Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Disorders presenting in neonates and young children comprise a heterogeneous group of conditions that can be divided into two broad categories, entities with a known etiology and those of unknown or poorly understood etiology. The well-characterized disorders include those that reflect altered lung growth and development or a poor transition from intrauterine to extrauterine life, including pulmonary hypoplasia, hyaline membrane disease (HMD), chronic lung disease of prematurity (eg, bronchopulmonary dysplasia [BPD]), persistent pulmonary hypertension of the newborn (PPHN), and pulmonary interstitial emphysema (PIE). Those classified as poorly understood include two idiopathic lung diseases unique to infants and very young children: pulmonary interstitial glycogenosis (PIG) and neuroendocrine cell hyperplasia of infancy (NEHI).
Pulmonary hypoplasia refers to the incomplete development of the lung, resulting in reduced number and complexity of acini
Pulmonary hyperplasia, typically associated with an airway obstruction, is characterized by a marked increase in alveolar number
Estimated 10 per 10,000 live births
Typically associated with pregnancy complications or coexisting malformations
Compression deformities may be present from prolonged oligohydramnios (contractures, Potter facies, arthrogryposes)
In severe cases, neonates present with respiratory distress and difficulty in ventilation; they frequently get pneumothoraces and PIE
Mild cases or those of postnatal onset may present later in life with dyspnea and cyanosis on exertion or a history of repeated respiratory infections
When all lobes are affected, associated with tracheal or laryngeal atresia
Focal lesions such as bronchial stenosis and atresia will cause subtotal involvement
Most patients present within the first 6 months of life with respiratory distress
Chest radiograph
Findings vary depending on the mechanism and severity of hypoplasia
Chest computed tomographic scans
May show loss of lung volume and abnormal or absent normal airway branching
Chest radiograph
Initially demonstrates an opacified lobe, commonly an upper lobe, which progresses to overinflation and hyperlucency
Poor prognosis in the setting of prolonged oligohydramnios or residual lung volume of <45%
Patients are at an increased risk for pneumothorax, PPHN, and CNLD
Long-term survivors are at risk for chronic pulmonary insufficiency, recurrent respiratory infections, and reduced exercise tolerance, even in mild cases
May require surgical resection to avoid further respiratory compromise
May be fatal if associated with mediastinal shift and compression of unaffected lobes
With early prenatal arrest, the lungs are notably small, and lung weight is often less than 40% of expected
Postnatal arrest, as in Down syndrome, may manifest as peripheral cysts
Diffuse or focal lobar overinflation
In prenatal arrest, there are fewer alveoli than expected for gestational age with close approximation of the bronchi to the pleural surface
Postnatal arrest is characterized by airspace enlargement accentuated in subpleural and lobular areas with patchy overexpansion and collapse
Absolute increase in the number of alveoli, which are mildly enlarged
Remodeling after lung injury
Congenital lobar overinflation/emphysema
Abnormalities of lung growth, specifically pulmonary hypoplasia and pulmonary hyperplasia, largely reflect the influence of a developmental process or malformation that alters lung maturation. Distension of the lung with liquid and fetal respiratory movements is required for normal fetal lung growth, so any mechanism that interferes with these processes can result in a prenatal growth disorder. Prenatal-onset pulmonary hypoplasia ranges from mild to severe, depending on the mechanism of hypoplasia and timing of the insult in relation to the stage of lung development. Early insults that take place before 16 weeks’ gestation (renal anomalies, congenital diaphragmatic hernia) may interfere with airway branching, as well as acinar development, whereas later events (premature rupture of membranes) will exclusively affect acinar development. Because lung maturation continues well into the postnatal period, with most alveolarization occurring within the first year of a term birth, postnatal events can affect lung growth as well. Postnatal-onset growth abnormalities are commonly associated with premature birth (see “Complications of Prematurity and Its Therapy” ) and Down syndrome and, not infrequently, are seen in patients with congenital heart disease.
Like pulmonary hypoplasia, pulmonary hyperplasia, or excessive growth of the parenchyma, is a secondary phenomenon. During development it appears to be a response to airway obstruction, which blocks the outflow of fetal fluid leading to increased alveolar growth. Pulmonary hyperplasia has been also referred to as polyalveolar lobe and type 3 cystic adenomatoid malformation. The pathogenesis and clinical characteristics of this entity are related to congenital lobar overinflation/emphysema.
The majority of cases of pulmonary hypoplasia are secondary to congenital anomalies or pregnancy complications that affect amniotic fluid volume. Table 5.1 summarizes the most important conditions associated with prenatal pulmonary hypoplasia. The clinical profile and time of presentation are variable depending on the extent of hypoplasia and other anomalies.
| Oligohydramnios |
|
| Restriction of thoracic space |
|
| Decreased fetal breathing |
|
| Congenital heart disease with poor pulmonary blood flow |
|
| Syndromes and associations |
|
Pulmonary hyperplasia is most frequently seen in the setting of airway obstruction. When all lobes are affected, this malformation is typically associated with a developmental upper airway obstruction such as tracheal or laryngeal atresia. Obstructive lesions causing focal hyperplasia include bronchial atresia and stenosis. Extrinsic airway compression from a bronchogenic cyst or vascular anomaly could also result in a hyperplastic or overinflated lung lobe. Affected neonates usually present with dyspnea in early life.
Radiographic identification of late-onset pulmonary hypoplasia is often difficult. Secondary findings include spontaneous pneumothorax and pneumomediastinum. Pulmonary hypoplasia in Down syndrome may appear as peripheral cystic disease.
In pulmonary hyperplasia chest radiographs demonstrate progressive hyperinflation or hyperlucency of a lobe. Marked overinflation may lead to compression of the adjacent lung and mediastinum ( Fig. 5.1 ).

Grossly, the hypoplastic lung is small and the ratio of lung weight to body weight is lower than expected. Normal mean ratios are 0.018 for term infants (37–41 weeks), 0.025 for infants 28 to 36 weeks’ gestation, and 0.030 for infants 16 to 27 weeks’ gestation. In pulmonary hyperplasia, lungs are large, bulky, and often pale with normal lobation. It may affect all or some lobes.
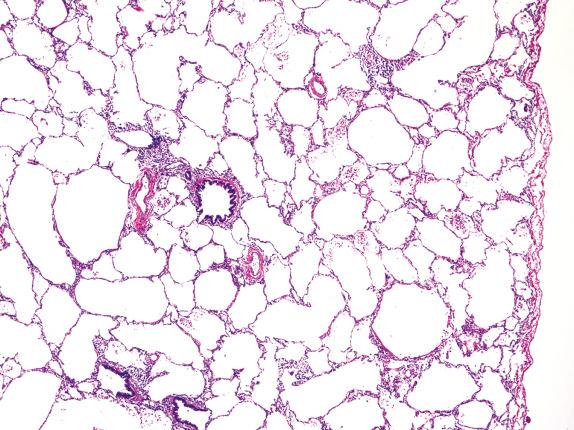
To define pulmonary hypoplasia, specific criteria have been devised that are based on reduced lung weight, lung volume, DNA content, and radial alveolar count. Although limited to the later stages of lung development (late saccular to alveolar) and well-inflated lung, the simplest method is the radial alveolar count, which measures complexity of the acinus. Radial alveolar count is the number of alveoli transected by a perpendicular line drawn from the center of a respiratory bronchiole to the nearest septal division or pleural margin. At least ten fields should be counted to offset bias due to differences between counts made from first-order and from third-order respiratory bronchioles. The radial count in a full-term infant should average five alveolar spaces and increases to approximately eight to ten alveolar spaces by 1 year of age. In pulmonary hypoplasia there is a reduction of alveolar spaces for gestational age, which is often accompanied by prominence of the bronchovascular structures and thickened interlobular septa. Widened alveolar ducts, enlarged airspaces, and dilatation of the subpleural alveoli that may resemble cysts characterize deficient alveolarization of postnatal onset ( Fig. 5.2 ).
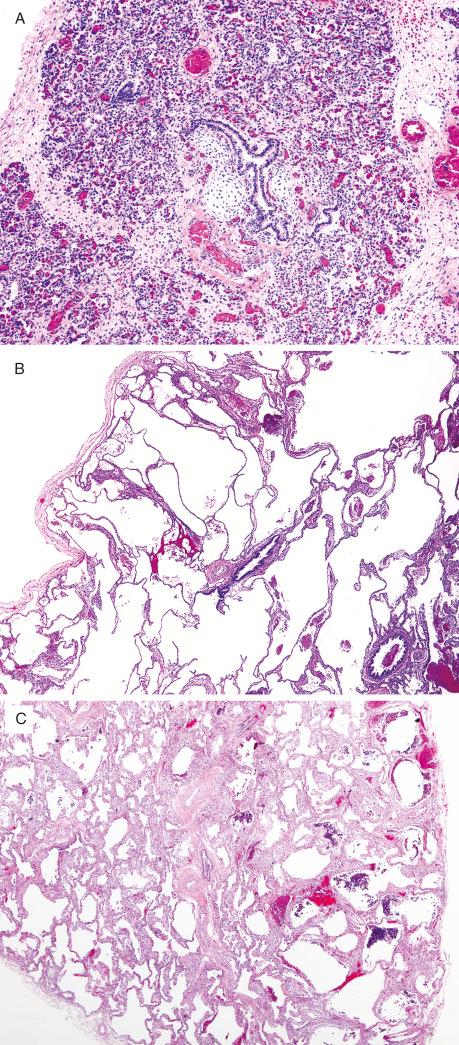
Pulmonary hyperplasia, diffuse or focal, is characterized by a striking increase in alveoli in relation to airways, which can be confirmed by the radial alveolar count. Alveoli are often abnormally enlarged and simplified, and there may be a decrease or absence of interlobular septa ( Fig. 5.3 ).
Due to the presence of alveolar enlargement, pulmonary hypoplasia is often misinterpreted as emphysematous change or remodeling after lung injury. However, unlike these conditions, in a growth abnormality there is no evidence of a destructive or reparative process, including inflammation, type II cell hyperplasia, and significant fibrosis.
Pulmonary hyperplasia should be distinguished from congenital lobar overinflation. In the latter condition, the volume increase is due to alveolar enlargement as opposed to an absolute increase in alveoli. Radial alveolar counts can be helpful for distinguishing between these two abnormalities.
Because prenatal-onset pulmonary hypoplasia is frequently associated with severe and irreversible lesions, it carries a poor prognosis. Survivors are at risk for the complications frequently seen in infants with prematurity, including pneumothoraces, PIE, and persistent pulmonary hypertension. In entities such as diaphragmatic hernia, right-sided hypoplasia has a worse prognosis than left sided, due to loss of more lung mass, more severe mediastinal shift, and great vessel displacement.
Pulmonary hyperplasia may be associated with in utero death due to compression of venous return to the heart and/or esophageal compression, resulting in polyhydramnios and fetal hydrops. The therapy for infants with lobar distension causing severe mediastinal shift and normal lung compression is surgical removal of the affected lobe or segment.
Idiopathic neonatal interstitial lung disease characterized by expansion of the alveolar walls by glycogen-laden mesenchymal cells
Rare, although recognition of the disorder is leading to identification of more cases
Preterm and term infants
May have a male predominance
Tachypnea and hypoxia usually presenting in the first few days to weeks of life
Unusual after 6 months of age
Pulmonary hypertension commonly coexists
Chest radiograph
Diffuse interstitial infiltrates or hazy opacities
Chest computed tomographic scans
No characteristic appearance
Favorable in the absence of an underlying lung disorder or other comorbid condition, including congenital heart disease
May be symptomatic for months, requiring supplemental oxygen
Short-term pulse steroids have been shown to be beneficial in limited case series
Variable proliferation of monomorphic spindle-shaped cells with indistinct cell borders and oval, bland nuclei in the alveolar walls
Spindle-shaped cells have vacuolated cytoplasm containing PAS-positive diastase-labile material, which may be difficult to demonstrate
Patchy distribution often associated with a growth abnormality
Hypertensive changes of pulmonary arteries are frequent when the lung is diffusely involved
Interstitial inflammation, fibrosis, and accumulation of alveolar proteinaceous material should be absent
Cells are always positive for vimentin, focally for smooth muscle actin
Cells are negative for desmin, CD45, CD68, and lysozyme
Interstitial mesenchymal cells with few organelles, which focally contain abundant monoparticulate glycogen
Some cells may contain drops of neutral lipid
Surfactant dysfunction disorders
Storage diseases
PIG, previously referred to as cellular interstitial pneumonitis, is a poorly understood entity seen exclusively in infants less than 1 year of age. The hallmark histologic feature of PIG is a variable proliferation of glycogen-laden mesenchymal cells within the alveolar septa. PIG may be an isolated disorder or a component of another preexisting congenital or neonatal condition. The disorder commonly occurs in the setting of a lung growth abnormality, such as chronic neonatal lung disease of prematurity and pulmonary hypoplasia, but may also be seen in the setting of pulmonary hypertension, meconium aspiration, PIE, and congenital lung malformations (eg, congenital pulmonary airway malformation). There is debate concerning the underlying etiology of this condition. Some authors propose that accumulation of immature mesenchymal cells within the interstitium may represent a selective delay or aberration in the maturation of pulmonary mesenchymal cells, whereas others suggest that this accumulation is a nonspecific feature of several conditions that transiently alter lung growth and development in the neonatal period.
PIG can occur in both preterm and term infants. Infants generally present in the first few weeks of life, not uncommonly in the first few days, with tachypnea and hypoxemia. Deteriorating respiratory function often occurs after an initial period of well-being, and patients may require mechanical ventilation and nitric oxide for respiratory failure and refractory pulmonary hypertension.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here