Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
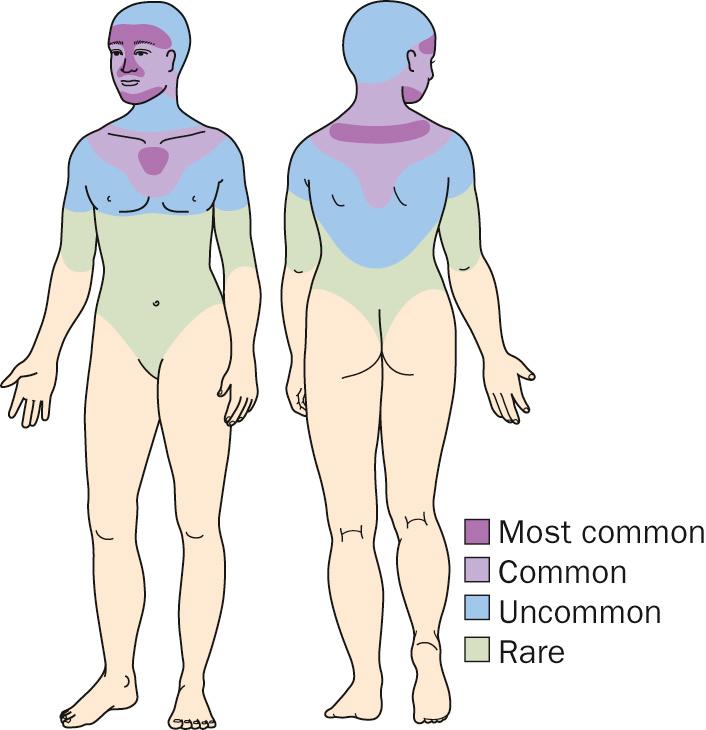
Acne is a papular or pustular eruption involving the face, chest, and back.
Acne may occur at any age but is more common in the teenage years and may persist well into adulthood.
Twenty percent of affected individuals develop severe acne resulting in scarring.
Acne can run in families, and those with a family history of acne often develop acne at an earlier age.
If both parents have acne, there is a 75% chance that a given child will develop acne.
Plugged follicles, increased sebum production, Propionibacterium acnes, and inflammation are thought to promote acne.
The role of diet in the pathogenesis of acne remains unclear, although consumption of dairy products and simple sugars has been implicated in some studies.
There are several variants of acne:
Steroid acne (papular and pustular acne on the face and torso 2 to 5 weeks after a steroid has been taken)
Neonatal acne (younger than 1 month of age)
Infantile acne (1 month to 1 year of age)
Acne necrotica (scarring scalp acne)
Acne excoriée (acne that has been manipulated by the patient, leaving erosions and scars)
Acne conglobata (severe cystic scarring acne on chest, back, and shoulders)
Consider a hyperandrogen state, such as congenital adrenal hyperplasia or polycystic ovarian syndrome.
Acne lesions are divided into noninflammatory and inflammatory lesions.
Noninflammatory lesions consist of open comedones (blackheads) and closed comedones (whiteheads).
Inflammatory lesions consist of red papules, pustules, nodules, and cysts.
Recurring rupture and re-epithelialization of cysts lead to epithelium-lined sinus tracks, often accompanied by disfiguring scars.
Eroded papules are seen in patients who pick acne papules (acne excoriée).
Patients with androgen excess can develop signs of virilism (thinning of scalp hair, hirsutism) and precocious puberty.
Rarely, acne occurs in association with fever, bone, and joint problems (acne fulminans).
Significant psychosocial issues may be present, including depression, anxiety, and social withdrawal.
Laboratory evaluation is indicated for female patients with persistent acne and evidence of a hyperandrogenic state (facial hair, muscle hypertrophy, irregular menses).
Tests include measurements for testosterone, follicle-stimulating hormone, luteinizing hormone, and dehydroepiandrosterone sulfate.
Bacterial and fungal cultures can be done to rule out infectious folliculitis.
Rosacea (flushing and blushing but no comedones)
Bacterial (gram-negative folliculitis) and yeast folliculitis (not typical on the face)
Keratosis pilaris (location more typical on the extensor upper arms)
Perioral dermatitis (comedones are not seen)
Men have more severe disease than women; men are less likely to seek early medical treatment.
Androgens can aggravate acne. It is important to ask about use of anabolic steroids, especially in athletes.
Acne flares may be seen during periods of stress, before menstrual periods, with certain medications (corticosteroids, lithium, anticonvulsants, antituberculosis medications, and iodides).
The propensity to form scars varies from patient to patient.
The redness and pigmentation after resolution of acne lesions may take many months to fade.
Patients often confuse red macules for scars (pseudoscars).
Areas where the skin is rubbed, such as under a hat or under a chin strap, may have accentuated acne (acne mechanica).
Acne occurs with variable severity. Sometimes only comedones appear; at other times cystic lesions predominate.
Acne usually begins between ages 10 years and 15 years and lasts for 5 to 10 years.
Children who require oral medications at an early age tend to have a more severe course.
Adult women can have chronic low-grade acne that can be challenging to manage.
Girls who develop a large number of acne lesions (noninflammatory and/or inflammatory) at an early age are likely to develop more severe acne.
Therapy should account for medical, financial, and psychosocial factors.
When possible, regimens should be simplified, using the fewest possible medications.
Decrease the risk for antibiotic resistance by limiting oral antibiotic therapy to 3 months and combining oral and topical antibiotics with benzoyl peroxide.
It takes at least 2 months for most topical medications to show their full effect, so patience must be exercised.
Most treatment is continual and prolonged because it is control—not cure—that is most often achieved.
A patient's propensity to scar should be determined. Patients who show evidence of scarring should be treated systemically and followed closely.
Isotretinoin should be considered if acne does not improve after 3 months of oral antibiotics. Patients with nodulocystic acne may be started on isotretinoin as initial therapy.
When managing acne, skin sensitivity and the presence of noninflammatory and inflammatory lesions should be considered.
The skin should be gently cleansed with a mild soap and tepid water.
Patients should be encouraged not to excessively scrub the skin.
Deep cleaning brushes are best used separately from drying exfoliating agents (e.g., salicylic acid, benzoyl peroxide, and retinoids).
Let the skin dry before applying topical agents.
Medications should be applied in a thin layer with a gentle message to acne-prone sites.
Patient should not apply medications to normal skin where acne lesions do not occur.
If the skin becomes red or dry, one should ensure that excessive medication is not being applied and the correct vehicle was chosen for the patient's skin type.
Solutions and gels are better for oily skin, whereas creams and lotions are better for dry skin.
Lower concentration medications are better for patients with sensitive skin.
Hair conditioners and oils should be avoided.
If cosmetics are used, they should be oil free and water based.
Patients should not pick or pop their acne lesions.
To avoid redness and dryness, retinoids should be applied 30 minutes after skin cleansing.
Agents that gently exfoliate the top layer of skin and have antibacterial properties (e.g., benzoyl peroxide) are used in combination with agents that correct follicular plugging (e.g., tretinoin, adapalene, tazarotene). One agent is usually applied in the morning and the other in the evening.

Prescription and over-the-counter products used for exfoliation contain sulfur, salicylic acid, resorcinol, and benzoyl peroxide.
There are many over-the-counter benzoyl peroxide gels, lotions, and creams, ranging in strength from 2.5% to 10%.
Retinoid medications (tretinoin, adapelene, and tazarotene) primarily affect follicular plugging and produce mild anti-inflammatory effects.
Patients should apply retinoids at night.
The following are the most commonly used retinoid preparations:
Tretinoin
Retin-A gel (0.025%, 0.01%)
Tretinoin cream (0.1%, 0.05%, 0.025%)
Retin-A micro (0.04, 0.08, 0.1%)
Avita cream and gel (0.025%)
Renova cream (0.02%)
Atralin gel (0.05%)
Tretin-X cream (0.025%, 0.0375%, 0.05%, 0.075%, 0.1%)
Veltin, Ziana (tretinoin 0.025% combined with clindamycin 1.2%)
Adapalene
Adapalene (Differin) 0.1% gel, cream, lotion, and 0.3% gel
Epiduo gel (adapalene−benzoyl peroxide 0.1%–2.5%)
Epiduo Forte (adapalene−benzoyl peroxide 0.3%–2.5%)
Tazarotene
Tazorac 0.05%, 0.1% gel and 0.5%, 0.1% cream
Fabior 0.1% foam
Adapalene, Renova, and Atralin cause less dryness and redness.
Adapalene is the least photosensitizing retinoid.
Tazarotene effectively removes comedones but can be very irritating. Applying the cream formulation or having the patient use the gel formulation and wash it off at increasing intervals (short contact therapy) may lessen irritation.
Tazarotene has a Pregnancy Category X warning.
Azaleic acid (Azelex) relieves follicular plugging and has antimicrobial activity.
Facial peels (glycolic acid, salicylic acid) effectively open plugged pores and should be considered for most patients.
Inflammatory acne is treated with antimicrobial agents in combination with retinoids and benzoyl peroxide.
Topical antimicrobial preparations include benzoyl peroxide, benzoyl peroxide antibiotic combinations (e.g., BenzaClin, Duac, Acanya, Onexton), and sulfur preparations (e.g., Klaron, Aczone).
Sulfacetamide and sulfur washes (e.g., AVAR, Plexion, Rosanil, Clenia) are effective and convenient.
Oral antibiotics should be started at higher doses and quickly tapered to minimize side effects.
Typical starting dosages are doxycycline 100 mg twice a day and minocycline 100 mg twice a day.
Maximal effect of an oral antibiotic is achieved after 2 months.
Oral antibiotics, with the exception of rifampin, are not thought to lower the contraceptive efficacy of oral contraceptives.
Photodynamic therapy and lasers have been used to treat inflammatory acne, but their use is limited by pain and expense.





Acne not responsive to intensive therapy with oral antibiotics and topical retinoids requires alternative therapy.
A small amount of triamcinolone (2.5 mg/mL) can be injected into individual cysts, but there is a risk for cutaneous atrophy.
Short courses of systemic corticosteroids improve acne, but acne has a tendency to flare after treatment. Prednisone 20 mg twice a day for 1 week can rapidly control severely inflamed cystic acne.
Oral contraceptives (e.g., Ortho Tri-Cyclen, Yaz, Estrostep, Beyaz) are beneficial for female patients with acne who desire contraception.
Spironolactone at doses of 25 to 100 mg twice daily improves acne in many women, especially adult women. Spironolactone may be taken with oral contraceptives, and pregnancy should be avoided.
Isotretinoin is the most consistent and effective treatment for acne. A clinical cure can be achieved in approximately 80% of patients with a cumulative dose of 120 to 150 mg/kg over 4 to 5 months.
For scarring, referral to a dermatologic surgeon is advisable only after the acne is quiescent for at least 1 year. This allows for maximal normal healing before any invasive procedure.
Red macules fade with time and are not true scars.
Some patients, especially if they have a dark complexion, develop light and/or dark macules that take many months or years to resolve and that are permanent in some patients.
Scars may be raised and thick (hypertrophic and keloid) or depressed (pitted or broad-based).
Treatments for pigment changes include hydroquinone, tretinoin, azelaic acid, chemical peeling, and laser resurfacing.
Treatment for acne scars includes excision, laser, dermabrasion, chemical peeling, injection with “fillers” (hyaluronic acid, collagen, others), and microneedling.
Intralesional corticosteroid (Kenalog 2.5–10 mg/mL) injections and application of silicone gel sheeting can be helpful for thick scars.
Alternative therapies (e.g. tree tree oil, oral supplements, maunka honey, tannis, fruit acids, brewers yeast) may be utilized by patients. Be sure to ask patients about their use, since they may be counter-productive with traditional therapies.
Patients with the possibility of an underlying endocrine abnormality should be evaluated in consultation with a dermatologist and an endocrinologist.
Patients with scarring acne or with acne that fails to respond to conventional treatment should be referred to a dermatologist.
Combination therapy is essential to successful management of acne.
Set realistic expectations with patients on the first visit, but be encouraging, and let patients know that acne therapy is extremely effective when used consistently and appropriately.
Neonates and infants can develop acne. Topical medicine is usually sufficient to control the acne; however, if recalcitrant inflammatory lesions or scarring is present, oral erythromycin or isotretinoin may be required.
Tetracycline, doxycycline, and minocycline should not be used in children younger than 12 years to avoid staining permanent teeth.










Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here