Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The maintenance of a relatively constant volume and stable composition of the body fluids is essential for homeostasis. Some of the most common and important problems in clinical medicine arise because of abnormalities in the control systems that maintain this relative constancy of the body fluids. In this chapter and in the following chapters on the kidneys, we discuss overall regulation of body fluid volume, constituents of the extracellular fluid, acid–base balance, and control of fluid exchange between extracellular and intracellular compartments.
The relative constancy of the body fluids is remarkable, because there is continuous exchange of fluid and solutes with the external environment, as well as within the different body compartments. For example, fluid added to the body is highly variable and must be carefully matched by an equal output of water from the body to prevent body fluid volumes from increasing or decreasing.
Water is added to the body by two major sources: (1) it is ingested in the form of liquids or water in food, which together normally add about 2100 ml/day to the body fluids; and (2) it is synthesized in the body by oxidation of carbohydrates, adding about 200 ml/day. These mechanisms provide a total water intake of about 2300 ml/day ( Table 25-1 ). However, intake of water is highly variable among different people and even within the same person on different days, depending on climate, habits, and level of physical activity.
| Intake or Output | Normal | Prolonged Heavy Exercise |
|---|---|---|
| Intake | ||
| Fluids ingested | 2100 | ? |
| From metabolism | 200 | 200 |
| Total intake | 2300 | ? |
| Output | ||
| Insensible: skin | 350 | 350 |
| Insensible: lungs | 350 | 650 |
| Sweat | 100 | 5000 |
| Feces | 100 | 100 |
| Urine | 1400 | 500 |
| Total output | 2300 | 6600 |
Some water losses cannot be precisely regulated. For example, humans experience continuous water loss by evaporation from the respiratory tract and diffusion through the skin, which together account for about 700 ml/day of water loss under normal conditions. This loss is termed insensible water loss because we are not consciously aware of it, even though it occurs continually in all living people.
Insensible water loss through the skin occurs independently of sweating and is present even in people who are born without sweat glands; the average water loss by diffusion through the skin is about 300 to 400 ml/day. This loss is minimized by the cholesterol-filled, cornified layer of the skin, which provides a barrier against excessive loss by diffusion. When the cornified layer becomes denuded, as occurs with extensive burns, the rate of evaporation can increase as much as 10-fold, to 3 to 5 L/day. For this reason, persons with burns must be given large amounts of fluid, usually intravenously, to balance fluid loss.
Insensible water loss through the respiratory tract normally averages about 300 to 400 ml/day. As air enters the respiratory tract, it becomes saturated with moisture to a vapor pressure of about 47 mm Hg before it is expelled. Because the vapor pressure of the inspired air is usually less than 47 mm Hg, water is continuously lost through the lungs with respiration. In cold weather, the atmospheric vapor pressure decreases to nearly 0, causing an even greater loss of water from the lungs as the temperature decreases. This process explains the dry feeling in the respiratory passages in cold weather.
The amount of water lost by sweating is highly variable, depending on physical activity and environmental temperature. The volume of sweat normally is about 100 ml/day, but in very hot weather or during heavy exercise, fluid loss in sweat occasionally increases to 1 to 2 L/hour. This fluid loss would rapidly deplete the body fluids if intake were not also increased by activating the thirst mechanism, as discussed in Chapter 29 .
Only a small amount of water (100 ml/day) normally is lost in the feces. This loss can increase to several liters a day in people with severe diarrhea. Therefore, severe diarrhea can be life-threatening if not corrected within a few days.
The remaining water loss from the body occurs in the urine excreted by the kidneys. Multiple mechanisms control the rate of urine excretion. The most important means whereby the body maintains balance between water intake and output, as well as a balance between intake and output of most electrolytes in the body, is by controlling the rate at which the kidneys excrete these substances. For example, urine volume can be as low as 0.5 L/day in a dehydrated person or as high as 20 L/day in a person who has been drinking tremendous amounts of water.
This variability of intake is also true for most of the electrolytes of the body, such as sodium, chloride, and potassium. In some people, sodium intake may be as low as 20 mEq/day, whereas in others, sodium intake may be as high as 300 to 500 mEq/day. The kidneys have the task of adjusting the excretion rate of water and electrolytes to match the intake of these substances precisely, as well as compensating for excessive losses of fluids and electrolytes that occur in certain disease states. In Chapter 26, Chapter 27, Chapter 28, Chapter 29, Chapter 30, Chapter 31, Chapter 32 , we discuss the mechanisms that allow the kidneys to perform these remarkable tasks.
The total body fluid is distributed mainly between two compartments, the extracellular fluid and the intracellular fluid ( Figure 25-1 ). The extracellular fluid is divided into the interstitial fluid and the blood plasma .

There is another small compartment of fluid that is referred to as transcellular fluid . This compartment includes fluid in the synovial, peritoneal, pericardial, and intraocular spaces, as well as the cerebrospinal fluid; it is usually considered to be a specialized type of extracellular fluid, although in some cases its composition may differ markedly from that of the plasma or interstitial fluid. All the transcellular fluids together constitute about 1 to 2 liters.
In a 70-kg adult man, the total body water is about 60% of the body weight, or about 42 liters. This percentage depends on age, sex, and degree of obesity. As a person grows older, the percentage of total body weight that is fluid gradually decreases. This decrease is due in part to the fact that aging is usually associated with an increased percentage of the body weight being fat, which decreases the percentage of water in the body.
Because women normally have a greater percentage of body fat compared with men, their total body water averages about 50% of the body weight. In premature and newborn babies, the total body water ranges from 70% to 75% of body weight. Therefore, when discussing average body fluid compartments, we should realize that variations exist, depending on age, sex, and percentage of body fat.
In many other countries, the average body weight (and fat mass) has increased rapidly during the past 30 years. The average body weight for adult men older than 20 years in the United States is estimated to be approximately 88.8 kg (∼196 pounds), and for adult women it is 77.4 kg (∼170 pounds). Therefore, data discussed for an average 70-kg man in this and other chapters would need to be adjusted accordingly when considering body fluid compartments in most people.
About 28 of the 42 liters of fluid in the body are inside the trillions of cells and is collectively called the intracellular fluid . Thus, the intracellular fluid constitutes about 40% of the total body weight in an “average” person.
The fluid of each cell contains its individual mixture of different constituents, but the concentrations of these substances are similar from one cell to another. In fact, the composition of cell fluids is remarkably similar, even in different animals, ranging from the most primitive microorganisms to humans. For this reason, the intracellular fluid of all the different cells together is considered to be one large fluid compartment.
All the fluids outside the cells are collectively called the extracellular fluid . Together these fluids account for about 20% of the body weight, or about 14 liters in a 70-kg man. The two largest compartments of the extracellular fluid are the interstitial fluid , which makes up more than three-fourths (11 liters) of the extracellular fluid, and the plasma , which makes up almost one-fourth of the extracellular fluid, or about 3 liters. The plasma is the noncellular part of the blood; it exchanges substances continuously with the interstitial fluid through the pores of the capillary membranes. These pores are highly permeable to almost all solutes in the extracellular fluid, except the proteins. Therefore, the extracellular fluids are constantly mixing, so the plasma and interstitial fluids have about the same composition, except for proteins, which have a higher concentration in the plasma.
Blood contains extracellular fluid (the fluid in plasma) and intracellular fluid (the fluid in the red blood cells). However, blood is considered to be a separate fluid compartment because it is contained in a chamber of its own, the circulatory system. The blood volume is especially important in the control of cardiovascular dynamics.
The average blood volume of adults is about 7% of body weight, or about 5 liters. About 60% of the blood is plasma and 40% is red blood cells, but these percentages can vary considerably in different people, depending on sex, weight, and other factors.
The hematocrit is the fraction of the blood composed of red blood cells, as determined by centrifuging blood in a hematocrit tube until the cells become tightly packed in the bottom of the tube. Because the centrifuge does not completely pack the red blood cells together, about 3% to 4% of the plasma remains entrapped among the cells, and the true hematocrit is only about 96% of the measured hematocrit.
In men, the measured hematocrit is normally about 0.40, and in women, it is about 0.36. In persons with severe anemia , the hematocrit may fall as low as 0.10, a value that is barely sufficient to sustain life. Conversely, in persons with some conditions, excessive production of red blood cells occurs, resulting in polycythemia . In these persons, the hematocrit can rise to 0.65.
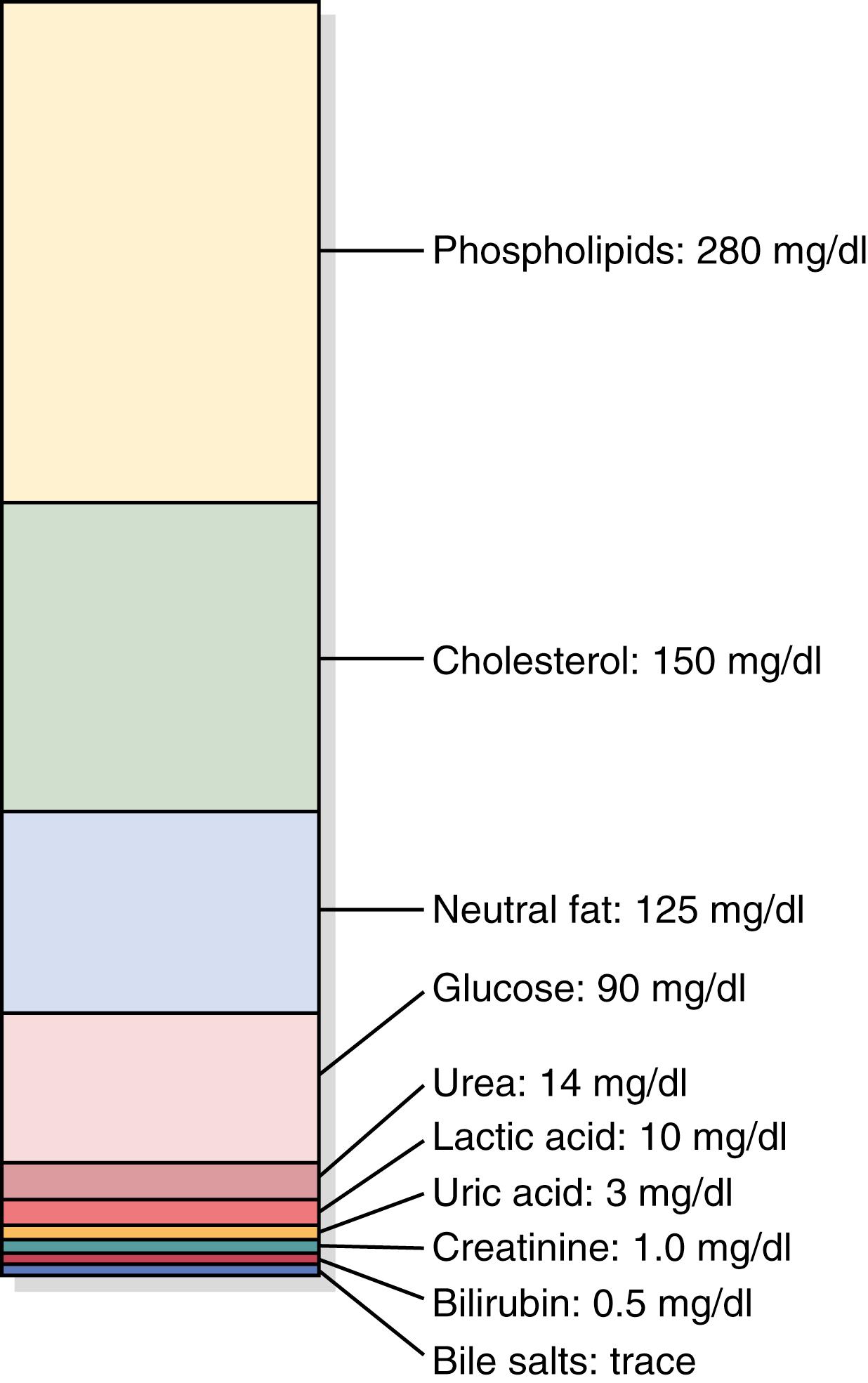
Comparisons of the composition of the extracellular fluid, including the plasma and interstitial fluid, and the intracellular fluid are shown in Figures 25-2 and 25-3 and in Table 25-2 .

| Substance | Plasma (mOsm/L H 2 O) | Interstitial (mOsm/L H 2 O) | Intracellular (mOsm/L H 2 O) |
|---|---|---|---|
| Na + | 142 | 139 | 14 |
| K + | 4.2 | 4.0 | 140 |
| Ca 2+ | 1.3 | 1.2 | 0 |
| Mg 2+ | 0.8 | 0.7 | 20 |
| Cl − | 106 | 108 | 4 |
| HCO 3 − | 24 | 28.3 | 10 |
| HPO 4 2− , H 2 PO 4 − | 2 | 2 | 11 |
| SO 4 2− | 0.5 | 0.5 | 1 |
| Phosphocreatine | 45 | ||
| Carnosine | 14 | ||
| Amino acids | 2 | 2 | 8 |
| Creatine | 0.2 | 0.2 | 9 |
| Lactate | 1.2 | 1.2 | 1.5 |
| Adenosine triphosphate | 5 | ||
| Hexose monophosphate | 3.7 | ||
| Glucose | 5.6 | 5.6 | |
| Protein | 1.2 | 0.2 | 4 |
| Urea | 4 | 4 | 4 |
| Others | 4.8 | 3.9 | 10 |
| Total mOsm/L | 299.8 | 300.8 | 301.2 |
| Corrected osmolar activity (mOsm/L) | 282.0 | 281.0 | 281.0 |
| Total osmotic pressure at 37°C (98.6°F) (mm Hg) | 5441 | 5423 | 5423 |
Because the plasma and interstitial fluid are separated only by highly permeable capillary membranes, their ionic composition is similar. The most important difference between these two compartments is the higher concentration of protein in the plasma; because the capillaries have a low permeability to the plasma proteins, only small amounts of proteins are leaked into the interstitial spaces in most tissues.
Because of the Donnan effect , the concentration of positively charged ions (cations) is slightly greater (∼2%) in plasma than in interstitial fluid. Plasma proteins have a net negative charge and therefore tend to bind cations such as sodium and potassium ions, thus holding extra amounts of these cations in the plasma, along with the plasma proteins. Conversely, negatively charged ions (anions) tend to have a slightly higher concentration in interstitial fluid compared with plasma because the negative charges of the plasma proteins repel the negatively charged anions. For practical purposes, however, the concentrations of ions in interstitial fluid and plasma are considered to be about equal.
Referring again to Figure 25-2 , one can see that the extracellular fluid, including the plasma and interstitial fluid, contains large amounts of sodium and chloride ions and reasonably large amounts of bicarbonate ions but only small quantities of potassium, calcium, magnesium, phosphate, and organic acid ions. The composition of extracellular fluid is carefully regulated by various mechanisms, but especially by the kidneys, as discussed later. This regulation allows the cells to remain continually bathed in a fluid that contains the proper concentration of electrolytes and nutrients for optimal cell function.
The intracellular fluid is separated from the extracellular fluid by a cell membrane that is highly permeable to water but is not permeable to most electrolytes in the body. In contrast to the extracellular fluid, the intracellular fluid contains only small quantities of sodium and chloride ions and almost no calcium ions. Instead, it contains large amounts of potassium and phosphate ions plus moderate quantities of magnesium and sulfate ions, all of which have low concentrations in the extracellular fluid. Also, cells contain large amounts of protein—almost four times as much as in the plasma.
The volume of a fluid compartment in the body can be measured by placing an indicator substance in the compartment, allowing it to disperse evenly throughout the compartment’s fluid, and then analyzing the extent to which the substance becomes diluted. Figure 25-4 shows this indicator-dilution method of measuring the volume of a fluid compartment. This method is based on the conservation of mass principle, which means that the total mass of a substance after dispersion in the fluid compartment will be the same as the total mass injected into the compartment.

In the example shown in Figure 25-4 , a small amount of dye or other substance contained in the syringe is injected into a chamber, and the substance is allowed to disperse throughout the chamber until it becomes mixed in equal concentrations in all areas. Then a sample of fluid containing the dispersed substance is removed, and the concentration is analyzed chemically, photoelectrically, or by other means. If none of the substance leaks out of the compartment, the total mass of substance in the compartment (Volume B × Concentration B) will equal the total mass of the substance injected (Volume A × Concentration A). By simple rearrangement of the equation, one can calculate the unknown volume of chamber B as follows:
For this calculation, one needs to know the following: (1) the total amount of substance injected into the chamber (the numerator of the equation); and (2) the concentration of the fluid in the chamber after the substance has been dispersed (the denominator).
For example, if 1 milliliter of a solution containing 10 mg/ml of dye is dispersed into chamber B, and the final concentration in the chamber is 0.01 mg/ml of fluid, the unknown volume of the chamber can be calculated as follows:
This method can be used to measure the volume of virtually any compartment in the body as long as the following occur: (1) the indicator disperses evenly throughout the compartment; (2) the indicator disperses only in the compartment that is being measured; and (3) the indicator is not metabolized or excreted . If the indicator is metabolized or excreted, correction must be made for loss of the indicator from the body. Several substances can be used to measure the volume of each of the different body fluids.
Radioactive water (tritium, 3 H 2 O) or heavy water (deuterium, 2 H 2 O) can be used to measure total body water. These forms of water mix with the total body water within a few hours after being injected into the blood, and the dilution principle can be used to calculate total body water ( Table 25-3 ). Another substance that has been used to measure total body water is antipyrine , which is very lipid-soluble, rapidly penetrates cell membranes, and distributes uniformly throughout the intracellular and extracellular compartments.
| Volume | Indicators |
|---|---|
| Total body water | 3 H 2 O, 2 H 2 O, antipyrine |
| Extracellular fluid | 22 Na, 125 I-iothalamate, thiosulfate, inulin |
| Intracellular fluid | (Calculated as total body water—extracellular fluid volume) |
| Plasma volume | 125 I-albumin, Evans blue dye (T-1824) |
| Blood volume | 51 Cr-labeled red blood cells, or calculated as blood volume = plasma volume/(1 − hematocrit) |
| Interstitial fluid | Calculated as extracellular fluid volume − plasma volume |
The volume of extracellular fluid can be estimated using any of several substances that disperse in the plasma and interstitial fluid but do not readily permeate the cell membrane. These include radioactive sodium, radioactive chloride, radioactive iothalamate, thiosulfate ion, and inulin. When any one of these substances is injected into the blood, it usually disperses almost completely throughout the extracellular fluid within 30 to 60 minutes. Some of these substances, however, such as radioactive sodium, may diffuse into the cells in small amounts. Therefore, one frequently speaks of the sodium space or inulin space instead of calling the measurement the true extracellular fluid volume.
The intracellular volume cannot be measured directly. However, it can be calculated as follows:
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here