Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The liver is a common site for both primary and metastatic oncologic disease. Primary hepatocellular carcinoma (HCC) has an annual incidence of 6 per 100,000 in the United States. Worldwide HCC is the second leading cause of cancer-related death in men and sixth leading cause in women. Furthermore, the worldwide incidence and number of deaths per year for HCC are nearly identical, highlighting the aggressive nature of the disease.
The liver is also the most common site for gastrointestinal (GI) tumor metastasis. Colorectal cancer is the third leading cancer cause of death in the United States. Approximately 15% to 20% of patients with colorectal cancer present with synchronous liver metastases, and approximately 50% will develop liver metastases at some point. There are limited data suggesting a role for liver-directed therapies in other metastatic GI tumors at this time, although there is some evidence that certain neuroendocrine and GI stromal tumors may also benefit from resection or ablation.
The first-line therapy for both primary and metastatic liver neoplastic disease is resection by partial hepatectomy or, in the case of select HCC, total hepatectomy and transplantation. The liver can tolerate extensive resection because of its regenerative capacity, but underlying liver disease and the presence of multiple lesions limit the number of candidates for this potentially curative therapy. Ablative therapies were developed to expand the number of patients amenable to treatment. The widespread use of ablative techniques has been limited by the lack of randomized trials comparing ablation to other therapies. Specifically, ablative techniques have not been directly compared with surgical resection in randomized trials, except in the treatment of small HCC lesions. All nonrandomized comparisons are limited by the variation in the definition of “unresectable.” Resection studies tend to find fewer unresectable tumors, and ablation studies tend to find more. These caveats make direct comparisons challenging.
This chapter will focus on the multitude of ablative treatment options. The most established is radiofrequency ablation (RFA). Newer strategies include microwave ablation (MWA), high-intensity focused ultrasound, irreversible electroporation (IRE), and percutaneous laser ablation. It will also touch on cryotherapy and percutaneous ethanol injection (PEI), which are used less frequently nowadays.
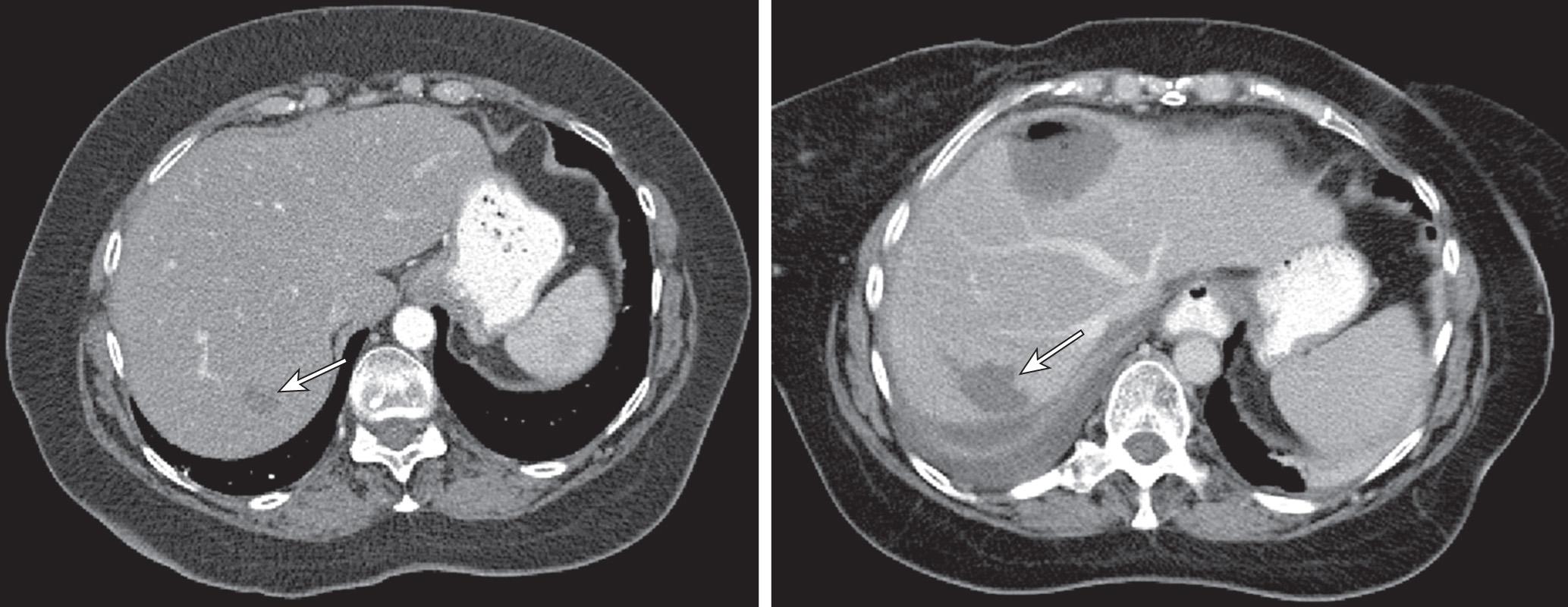
RFA is the most commonly used nonsurgical therapy for liver neoplasms. RFA can be performed open, laparoscopically, or percutaneously. RFA uses a needle electrode to deliver a high-frequency electrical current to generate heat, ultimately resulting in cellular necrosis. Fig. 126.1 shows the characteristic posttreatment appearance on computed tomography (CT) scan.
A major limiting factor for RFA efficacy is the proximity of target lesions to blood vessels, which function as a heat sink, result in smaller-diameter treatment areas, and can be a cause of persistent disease. Specifically, proximity to blood vessels larger than 3 mm has been shown to be an independent predictor of incomplete tumor ablation by RFA. The heat sink effect can be partially mitigated with either the Pringle maneuver or percutaneous balloon occlusion of a large hepatic or portal vessel, although the effect may only work in smaller tumors.
Controversy also exists over the best access method, percutaneous versus a surgical approach. Early studies showed lower recurrence rates with an open surgical approach. However, recurrence rates overlap broadly in different studies. The American Society of Clinical Oncology (ASCO) review of RFA concluded that there is insufficient evidence to resolve the issue of optimal approach. It may be advisable to avoid a percutaneous RFA approach if the stomach, duodenum, diaphragm, or transverse colon are in close proximity to one of the target lesions.
RFA is typically well tolerated. The mortality rate is 0% to 2%, and the major complication rate was 6% to 9%. Common complications included liver abscess, biliary leakage or stricture, hemorrhage, pleural effusion, pneumothorax, hypoxemia during treatment, and subcapsular hematoma.
Local recurrence rates were analyzed in a meta-analysis and found multiple contributing factors. Namely, tumor size greater than 5 cm, close proximity to a major vessel, subcapsular tumor location, intentional margin less than 1 cm, lack of vascular occlusion, and physician experience were all statistically significant predictors of local recurrence after RFA.
RFA has been extensively used either alone or combined with other therapies for localized HCC both as primary therapy and as a bridge to hepatic transplantation. The most important predictor of efficacy is size of the tumor(s) being treated. Complete radiographic response is seen in 80% to 90% of tumors less than 3 cm, as compared with 50% to 70% in lesions 3 to 5 cm in size. Table 126.1 shows representative series of patients with HCC treated with RFA. Five-year overall survival (OS) ranged from 47% to 76%, with complication rates of 1% to 12%.
| Author | Year | Patients | 1-Year Overall Survival (%) | 3-Year Overall Survival (%) | 5-Year Overall Survival (%) | Complications (%) | Incomplete Ablation (%) | Local Recurrence (%) |
|---|---|---|---|---|---|---|---|---|
| Wong * | 2013 | 76 | 87.3 | 61 | 48.6 | 4.7 | 17.5 | 24.7 |
| Wong † | 2013 | 100 | 92.8 | 68.7 | 47.2 | 4.7 | 15.4 | 29.4 |
| Shiina | 2012 | 1170 | 96.6 | 80.5 | 60.2 | 2.2 | 0.6 | 2.9 |
| Rossi | 2011 | 706 | — | 67 | 47.1 | 1 | 1.4 | 12.1% at 3 years |
| Livraghi | 2008 | 218 | — | 76 | 55 | 1.8 | 1.8 | 0.90% |
| Choi | 2007 | 570 | 95.2 | 69.5 | 58 | 1.9 | 3.3 | 11.8% at 3 years |
| Takahashi | 2007 | 171 | 98.8 | 91.1 | 76.8 | — | — | 17.7% at 3 years |
| Chen | 2006 | 71 | 95.8 | 71.4 | 64 | 4.2 | 4.2 | — |
| Tateishi | 2005 | 319 | 94.7 | 77.7 | 54.3 | — | — | 2.4% at 3 years |
| Lencioni | 2005 | 187 | 97 | 71 | 48 | — | — | 10% at 3 years |
| Raut | 2005 | 194 | 84.5 | 68.1 | 55.4 | 12 | 2.1 | 4.6 |
There have been several trials directly comparing RFA with primary surgical resection for HCC. In one large study of patients with HCC tumors less than 2 cm, OS was similar at 1 and 2 years (98% vs. 99% and 94% vs. 95%, respectively). However, disease-free survival was significantly higher in the surgery group at both 1 and 2 years (91% vs. 84% and 70% vs. 58%, respectively). More recently, a randomized trial between RFA and surgery in HCC tumors less than 4 cm found no statistically significant difference in OS or recurrence-free survival, although there was a trend toward the surgical group faring better. Another randomized trial of 230 patients who met the Milan criteria showed statistically improved overall and recurrence-free survival in the surgery group compared with RFA. At this point in time, patients who are surgical candidates and whose HCC is technically resectable should undergo surgical resection as first-line therapy.
RFA is also a viable option for recurrent HCC. Two representative series of patients with HCC recurrence after a liver resection treated with RFA found 1-year OS of 82% to 91.8% and 5-year OS of 38.2%.
Patients with isolated liver metastases from colorectal cancer deemed not to be surgical candidates also benefit from RFA. RFA has also been studied both with and in place of chemotherapy in these patients with a significantly improved progression-free survival (PFS) and OS. Table 126.2 shows a select series of larger patient cohorts treated with RFA for colorectal cancer metastases to the liver.
| Author | Year | Patients | 1-Year Overall Survival (%) | 3-Year Overall Survival (%) | 5-Year Overall Survival (%) | Complications (%) | Incomplete Ablation (%) | Local Recurrence (%) |
|---|---|---|---|---|---|---|---|---|
| Kennedy * | 2013 | 130 | 93.5 | 50.1 | 28.8 | 8.4 | — | 9.2 |
| Veltri † | 2012 | 248 | 93 | 62 | 35 | 7.3 | 0 | — |
| Solbiati ‡ | 2012 | 99 | 98 | 69.3 | 47.8 | 1.3 | 6.9 | 11.9 |
| Hammill § | 2011 | 101 | 87.6 | 52 | 33.1 | 2 | — | 11.9 |
| Siperstein | 2007 | 234 | — | 20.2 | 18.4 | — | — | — |
| Sorensen | 2007 | 102 | 96 | 64 | 44 | 10.9 | — | — |
| Machi || | 2006 | 100 | 90 | 42 | 30.5 | 4.8 (major) | — | 6.7 |
* Access was all laparoscopically.
† Median survival was 41 months if less than 3 cm and 21.7 months if greater than 3 cm.
‡ 10 years OS 18%. Fifty-four percent of locally progressive tumors were retreated with RFA and survival significantly improved compared with no retreatment.
§ Access was all laparoscopically. Patients with technically resectable disease had significantly longer OS but similar DFS.
|| Median survival was 48 months when RFA used as first-line treatment and 22 months when second-line or salvage therapy after failed chemotherapy.
There have been no randomized controlled trials comparing surgical resection to RFA for patients with potentially resectable liver metastases. Retrospective series have been done which show improved PFS and OS in patients in the surgical arm. Of note, in these and other similar studies, patients typically underwent RFA only if their disease was unresectable or if they were deemed poor operative candidates. Based on these and similar studies, both ASCO and a Cochrane review concluded that surgical resection should be favored over RFA in patients with potentially resectable liver metastases from colorectal cancer.
One interesting series compared 45 patients who received RFA with 39 who received systemic chemotherapy prospectively after a laparotomy revealed unresectable disease. There was a nonsignificant trend toward improved OS in the RFA group at both 2 years (56% vs. 51%) and 5 years (27% vs. 15%). There was also a significant improvement in quality-adjusted life years in the RFA group, which is an important outcome for oncologic patients.
A randomized trial of 119 patients with nonresectable colorectal cancer liver metastases between chemotherapy (FOLFOX ± bevacizumab) with or without RFA was done. In the 10-year follow-up, patients in the combination group had a significantly longer median survival (45.6 vs. 40.5 months) and 8-year OS (36% vs. 9%). A creative study compared the RFA arm of the above trial to the surgical arm of another prospective randomized trial, which randomized patients with metastatic colorectal cancer to surgery alone or surgery with neoadjuvant and adjuvant FOLFOX4. In comparing the two trials, the group found the local recurrence rate for surgery was 5.5% per lesion compared with 6.0% per lesion in their RFA group; the rate for RFA local recurrence of lesions smaller than 3 cm was 2.9%. Although this study is limited because the two sets of patients were different and the RFA trial had patients with, on average, more advanced disease, it does provide some preliminary evidence that RFA may provide similar local control for limited liver metastases compared with surgery when combined with systemic chemotherapy.
The benefit of RFA for regional treatment of liver metastases in patients with extrahepatic disease who are undergoing systemic chemotherapy remains uncertain, and this approach is not considered standard of care.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here