Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The diagnosis and management of abdominal sepsis is one of the great challenges the general surgeon faces. Optimal patient outcome requires considered decision-making and prompt action. However, even complex cases of abdominal sepsis can be managed confidently and competently by the application of basic principles. Up to 90% of general surgical mortality follows emergency admission with sepsis, yet there are few units where 90% of resource is targeted at non-elective work. Delay to definitive treatment is the single most common reason for adverse outcomes and anastomotic leak the single commonest complication in fatal cases. Given its frequency and severity, a sound understanding of abdominal sepsis should be integral to every general surgeon’s professional practice.
This chapter will address the diagnosis and management of abdominal sepsis, including patients treated in the intensive care unit, where management of abdominal compartment syndrome (ACS), the open abdomen and enterocutaneous fistulas (ECFs) can be particularly challenging. Intra-abdominal compartment syndrome is where intra-abdominal hypertension (IAH) leads to a spectrum of life-threatening pathophysiological changes and is often associated with sepsis. The reader is referred to Chapter 5 for a description of the intensive care management of the surgical patient, and to Chapter 6 for a discussion of surgical nutrition.
Sepsis is defined as life-threatening organ dysfunction caused by dysregulated host response to infection. This definition moves away from previous focus on the systemic inflammatory response syndrome (SIRS), which emphasised inflammation but is widely found in hospitalised patients who never develop infection. In the more recent definition, organ dysfunction is defined by the Sequential (Sepsis-specific) Organ Failure Assessment (SOFA) score: an increase by 2 or more points is associated with in-hospital mortality greater than 10%. An abbreviated score (quickSOFA) identifies patients with suspected infection at risk of poor outcomes typical of sepsis based on the presence of any two of the following:
respiratory rate ≥ 22 breaths/min;
altered mentation;
systolic blood pressure ≤ 100 mmHg.
Septic shock is defined as a subset of sepsis in which underlying circulatory and cellular metabolism abnormalities are profound enough to substantially increase mortality. Septic shock is identified by the requirement of vasopressors to maintain mean arterial pressure above 65 mmHg and a serum lactate greater than 2 mmol/L (18 mg/dL) in the absence of hypovolaemia. Septic shock is associated with hospital mortality of over 40%.
The healthy host response to bacterial invasion includes neutrophil- and macrophage-mediated release of proinflammatory mediators including cytokines, chemokines and nitric oxide at the site of infection (documented in standard texts). If this inflammatory response becomes generalised, systemic vasodilatation, increased vascular permeability and microcirculatory dysfunction with decreased capillary flow lead to hypotension, fluid transudation and ultimately tissue hypoxia. The resulting multiorgan dysfunction syndrome (MODS) is associated with high mortality. Once established, this downward spiral can become independent of the precipitating infective insult and is similar in conditions without initiating infection, such as major trauma, burns and pancreatitis.
The hypothesis that septic shock and MODS may be ameliorated by damping the exaggerated, uncontrolled inflammatory response has not been supported by clinical studies to date. Probably due to the complexity and redundancy of the many pathways involved, targeting a single mediator or even single pathway has had limited clinical success. The predominant current theories can be summarised as follows:
Uncontrolled systemic cytokine release. Uncontrolled or exaggerated release of cytokines from macrophages in response to cellular injury is proposed to initiate further mediator cascades resulting in neutrophil and platelet activation. There has been particular focus on the role of mediators believed to play a central role, including tumour necrosis factor alpha (TNF-α) and interleukins 1 and 6 (IL-1 and IL-6). However, the measured circulating levels of cytokines vary widely between studies and indeed within study populations. Clinical trials of drugs that inhibit the inflammatory cascade (corticosteroids, TNF-α antagonists and specific monoclonal antibodies) have failed to demonstrate a survival advantage. Individual randomised trials examining the clinical effectiveness of activated protein C in severe sepsis showed promising initial results, but a recent Cochrane review concluded no survival advantage, and this intervention has now been withdrawn.
Disturbances to coagulation. Activation of vascular endothelial cells by inflammatory mediators leads to a pro-thrombotic state, by alteration of both the coagulation and fibrinolytic systems. This can result in haematological failure with a consumptive coagulopathy resulting in disseminated intravascular coagulation (DIC). ,
Immunosuppression. Septic patients display features of immunosuppression including reduced capacity to clear primary infection and predisposition towards secondary infection with nosocomial pathogens. A number of mechanisms have been mooted—for example, reduced secretion of proinflammatory cytokines such as TNF-α, IL-1 and IL-6 in exchange for increased release of the anti-inflammatory cytokines IL-4 and IL-10 by T-helper cells may play a central role. This pattern of cytokine release has been observed in septic patients in the intensive care setting. , However, the possibility of immunotherapy to modify this host response has not yielded a therapeutic target to date.
There is an increasing awareness that chronic critical illness develops in a proportion of patients who survive the initial insult that led to the need for intensive care support but remain dependent on long-term organ support. This is characterised by prolonged need for ventilation and may be associated with polyneuropathy, myopathy, catabolism and prolonged delirium. Care for such patients is challenging and living with this condition may not be many patients’ choice.
Some degree of physiological derangement is common amongst surgical patients on the ward, although this is usually resolved by appropriate treatment of the underlying problem. When significant physiological derangement persists beyond 48 hours, progression to organ dysfunction is much more likely, an event associated with a mortality rate of up to 40%. Mortality, in general, increases with the number of organ systems affected and with the severity of physiological disturbance at onset. Early recognition of deterioration at a time when prompt intervention may yet avert catastrophe is essential. By the time the patient with abdominal sepsis has developed shock, mortality increases from less than 10% to over 50%. ,
It is critical to appreciate that deterioration can often start insidiously, and that early detection is vital as intervention is most successful at this stage. While there are objective criteria that define organ dysfunction as described above, clinical findings are helpful pointers. Hypoxia, oliguria, hypotension, deranged liver function tests or clotting, thrombocytopenia, acidosis and confusion are some of the features that indicate the beginning of a potentially severe systemic derangement.
The benefits of managing such high-risk surgical patients with early critical care input are well recognised. ,
![]() The importance of detecting the subtle signs of abdominal sepsis at an early stage cannot be overemphasised and while the rate with which organ dysfunction develops in individual patients will vary, the requirement for rapid identification and treatment is key.
The importance of detecting the subtle signs of abdominal sepsis at an early stage cannot be overemphasised and while the rate with which organ dysfunction develops in individual patients will vary, the requirement for rapid identification and treatment is key.
In 2008, informed by the results of a number of clinical trials, an international campaign was launched with the intention of improving outcomes in sepsis by standardising care. The emphasis of the campaign was timely identification and treatment of patients with severe sepsis, using goal-directed strategies. Evidence-based guidelines were published in 2004, split into ‘bundles’ of care to be accomplished within certain time frames ( Box 20.1 ). A total of 165 sites submitted bundle compliance and outcome data on 15 022 patients with severe sepsis. Despite incomplete compliance, a significant reduction in unadjusted hospital mortality (from 37% to 31% over the 2-year study period) was achieved in participating centres. The Surviving Sepsis Campaign (SSC) has continued to re-issue guidelines and remains active.
![]() The goal-directed treatment bundles developed by the Surviving Sepsis Campaign are a recommended standard of care. Their use in the timely identification and management of patients with severe sepsis has been shown to reduce mortality.
The goal-directed treatment bundles developed by the Surviving Sepsis Campaign are a recommended standard of care. Their use in the timely identification and management of patients with severe sepsis has been shown to reduce mortality.
To be accomplished within the first 6 hours of identification of severe sepsis:
Measure serum lactate
Obtain blood cultures prior to antibiotic administration
Administer broad-spectrum antibiotic, within 3 hours of A&E admission and within 1 hour for current inpatients
In the event of hypotension and/or a serum lactate > 4 mmol/L:
Deliver an initial minimum of 20 mL/kg of crystalloid or an equivalent
Apply vasopressors for hypotension not responding to initial fluid resuscitation to maintain mean arterial pressure (MAP) > 65 mmHg
In the event of persistent hypotension despite fluid resuscitation (septic shock) and/or lactate > 4 mmol/L:
Achieve a central venous pressure (CVP) of > 8 mmHg
Achieve a central venous oxygen saturation ( S cv o 2) > 70% or mixed venous oxygen saturation ( S v o 2 ) > 65%
To be accomplished within the first 24 hours of identification of severe sepsis:
Administer low-dose steroids for septic shock in accordance with a standardised ICU policy
Maintain glucose control > 70 but < 150 mg/dL
Maintain a median inspiratory plateau pressure (IPP) < 30 cmH 2 O for mechanically ventilated patients
Although effective management of patients with severe sepsis may entail complex investigations and procedures, the results of these manoeuvres are often suboptimal or even lethal without adequate prior resuscitation. A systematic approach such as that described in the Care of the Critically Ill Surgical Patient (CCrISP) course is recommended as it provides a common management structure for problems of any type or severity ( Fig. 20.1 ). Having a structured approach in times of crisis facilitates speed and reduces the likelihood of management errors. It certainly provides a common language and transparency that lets other health professionals understand the role of interventions, given that an integrated team approach involving diagnostic and interventional radiology, anaesthesia and intensive care is often required.
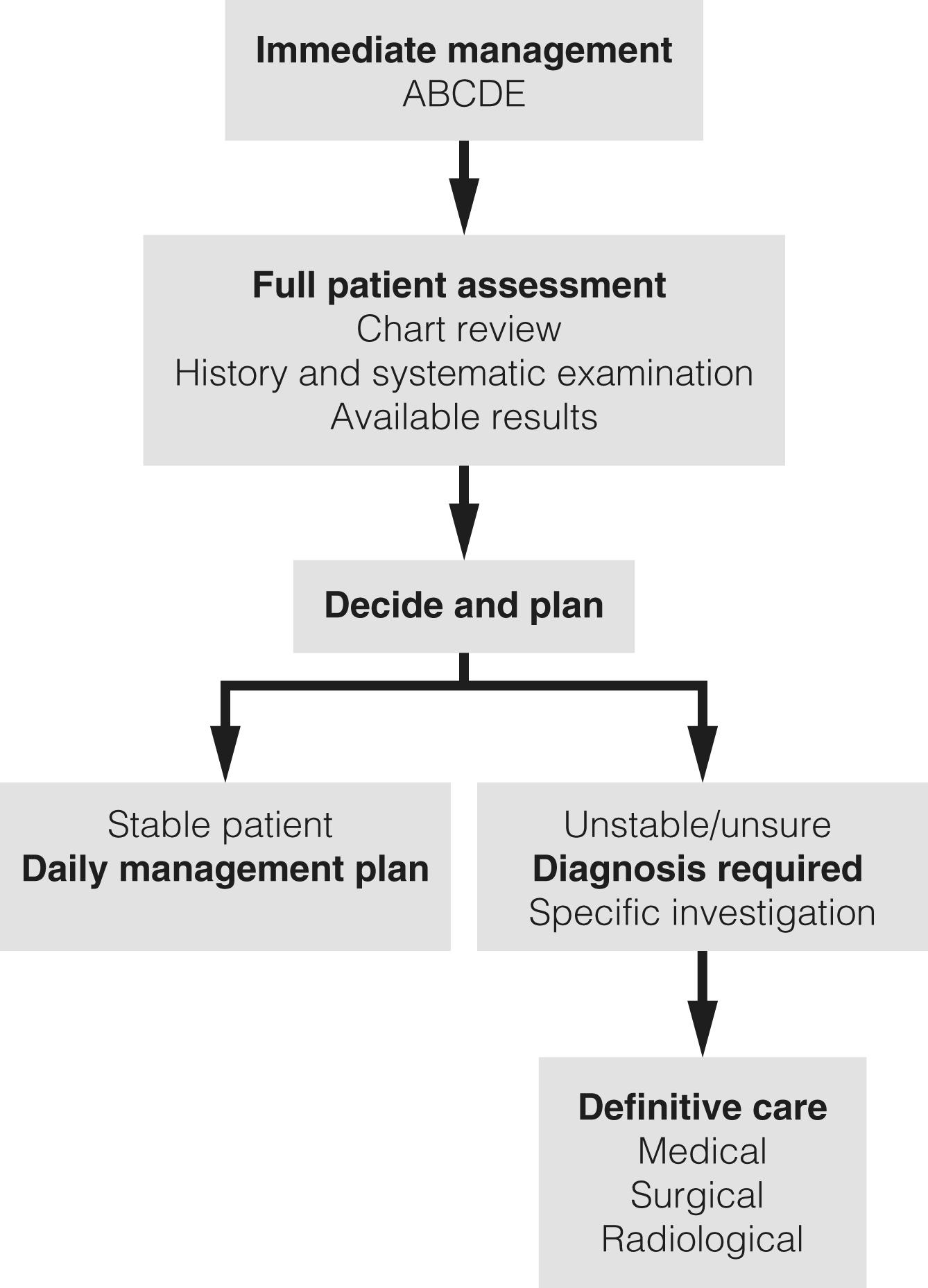
Patients with abdominal sepsis will inevitably have some degree of physiological instability. The CCrISP course advocates rapid immediate resuscitation following ABC principles of assessment with simultaneous correction of life-threatening conditions and initiation of high-flow oxygen therapy, intravenous fluids and monitoring as required. Some patients will deteriorate catastrophically and require intensive care support, but relatively simple interventions will commonly buy sufficient time for a comprehensive assessment. This assessment aims to determine the cause and severity of any problem and to exclude or optimise other conditions. A thorough review of the patient’s notes and charts is essential.
Complications can often be anticipated from the surgical condition in question, knowledge of any recent operative intervention and understanding of comorbidities ( Box 20.2 ). The range of possible diagnoses is often large ( Box 20.3 ) and the initial diagnostic net must be cast widely before drawing it in with the assistance of selective investigations. Reaching a provisional diagnosis and management plan rapidly is important as outcome worsens with delay.
Pyrexia or hypothermia
Tachycardia
Tachypnoea
Confusion
Oedema
Metabolic acidosis
Hypoalbuminaemia
Thrombocytopenia
Ileus
Poor peripheral perfusion
Hypotension
Hypoxia
Lethargy
Oliguria
Raised lactate
Hyponatraemia
Leucocytosis or neutropenia
Sepsis of other origin (urine, line, chest, etc.)
Cardiac (ischaemia, infarction, dysrhythmias, failure)
Cerebral (toxic confusion, ischaemia)
Pulmonary (atelectasis, collapse, infection, pulmonary embolism)
Fluid imbalance
Other non-septic abdominal complications (e.g. ileus, bleeding)
Patients should improve after clinical interventions. Failure to improve or signs of deterioration suggest a new problem or an incompletely treated initial one. The same systematic CCrISP approach forms the basis of ongoing assessment of the critically ill or at-risk patient on the critical care unit or ward. As repeated complications and setbacks are sadly common in complex cases, the surgeon must anticipate a long campaign rather than a single skirmish and be prepared to take a leading role in ongoing management.
Definitive management of abdominal sepsis requires eradication of the source of infection. However, antimicrobial therapy is also vital. Where sepsis is suspected, blood, vascular access sites, urine, wound and sputum should be sampled for urgent Gram staining and culture. Cultures from the main source of sepsis are several times more likely to be positive (75% vs 18%) than blood cultures, but both are important in the critically ill patient. Once samples for culture have been taken, broad-spectrum antibiotic therapy should begin immediately as delay may negatively influence the outcome. The role of cultures is to enable antibiotics to be changed selectively if the patient fails to respond to initial therapy. The choice of antibiotic will be influenced by the clinical circumstances and the expected range of infecting organisms. Early combination antibiotic therapy yields significantly improved survival compared with single-agent use in septic shock. The route of administration must ensure adequate plasma levels and the drugs should penetrate adequately into the tissues. Intravenous infusion is usually necessary. Whenever there is doubt concerning the optimal choice of antibiotics, the advice of a medical microbiologist should be sought. For most abdominal sepsis, coverage of Gram-negative and anaerobic bacteria will be necessary. With biliary sepsis, approximately 15% of cases will involve streptococci species that are resistant to cephalosporins, so the addition of a penicillin is a common approach. With hospital-acquired infection, cover against a broader and more resistant spectrum of organisms will be needed. Fungal infection (usually Candida species) is not uncommon in complex abdominal sepsis requiring ICU care and additional antifungal therapy will often be required and is something to be considered in a patient who is not responding to treatment.
![]() When severe sepsis is identified, blood cultures should be taken, and broad-spectrum antibiotics administered within 1 hour. This has been shown to reduce mortality as part of a management strategy in sepsis.
When severe sepsis is identified, blood cultures should be taken, and broad-spectrum antibiotics administered within 1 hour. This has been shown to reduce mortality as part of a management strategy in sepsis.
![]() Combination antibiotic therapy should be used in preference to monotherapy in septic shock as it is associated with a reduction in mortality.
Combination antibiotic therapy should be used in preference to monotherapy in septic shock as it is associated with a reduction in mortality.
A range of imaging techniques may be employed to localise an infective focus but computed tomography (CT) with intravenous contrast enhancement provides excellent information in thoracic, abdominal and pelvic sepsis. Consideration should be given to gastrointestinal contrast administration via mouth, nasogastric tube, drain, stoma or rectum. The vast majority of surgical patients can be stabilised sufficiently for scanning to take place safely and the guidance that CT provides in diagnosis and therapeutic intervention should not be underestimated. CT is excellent at primary diagnosis particularly in the complex or postoperative patient where clinical examination is more difficult. Comparison with previous scans is important and the input of an experienced, specialist radiologist is priceless. Modern hospital IT systems allow surgeons to look at scans themselves and routinely reviewing these images permits the surgeon to have more informed discussions. In emergency cases, the surgeon should ideally be present so that decisions about interventional radiological procedures may be made jointly.
Nevertheless, CT (or indeed any diagnostic test) is not perfect. Artefact from drains and metallic prostheses may reduce image quality. Intravenous contrast use is relatively contraindicated in acute kidney injury, although gastrointestinal contrast can still be used to advantage. Even in expert hands, there is a small rate of missed diagnoses and this is amplified in the interpretation of out-of-hours scans in complex postoperative patients.
The chest radiograph still plays a role in patient assessment and ultrasound has the advantage of being portable, harmless and repeatable. The greatest utility of ultrasound probably lies in assessment of biliary and renal pathology and monitoring identified collections. However, it is operator-dependent, and a negative scan will offer little reassurance when the clinical picture is concerning. When a focus of persistent sepsis cannot be identified on primary imaging, investigations such as magnetic resonance imaging particularly for biliary or pelvic pathologies or nuclear medicine modalities such as labelled white cell scanning may help identify occult sources of sepsis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here