Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Massive rotator cuff tears are often chronic in presentation and complicated by poor tendon quality, muscular fatty atrophy, tissue retraction, and scarring. For these reasons, successful footprint repair and tendon healing may be difficult and can result in retear rate of large-to-massive rotator cuff tears as high as 70% in the elderly and an approximate 45% retear in massive rotator cuff repairs in younger cohorts Known radiographic parameters for tear irreparability include acromiohumeral interval less than 7 mm, Goutallier grade 3–4 fatty infiltration of the infraspinatus, and a positive supraspinatus tangent sign. Approximately 10%–40% of all rotator cuff tears are massive. In the setting of irreparability, a number of surgical treatment approaches have been suggested.
There are multiple surgical treatment options for the irreparable rotator cuff tear. The patient’s age, integrity of the glenohumeral joint, extent of residual shoulder function, presenting symptoms, medical comorbidities, desired activity level, and rehabilitation requirements are all important considerations. An ideal treatment should include restoration of joint function and relief of pain. Although muscle transfer remains an option in the young, laboring patient, the demanding technical aspects of this procedure, relative perioperative morbidity, and unpredictable functional outcomes, particularly in older patients, limit the indications for this procedure.
Patch interposition (PI) and superior capsular reconstruction (SCR) have become the more commonly used reconstructive approaches Patch augmentation has also been used. Examples tried have included extracellular human, porcine, and synthetic grafts, as well as autografts using fascial and long head of biceps tendon autografts. In the absence of advanced cuff tear arthropathy, there is no clear indication for one reconstructive technique over another, and there is no standard treatment approach to this challenging clinical problem.
The treatment of the irreparable cuff tear remains a significant challenge to the shoulder surgeon. Historically, tendon transfers or shoulder hemiarthroplasty were limited goal treatment options. This option may work in older patients; however, in younger and active patients it may not give such good outcomes and may result in higher complications and reoperations rate than in older ones. Some authors suggest that Reverse Shoulder Arthroplasty (RSA) should be advocated in patients older than 65 years. This is one of the reasons why many new techniques are being investigated ( Figs. 7.1 and 7.2 ).
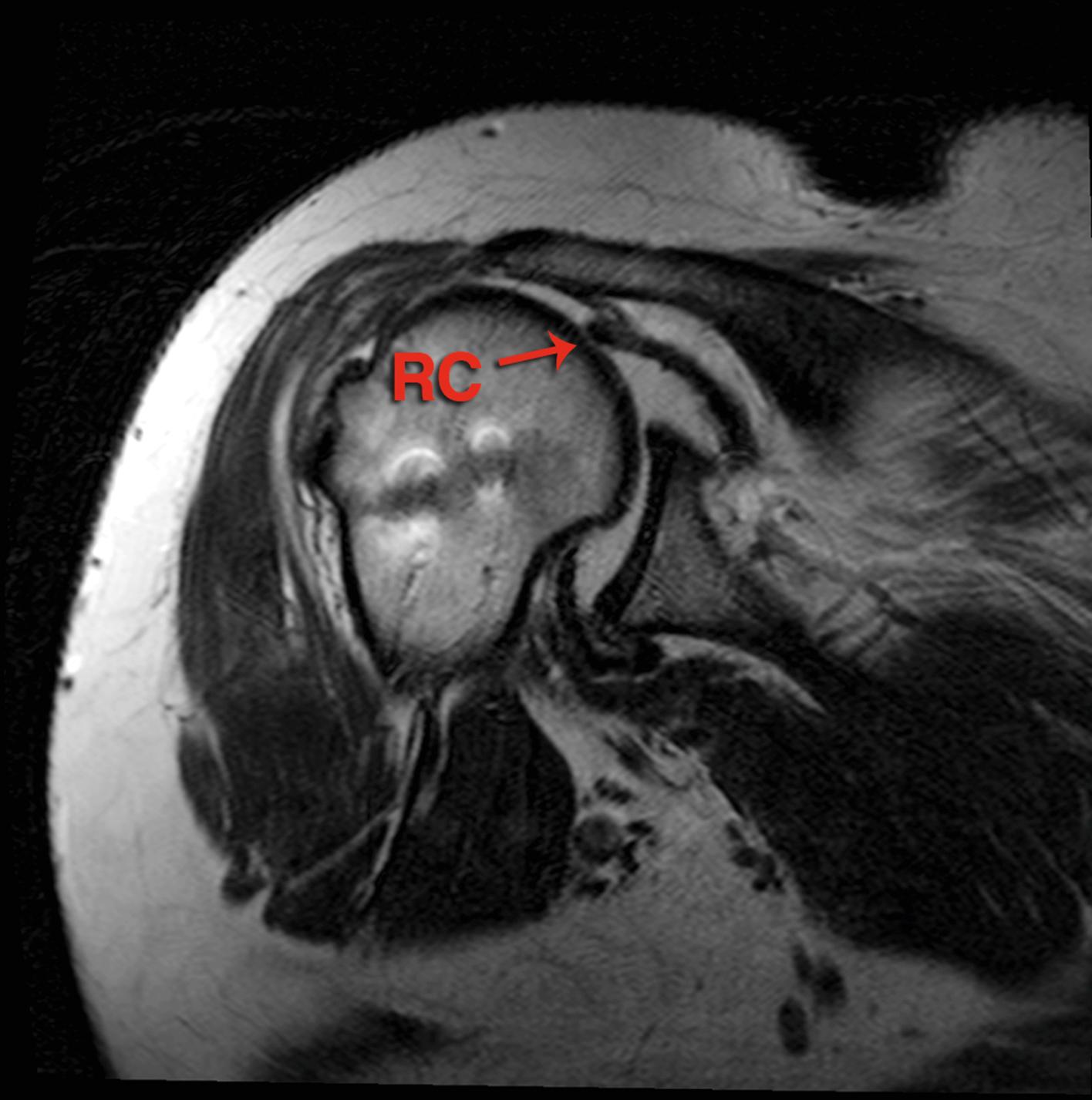
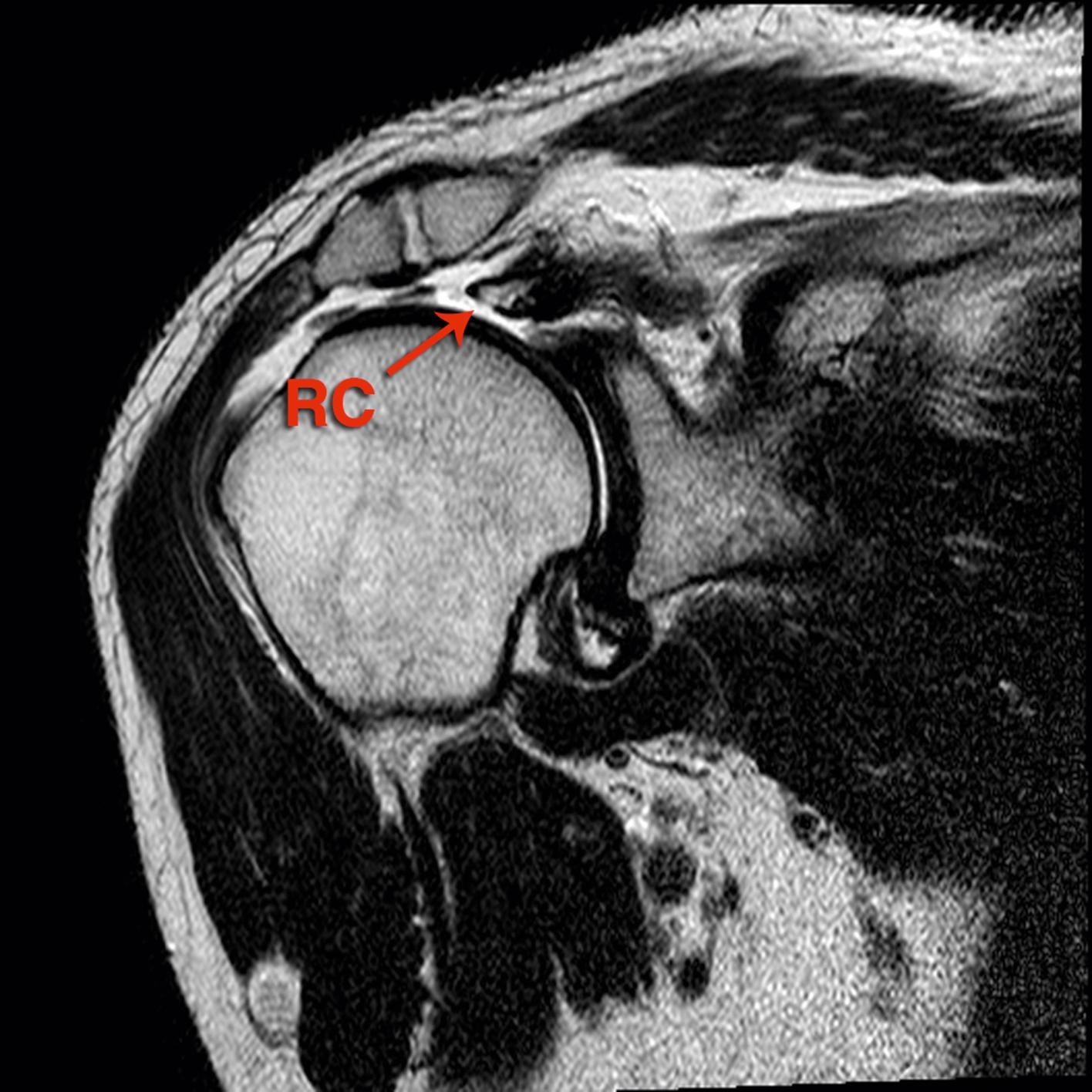
Some studies have evaluated treatment options for the massive irreparable rotator cuff tear in the setting of no or minimal osteoarthritis ( Fig. 7.3 ). The concept of implanting a patch or reconstructing the superior capsule is based on restoring the fulcrum for glenohumeral joint motions. The first reported approach was to fill the gap in irreparable cuff lesions with either biological or artificial grafts. There have been many clinical reports of different patch techniques published; unfortunately, high rate of retears have been also reported. This corresponds with our findings that almost 40% of patch grafts tore during follow-up; on contrary, only 17% reconstructed superior capsules were torn at the last follow-up visit. These results are supported by biomechanical work by Mihata et al. who reported that superior capsule reconstruction normalized superior stability of the shoulder, whereas patch grafts to the torn tendon only partially restored this stability.
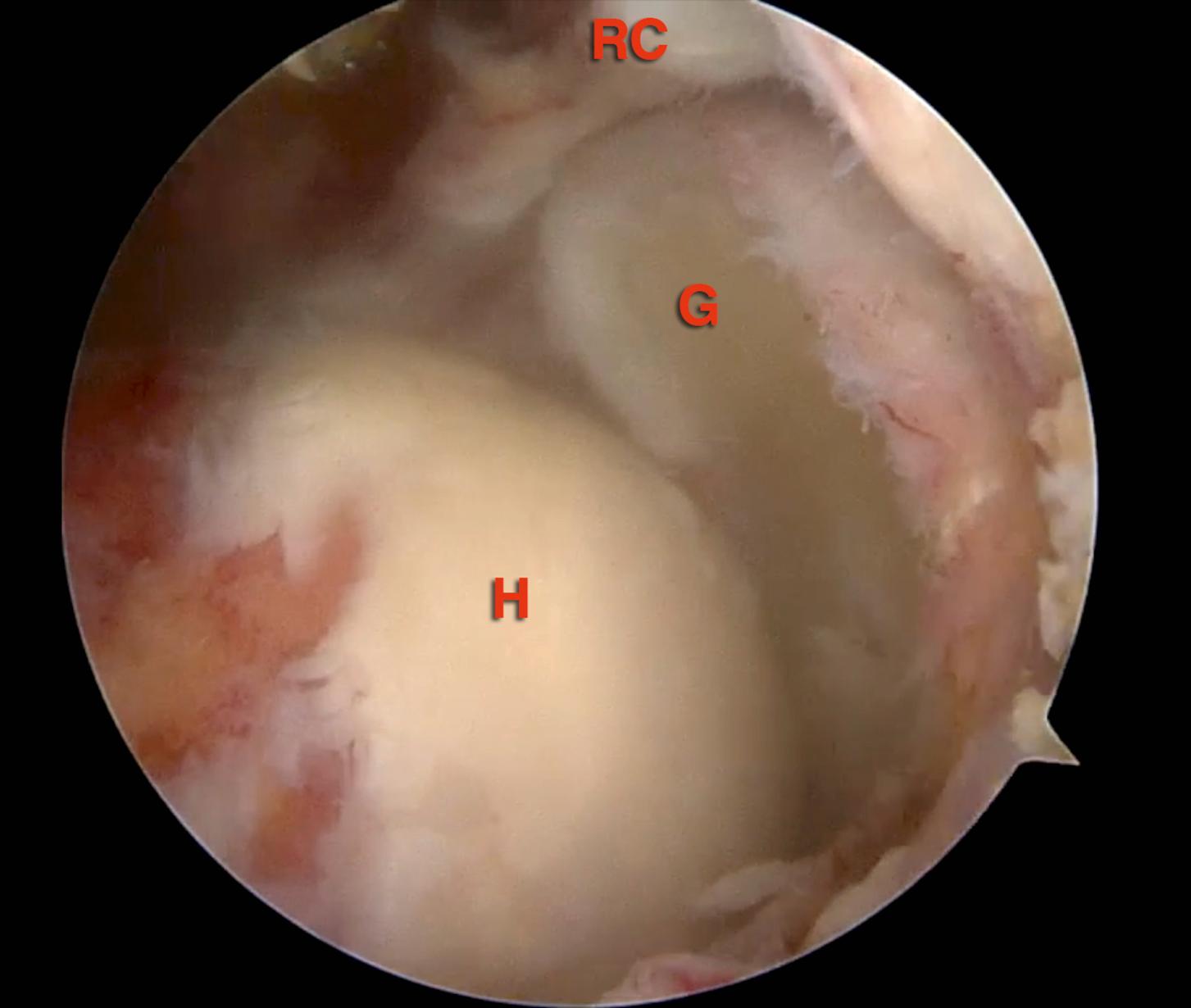
The concept of restoring glenohumeral biomechanics with patch techniques and capsule reconstruction was successfully tested on cadavers. This theory is supported in the published clinical outcome studies reported herein, in which in both groups, patch filling and SCR patients had a significant and comparable increase in their ranges of motion to around 150 degrees of flexion and around 40 degrees of external rotation (ER) ( Fig. 7.4 ).
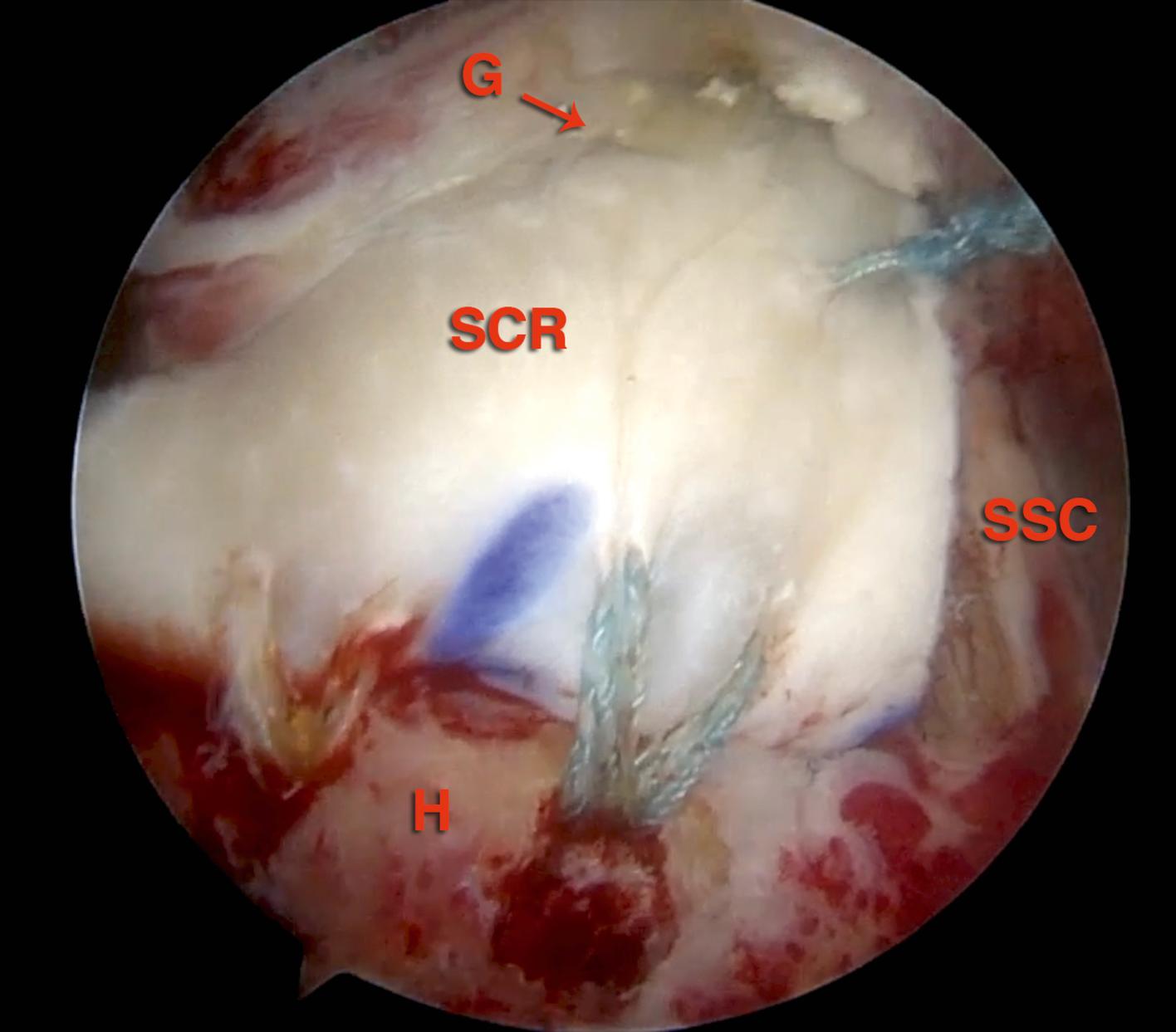
The published patient-reported outcomes did show that SCR is a promising solution. Postoperative change in American Shoulder and Elbow Society score (ASES) score for the SCR cohort was 70 points compared to 43 for patch interposition. Although direct comparisons between the cohorts are limited due to heterogeneity in reported outcome scores and measures, SCR reported more favorable range of motion and functional results than PI approaches. One potential explanation for this finding is the higher graft retear rate in the PI group than in SCR. Admittedly, the complication rate for SCR may prove to be higher with additional outcome studies and length of follow-up.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here