100% in the thigh and 94% and 100% in the pelvis, respectively, and an overall positive predictive and negative predictive values of 92% and 100%, respectively. Use of CTV has the benefit of evaluating pelvic veins and the inferior vena cava (IVC), the assessment of which are limited with ultrasound, as well as of detecting other etiologies of lower extremity swelling such as malignancies in the pelvis or extrinsic compression by other vascular structures such as iliac vein compression syndrome (also called May–Thurner syndrome). , When CTV is used in conjunction with evaluation of PE, it adds only 3 to 5 minutes to the examination, making it an attractive option as the sole diagnostic modality for acute lower extremity DVT and PE. Limitations of CTV include artifacts from orthopedic implants, poor venous enhancement, interpretation errors due to inexperience or nearby pathology, and the requirement for contrast administration which is a concern for patients with renal dysfunction. It is worth noting not all studies found CTV sufficiently accurate in the diagnosis of acute DVT with CTV. Peterson et al. demonstrated that although the sensitivity is high at 93%, producing a 97% negative predictive value, the ability of CTV to accurately diagnose DVT has a specificity of 71%, giving a positive predictive value of only 53%; and others have shown a 50% false-positive rate for CTV for pelvic DVT.
This technology is based on the detection of moving versus stationary tissues. MRV can be used with or without contrast enhancement. Non-contrast-enhanced techniques include time-of-flight (TOF) imaging, spin echo, steady-state free procession, flow-independent, and phase-contrast imaging. However, contrast-enhanced MRV is less susceptible to artifacts, acquired faster, has better signal-to-noise ratio and is more accurate in slow flow vessels ( Fig. 148.6 ).

A meta-analysis of the accuracy of MRI for the diagnosis of acute DVT found a pooled sensitivity of 92% (range 0%–100%), and specificity of 95% (range 43%–100%). The sensitivity and specificity were higher for proximal DVT than for below-knee thrombus. Studies comparing MRV to contrast venography, found the sensitivity and specificity of MRV up to 100% for the diagnosis of femoro-popliteal DVT, however accuracy was lower for distal thrombi. Overall, in the evaluation of proximal DVT, MRV has similar accuracy as ultrasound and contrast venography, with the benefit of high rates of detection of the proximal extent of the thrombus and isolated pelvic thrombi. For example, one small study showed MRV identified a thrombus in 27% of patients who sustained a PE with no detectable source of thrombus by ultrasound. Moreover, vessel wall enhancement associated with acute thrombus can be visualized with MRV, allowing the examiner a crude detection of thrombus age. ,
Although MRV technology demonstrates excellent accuracy for the detection of acute DVT, it has several disadvantages. The examination requires a nonmoving patient for long imaging times and cannot be used in patients with MRI incompatible devices or clips. Gadolinium can be toxic in patients with renal dysfunction and the need for frequent examinations can produce problematic utilization issues in larger institutions. Finally, the quality of MRV depends on experience with contrast timing and interpretation and therefore is institution dependent. MRV has been recommended as the imaging modality of choice by the American College of Radiology (ACR) appropriateness criteria for evaluation of pelvic or thigh DVT when ultrasound is nondiagnostic or for initial investigation in case of suspect central vein or pelvic vein thrombus.
18 F-labeled fluorodeoxyglucose ( 18 F-FDG) is a glucose analogue that is actively and avidly absorbed by tissues and cells with rapid metabolism. Among these are tumor cells, endothelial cells, macrophages, and lymphocytes. 18 F-FDG is frequently used in positive emission tomography/computer tomography (PET/CT) for the detection of primary and metastatic cancer; however, it has shown value in the diagnosis of acute DVT. 18 F-FDG PET/CT can detect acute DVT, determine thrombus age, and differentiate acute thrombus from tumor thrombus. Several studies have characterized the ability of 18 F-FDG PET/CT to detect acute DVT, but few studies have examined its utility for the direct diagnosis of acute DVT. Rondina et al. evaluated 12 patients with ultrasound-proven proximal acute DVT with 18 F-FDG PET/CT (median time from symptoms to PET/CT scan was 26 days). They demonstrated that metabolic activity was significantly higher in thrombosed vein compared to nonthrombosed veins and that 18 F-FDG PET/CT had excellent test characteristics for the diagnosis of acute symptomatic proximal DVT. Limitations of the technique include cost, radiation exposure, availability, false positives due to active inflammation or infection, and limited clinical data.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here