Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Fixation of acetabular components in total hip arthroplasty (THA) spans three phases: a transient, primary phase of fixation achieved in the operating room; an intermediate phase, which occurs only with cementless implants, in which new bone heals around the implant component; and a tertiary phase of secondary fixation in which the interface between implant and bone (cementless) or cement and bone (cemented) remodels as necessary to keep the implant well fixed.
Historically, acetabular components for THA were all fixed to the surrounding bone of the pelvis using bone cement as a mechanical grout.
Despite early failures, improvements in cementing technique and implant design led to improved long-term results such that, outside of North America, cemented acetabular fixation remains popular among THA surgeons.
Cementless fixation, the mainstay for acetabular components implanted in North America, evolved from unsatisfactory results with threaded and hydroxyapatite-coated components to biologic fixation using porous coatings to allow bone ingress.
Recently, the introduction of highly porous metals, some fabricated using additive manufacturing, has provided new means of designing the porous regions of acetabular components and increasing the coefficient of friction crucial to the initial phase of fixation.
Total hip arthroplasty (THA) was recently proclaimed “the operation of the century.” Its success and worldwide acceptance were built on the success and durability of the cemented low-friction arthroplasty introduced by Sir John Charnley in the 1960s. Charnley and other pioneers of THA initially fixed acetabular components to the pelvis with polymethylmethacrylate (PMMA) cement when replacing the hip, and the literature continues to demonstrate excellent performance with cemented acetabular cups. However, over the years, cementless acetabular fixation has gained popularity and become the primary fixation choice in the United States. Nonetheless, the choice of acetabular fixation method continues to vary among countries as reflected in annual reports from national registries. Different implant designs, materials, and fixation methods, both cemented and cementless, continue to be used, all with the goal of long-term survival rates by providing quality fixation of the acetabular component to the surrounding bone.
Adequate fixation is the stable mechanical joining of the acetabular component to the native acetabular bone such that no relative motion occurs at the interface between the implant and the bone. Regardless of the type of fixation (cemented or cementless), the fixation process can be divided into three phases similar to those described for femoral stem fixation. Primary fixation is achieved in the operating room when the acetabular component is held firmly against the bone with a grout (in the case of cement) or a mechanical press fit or with mechanical fixation (in the case of cementless components). However, this initial fixation stage is transient, with radiostereometric analysis (RSA) demonstrating that both cemented and cementless acetabular components migrate after implantation. With cemented implants, the fixation of the implant to the bone is strongest at the time of implantation and deteriorates over time. The second phase, intermediate fixation, which occurs only with cementless implants, begins with slight postoperative implant migration and continues as new bone heals around the implant component, leading to solid fixation. The intermediate phase ends when the bone around the implant is healed and remodeled, and no further migration or relative motion occurs. In the third and final phase, secondary fixation, the interface between implant and bone (cementless) or cement and bone (cemented) remodels as necessary to keep the implant well fixed.
The use of “bone cement” in arthroplasty was first proposed by the German surgeon Themistocles Gluck in 1891. He developed models for knee, hip, shoulder, elbow, ankle, and wrist arthroplasties. To secure these to bone, he experimented with bone cements made from materials such as copper amalgam, plaster of Paris, and stone putty (resin with pumice or gypsum). The use of PMMA as a bone cement was popularized by Charnley as part of his low-friction THA system in which a stainless steel stem and a polyethylene acetabular component were both fixed with PMMA. Charnley emphasized that PMMA does not act as an adhesive to the bone but rather as a grout, achieving fixation by intimately filling the gaps between the surfaces of the opposing implant and bone.
Successful long-term cemented acetabular fixation relies on an initially stable and secure fixation at the bone-cement interface to minimize micromotion. The creation of an extensive micro-interlock along the cement-bone interface is critical to avoid access to fluids entering the interface. These fluids can build damaging hydrostatic pressure when the joint is loaded and provide a migration path for wear debris from the bearing surfaces to be delivered to the bone along the interface.
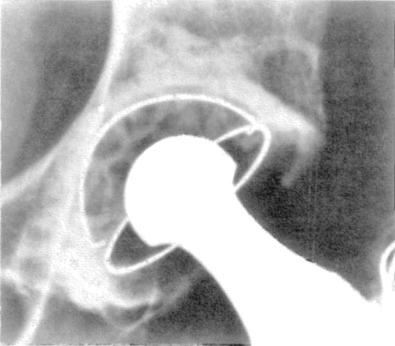
Optimal mechanical interlock at the bone-cement interface requires good cement interdigitation, obtained through adequate pressurization across the implant, cement, and bone. Penetration of bone cement into 3 to 5 mm of the cancellous bone creates a strong mechanical interlock. High cementation pressures and adequate preparation of the cancellous bone are needed to achieve this amount of penetration. Preparation of the acetabular bone bed is especially important ( Fig. 7.1 ). The subchondral bone plate should be removed, where possible, contrary to the so-called “second-generation” cementing technique theories popularized in the early 1980s. RSA studies show similar or better cup stability with subchondral bone plate removal compared with subchondral bone plate retention.
Cement penetration is also markedly influenced by the viscosity of the cement. Better penetration can be achieved with lower viscosity. However, at low viscosity, the cement is more difficult to handle, can leak around the acetabular rim during pressurization, and can escape more easily into the venous system instead of penetrating deeper into the bone. Better cement penetration is achieved with increased pressurization applied before cup insertion and in the early phase of cementation.
Today, we know that to achieve optimal interlocking fixation, the surgeon should remove the labrum with the surrounding osteophytes. The acetabulum should be decorticated, along with any cysts, to reveal trabecular bone. Bone graft should be used to fill cysts and on the medial wall to enhance fixation and to prevent cement extrusion under the transverse acetabular ligament. Multiple drill holes should be performed to maximize macro-interlock. The bone of the acetabulum is then washed with pulse lavage and packed with a swab soaked in saline or hydrogen peroxide to create a dry surface for cementing. Cement is introduced and pressurized until it is optimal for component implantation.
The importance of obtaining a good cement mantle around the acetabular component with no subsequent signs of radiolucency was highlighted by Ritter et al. They noted that postoperative radiolucency in DeLee and Charnley zone 1 following insertion of an all-polyethylene Charnley acetabular cup was highly predictive of component loosening ( Fig. 7.2 ), highlighting the importance of good surgical technique to create a strong, extensive interlock fixation. Bos et al. analyzed the cement-bone interface in postmortem retrieved cemented acetabular components. In 25 apparently well-fixed components, they found that the bone and cement were separated by a soft tissue membrane with the exception of some focal direct contacts between bone and cement. This membrane was thicker around acetabular components that had longer durations in vivo and contained abundant dense infiltrates of histiocytes, containing wear particles of cement and polyethylene. More details concerning PMMA in general and findings from postmortem bone-cement interfacial specimens are included in Chapter 4 .
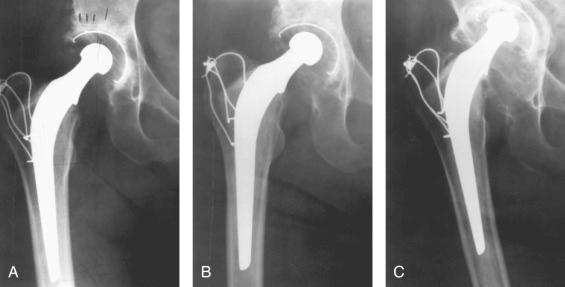
Several studies report excellent medium- to long-term survival rates of cemented acetabular components. Williams et al. reported a 97% survival rate free of aseptic loosening at 8 to 12 years follow-up using a cemented metal-backed cup. Despite satisfactory survival rates at 10 years, cemented fixation appears less secure during the second decade. Mulroy and Harris reported 15-year results with cemented implants and conventional polyethylene in younger patients with acetabular loosening occurring in 50% to 79% depending on implant design. However, in the same report, modern cementing techniques resulted in improved survival rates for metallic femoral stems.
Cemented acetabular components are also used in complex acetabular revision surgery. Regular polyethylene liners, constrained liners, and even dual-mobility components can be cemented into well-fixed metallic cementless acetabular shells. Biomechanical studies demonstrated fixation strength between the liner and shell comparable to that of modern locking mechanisms in conventional liner-shell constructs. However, the best fixation strength is achieved when the surfaces of both the shell and the liner are textured to maximize cement interdigitation and when the final cement mantle is at least 2 mm thick. In the case of massive acetabular bone defects, acetabular liners can be cemented during reconstructions with impaction bone grafting, with use of cages, highly porous jumbo cups (with and without acetabular augments), and custom triflange acetabular components.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here