Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The management of rectal cancer has changed dramatically in the last 5 years. Review of national databases has clearly outlined the wide variations in overall survival rates, rates of local recurrence, and rates of permanent colostomies. Championed by many in Western Europe, most notably by Drs. Quirk, Heald, and Brown, the multidisciplinary treatment of rectal cancer has been shown to result in significant improvement in all aspects of care. Because of these continued advances this process is rapidly gaining acceptance in the United States. The multidisciplinary team (MDT) approach is recognized by the OSTRiCh consortium, the American Cancer Society, and the American College of Surgeons Commission on Cancer, the latter of which has devised pilot programs that have adopted practices considered essential for certification for centers of excellence. Beyond the development of the MDT, the area of care that has provided the most dramatic change in rectal cancer care has been magnetic resonance imaging (MRI) refinement for rectal cancer evaluation. Accurate local staging and restaging is increasingly possible, with the ability to better avoid the over- or undertreatment of cancer, thereby achieving optimal oncologic outcomes while preserving quality of life. MRI has now largely replaced endorectal ultrasound in the evaluation of local staging. MRI is able to accurately define the T category, (to quantify depth of invasion), the extramural venous invasion (EMVI), the circumferential radial margin (CRM) status, the peritoneal reflection position relative to tumor positions in the rectum, and the lymph node involvement. In addition, MRI is becoming an integral part of evaluating postneoadjuvant staging and guiding potential “watch and wait” strategies. This chapter will address the use of MRI in initial staging, postneoadjuvant restaging, and for recurrent disease.
MRI is now an essential component of the management of rectal cancer. Indications for MRI are focused on the initial evaluation and staging of rectal cancer, the former arising as the standard of care. Restaging rectal cancer following neoadjuvant therapy is a key component in identifying surgical strategies, especially when there are threatened margins noted on pretreatment staging examinations. MRI is now considered essential in determining decisions related to “watch and wait” strategies and is the preferred follow-up imaging for these patients. However, MRI is not routinely used in surveillance follow-up after definitive management, unless surgical complications arise, such as fistula, or in cases of recurrent tumor to guide further possible surgical management. Although the incidence of local recurrence is now less than 5%, MRI has been invaluable in defining the extent of recurrence and determining resectability. When resection is considered, MRI has demonstrated value in predicting negative margins.
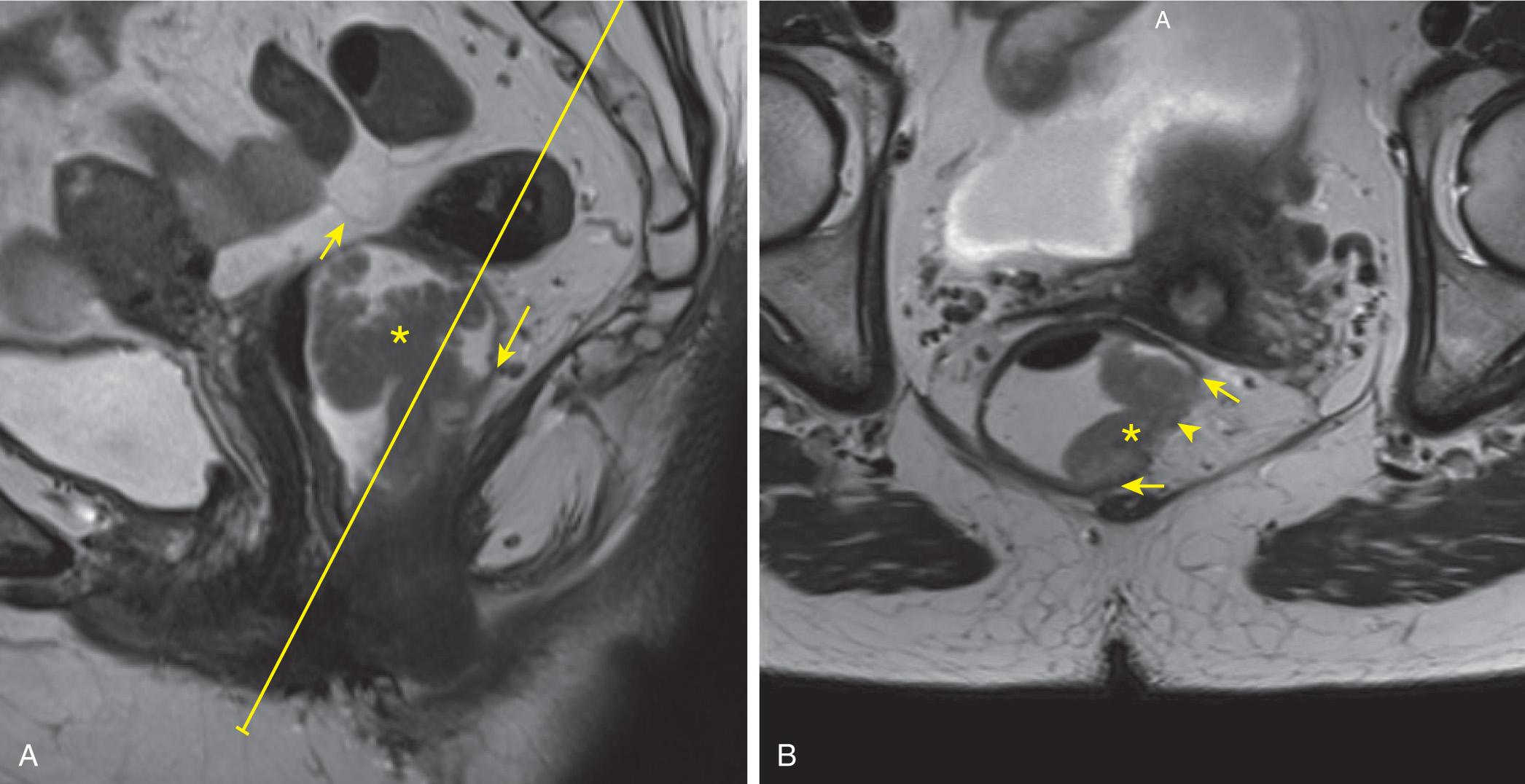
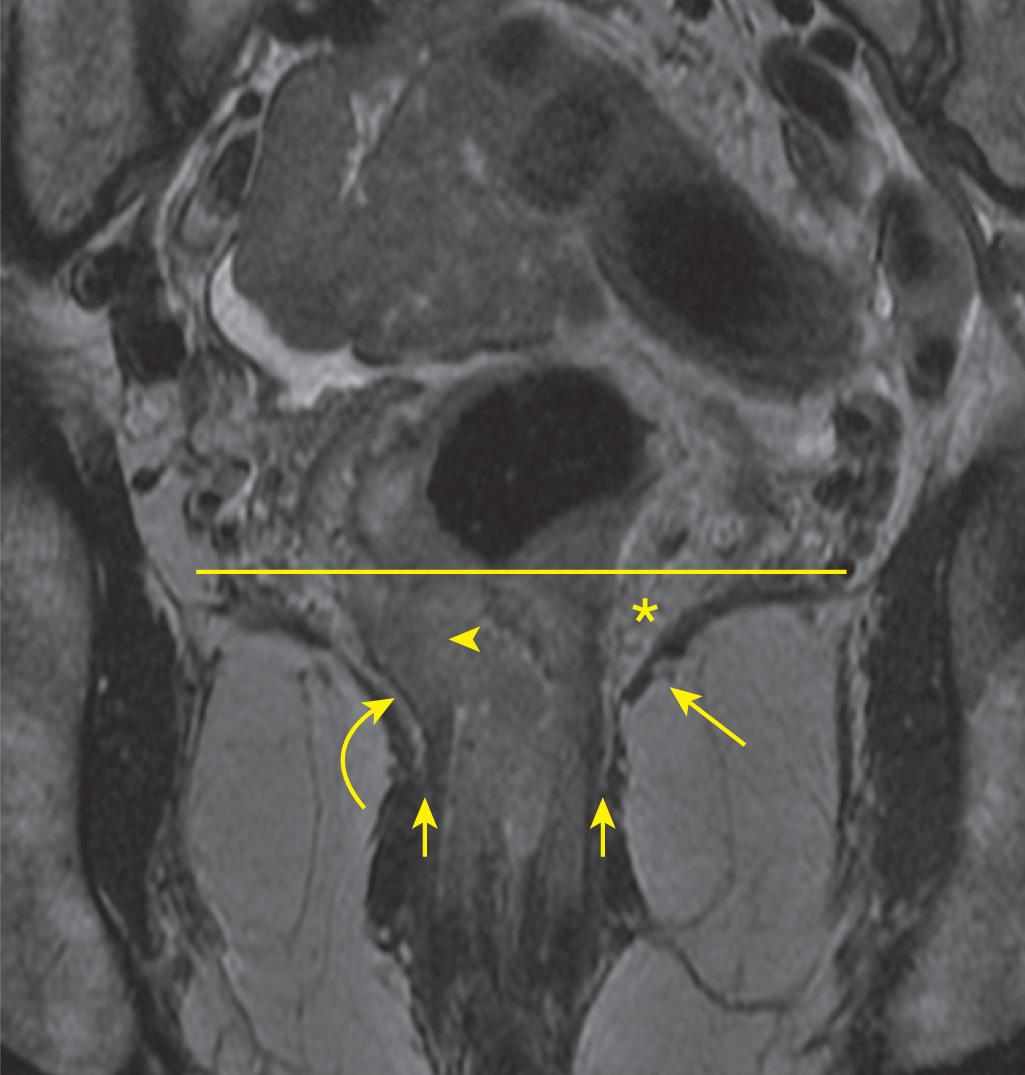
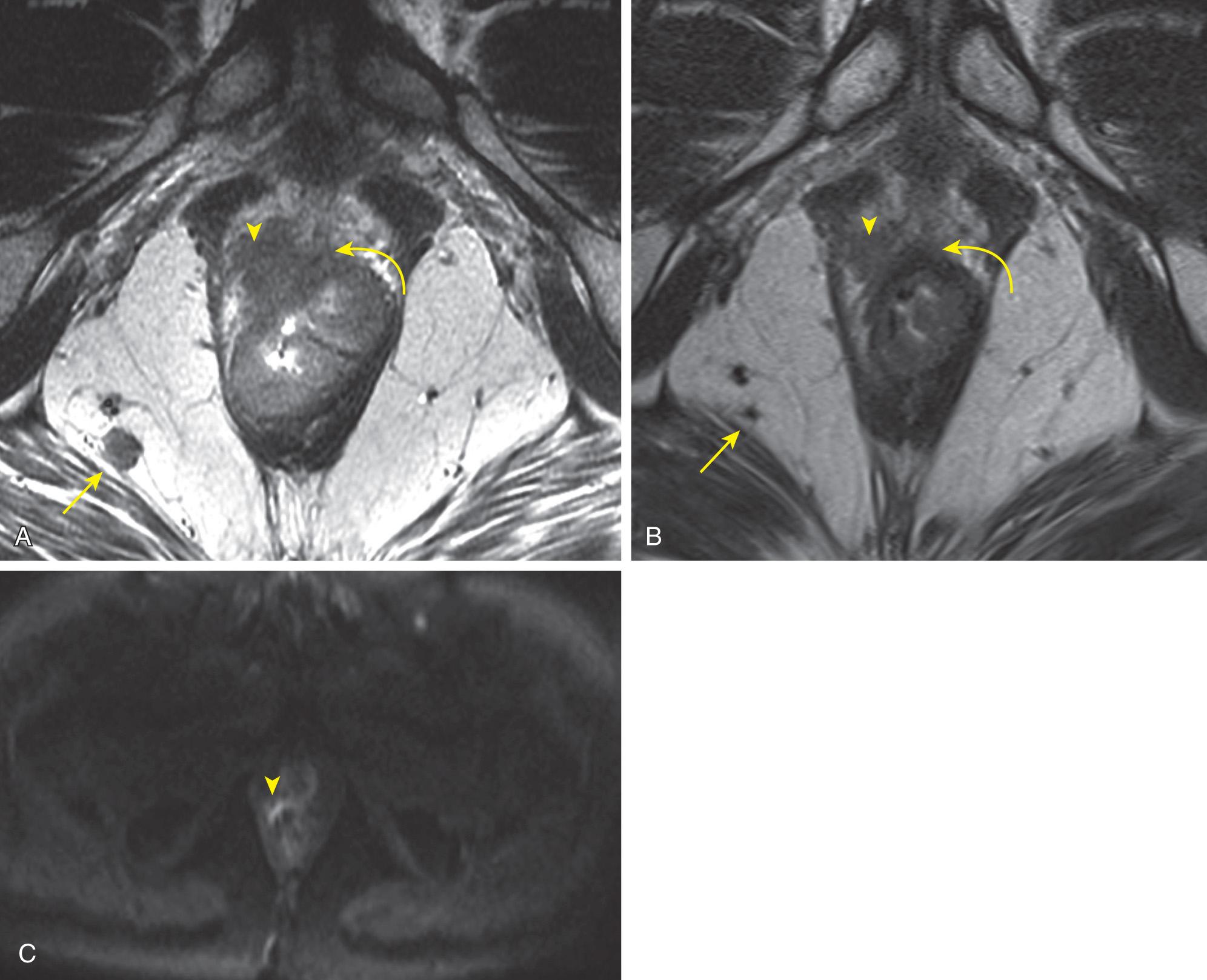
A standardized protocol has been validated and can be referenced in the MERCURY experience, the foundation being high-resolution small field-of-view (FOV) T2 images perpendicular to the long axis of the rectum. The angles of the axial oblique slices are determined from sagittal images of the tumor with annotation by the radiologist for the technologist ( Fig. 146.1A ). This angulation allows for precise determination of the tumor with origin from the rectal wall (see Fig. 146.1B ). MRI is not used as a screening exam for rectal cancer. The precise angulation of the slices is predicated on the knowledge of the exact tumor location, including the distance from the anal verge, tumor morphology, and radial location discovered on endoscopy or physical exam; thus, this location must be available at the time the exam is performed. Acquisition and interpretation of MRI exams without foreknowledge of tumor location may result in both understaging and overstaging lesions. For example, in the case of low rectal tumors, in addition to the standard imaging evaluation, an additional image series coronally oriented with respect to the anal canal is obtained to accurately assess the tumor's relationship to the sphincteric complex and intersphincteric plane ( Fig. 146.2 ). MRI exams may be performed on a 1.5 or 3 T MRI scanner; neither one is proven to demonstrate superiority. Recommended protocols for scanners from various manufacturers are available on the website of the Society of Abdominal Radiology.
Of note, the technique does not include the use of intravenous (IV) contrast. Based on the initial experience at our institution, IV contrast creates a tendency to overstage rectal tumors. Importantly, fat saturation techniques on T2 imaging, which are commonly used when evaluating most pelvic pathology, are to be avoided when performing exams for routine staging and restaging rectal cancer. These fat saturation techniques preclude accurate assessment of the tumor in relation to the mesorectal fascia and peritoneal reflection. To decrease motion artifact related to bowel peristalsis, antispasmodics are routinely given, typically glucagon (1 mg) in the United States, although buscopan is given in much of Europe. This medication may be given intramuscularly or IV just prior to the start of the examination. Glucagon is not given if there is a patient history of pheochromocytoma or glucagon allergy. The drug has been given in patients with diabetes mellitus.
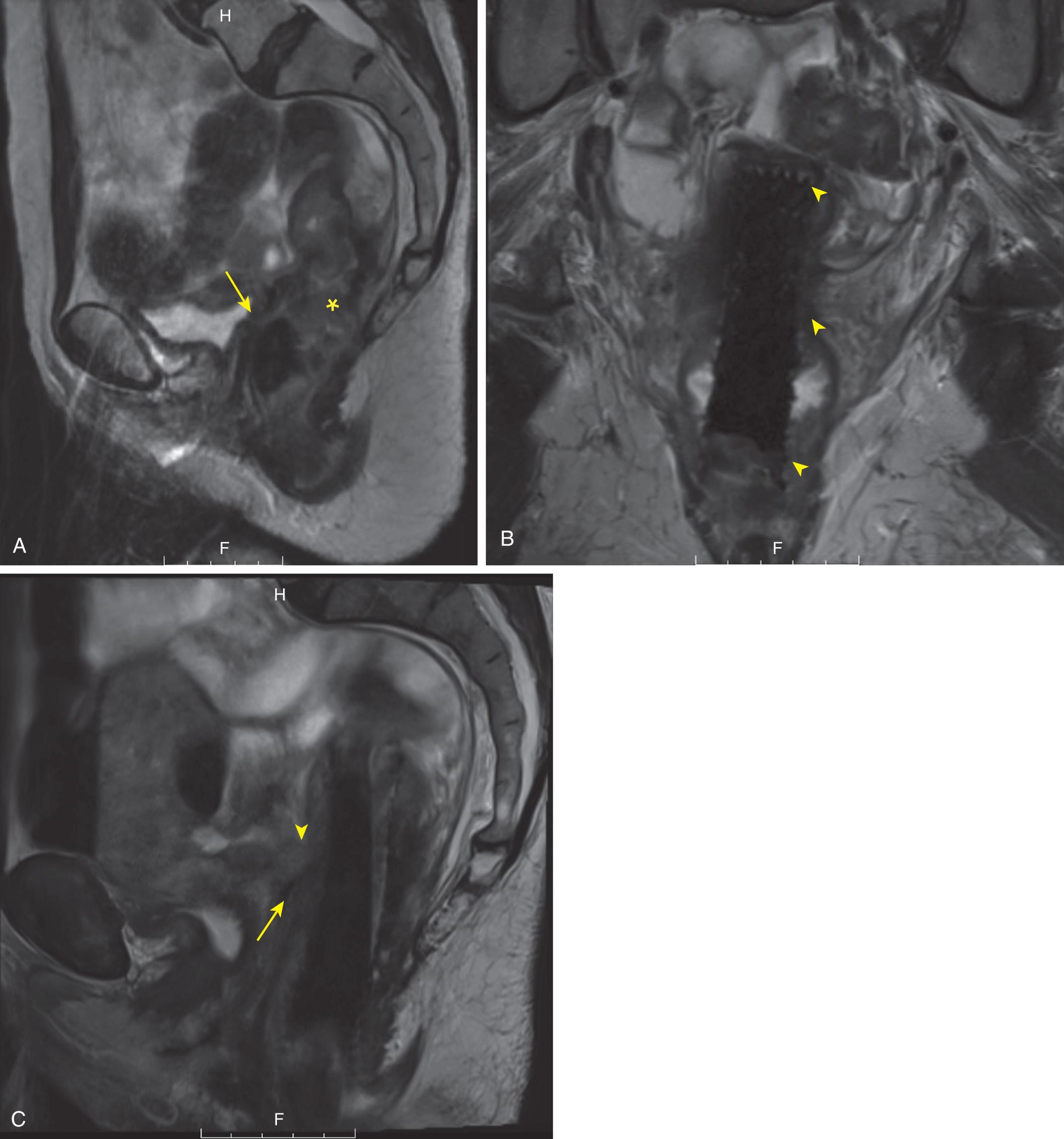
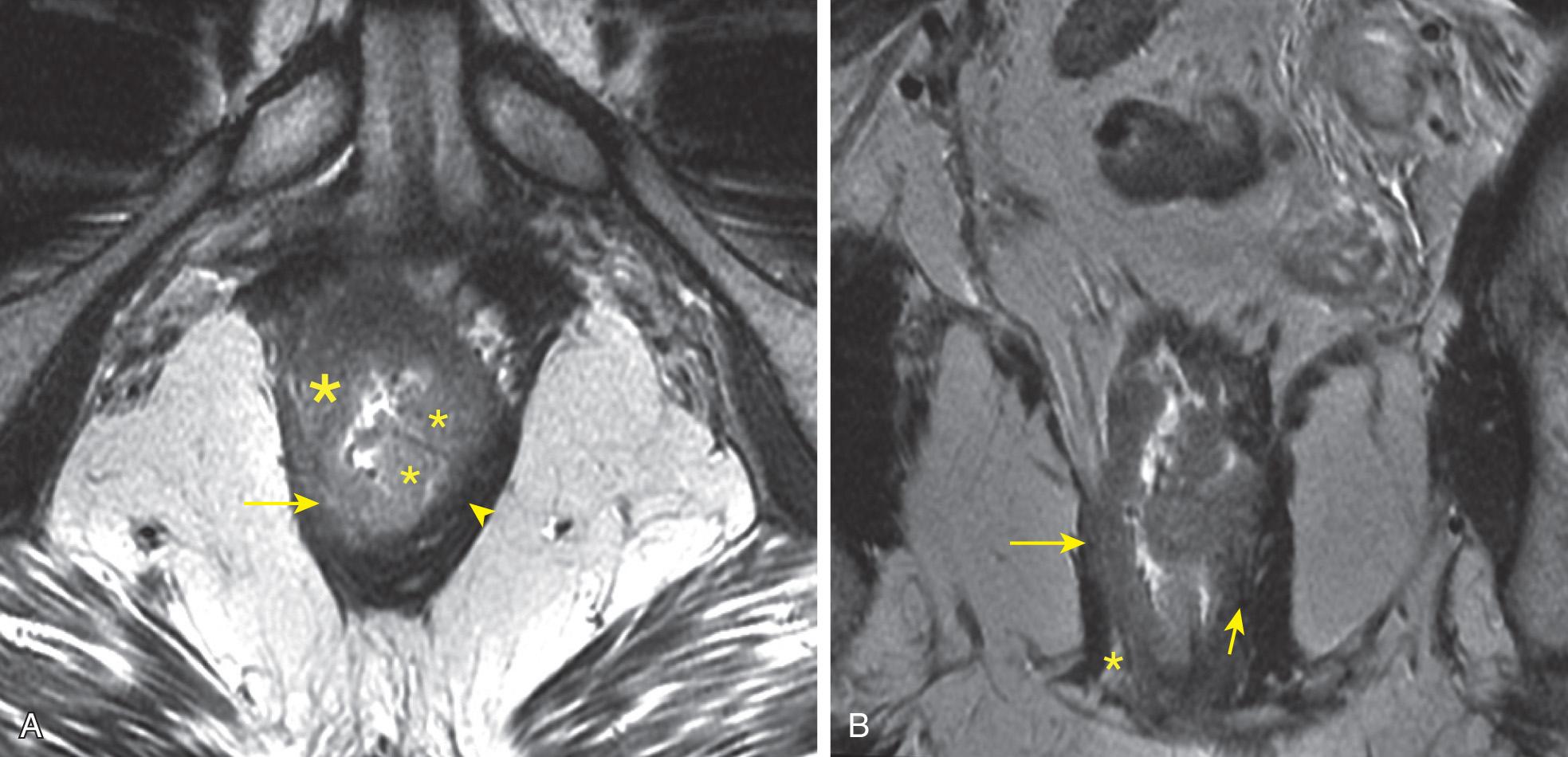
The initial use of endorectal coil MRI has been supplanted by the quality of present imaging techniques. The use of an endorectal coil is not recommended. Enema prep is not required. An indwelling rectal stent typically results in some degree of imaging artifact, but diagnostic information can often still be obtained ( Fig. 146.3 ). Ideally, the patient receives pre- and posttreatment examinations with the exact same parameters and protocol. In today's common practice, patients may not have a pretreatment MRI, or it may have been performed using a different technique prior to care being transferred to a high-volume center. Reproducibility of the technique will continue to improve with the move to centers of excellence and the standardization of care.
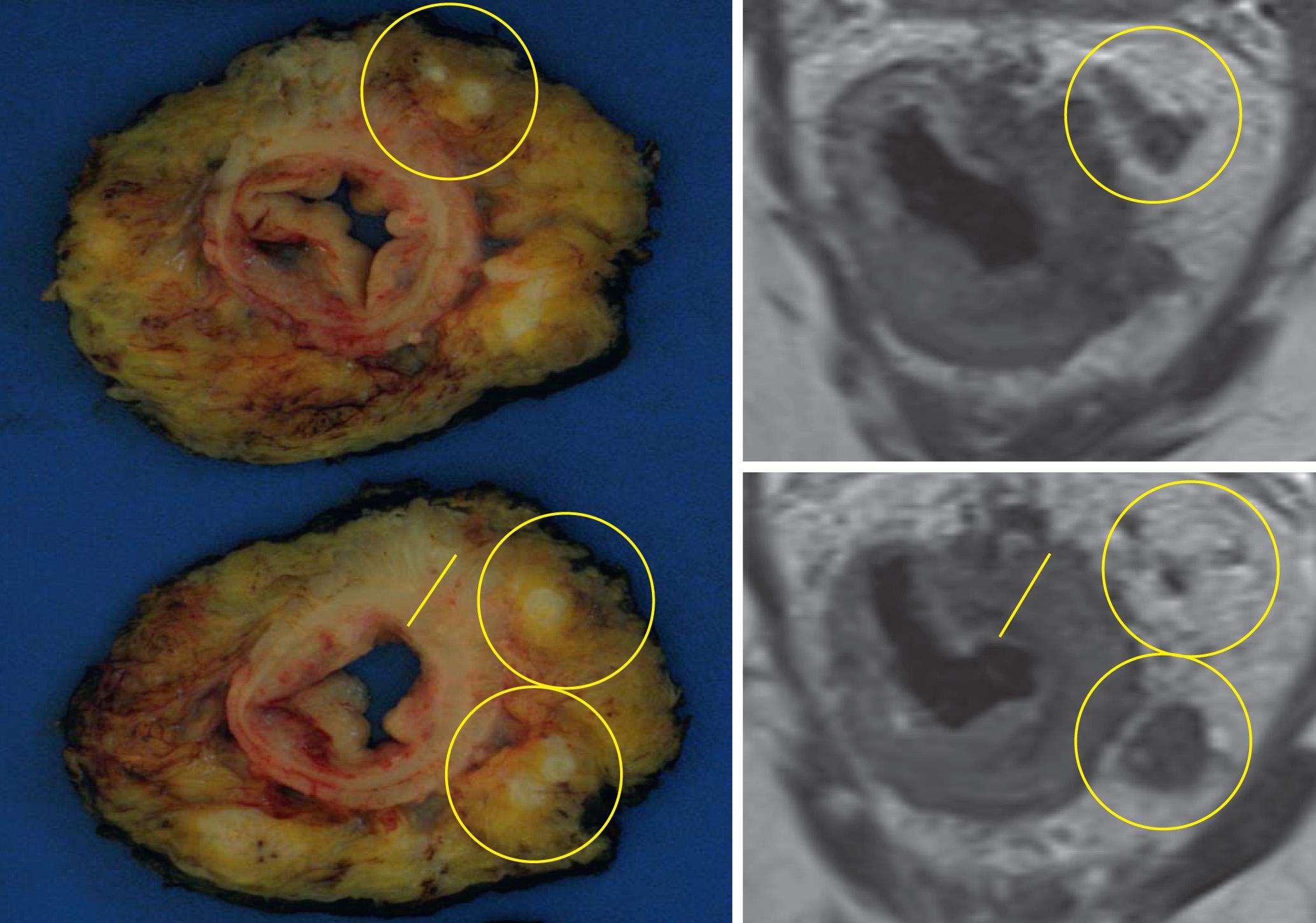
Although accurate disease characterization hinges on appropriate image acquisition, synoptic reporting of findings is necessary to ensure that all elements of pathology are captured in the report. Multiple synoptic reporting templates are publically available for both the staging and restaging of rectal cancer; the Cancer Care Ontario, Society of Abdominal Radiology, and Royal Marsden Hospital have all published similar templates, the common features of which are discussed later. Importantly, the incorporation of MRI findings into the MDT conference has enabled the surgeon, oncologist, pathologist, radiologist, and all members of the MDT to develop treatment strategies based on accurate local staging. Discussions surrounding the threatened or positive CRM, local tumor management, “watch and wait,” and recurrent disease and its management have been the main focus of these conferences and most of these discussions are based on MRI findings. Comparison of the preoperative MRI with the final pathology specimen provides an opportunity for quality assurance of surgery, pathology, and radiology ( Fig. 146.4 ). This precise radiologic-pathologic correlation requires the pathology specimen to be processed in a “breadloaf” technique as put forth by Quirk. If the rectum is “flayed open” along the organ's long axis, point-to-point MRI to pathology correlation is not feasible. Notably, rather than longitudinally opening a rectal specimen to assure an adequate distal margin, a pathologist should be summoned to gently partially evert the rectum and measure the margin.
Staging the patient with rectal cancer using tumor, node, metastasis (TNM) methodology put forth by the American Joint Committee on Cancer (AJCC) involves an assessment of the local tumor extent with regard to the bowel wall (T category), clinical lymph node status (N category), and the presence of metastatic disease (M category). The mucosa, submucosa, and muscularis propria can be distinguished on high-resolution MRI ( Fig. 146.5 ). MRI has been validated by multiple studies to accurately assess mural and direct extramural tumor spread and lymph node status. The MERCURY Trial confirmed MRI as the preferred modality of local evaluation. The following parameters are part of the standard reporting system for rectal cancer imaging.
The primary tumor is evaluated based on its morphology (semiannular [ Fig. 146.6 ], annular, polypoid [see Fig. 146.1 ]) and for the presence of mucinous features. The recognition of the tumor morphology is important because a common diagnostic pitfall leading to overstaging is confusing the raised, rolled tumor edge of a semiannular endoluminal tumor or the large endoluminal component of a polypoid tumor to be the invasive component of the tumor. Mucinous tumors are known to be a poor prognostic feature in rectal cancer. The presence of mucinous features can be reliably detected at MRI.
The height of the tumor from the anal verge and sphincteric complex and the radial location of the tumor are reported. Based on imaging, the tumor is in the upper third when its lowest margin is greater than 10 cm from the anal verge, and in the middle third when its lowest margin is 5 to 10 cm. The lower third is defined as less than 5 cm from the anal verge. Perhaps a more surgically relevant distinction of the low rectum is where the levator muscles converge medially, resulting in the sharp tapering of mesorectal fat, which can be observed on Fig. 146.2 . This distinction is critical as it is known that low rectal tumors are more challenging to stage and treat. Indeed, a separate staging schema has been proposed for low rectal cancer ( Table 146.1 ).
| Stage | Low Rectal Cancer as Seen on Magnetic Resonance Imaging |
|---|---|
| 1 | Confined to bowel wall but does not extend through full thickness; intact outer muscle coat |
| 2 | Replaces muscle coat but does not extend into intersphincteric plane |
| 3 | Invades intersphincteric plane or lies within 1 mm of levator muscle |
| 4 | Invades external anal sphincter and is within 1 mm and beyond levators with or without invading adjacent organs |
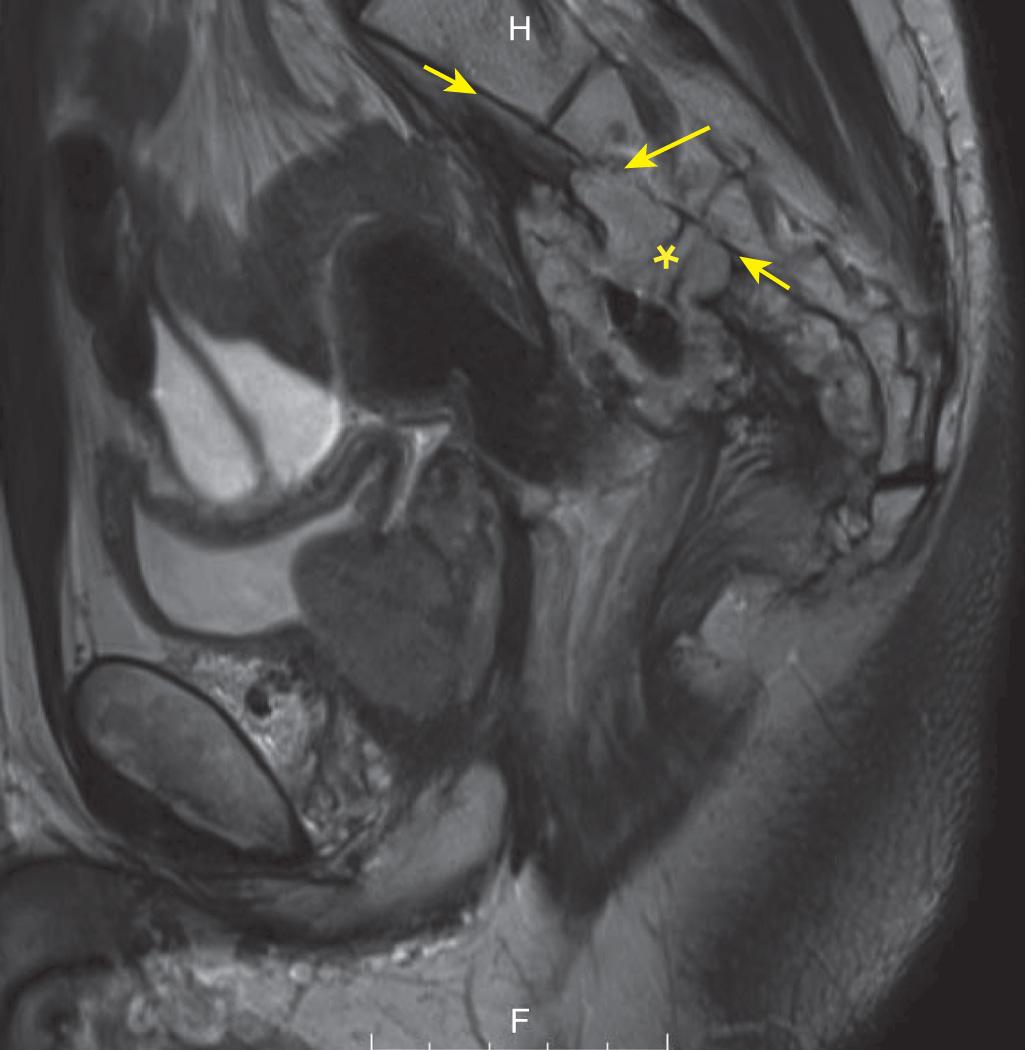
The T stage and depth of invasion (DOI) are assessed (see Fig. 146.4 ). MRI estimation of DOI is accurate to less than 0.5 mm of the final pathologic specimen, as demonstrated by the MERCURY experience. T2–T4 tumors need MRI for more accurate evaluation. Small tumors, less than 2 cm, may still benefit from more precise characterization with transrectal ultrasound (TRUS). The presence of a DOI greater than 5 mm beyond the bowel wall can be detected and can help identify the need for radiation treatment planning. The ability to accurately identify T4 lesions and their invasion into the vagina, uterus, prostate, seminal vesicles, and bladder has also been helpful in pretreatment care planning ( Figs. 146.7 and 146.8 ; see also Fig. 146.3 ). When measuring DOI, it is important to take into account the tumor morphology. For semiannular tumors, the DOI is measured at the midpoint of the tumor between the raised tumor edges, if present. For polypoid tumors, the DOI is measured at the tumor stalk (see Fig. 146.1 and Table 146.1 ).
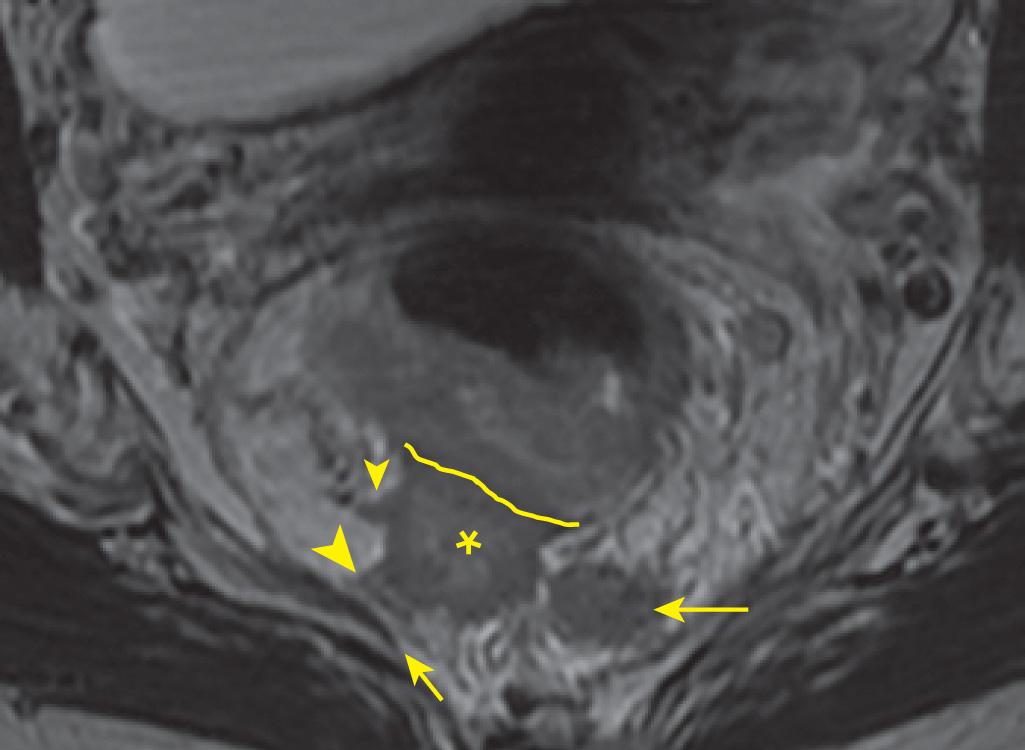
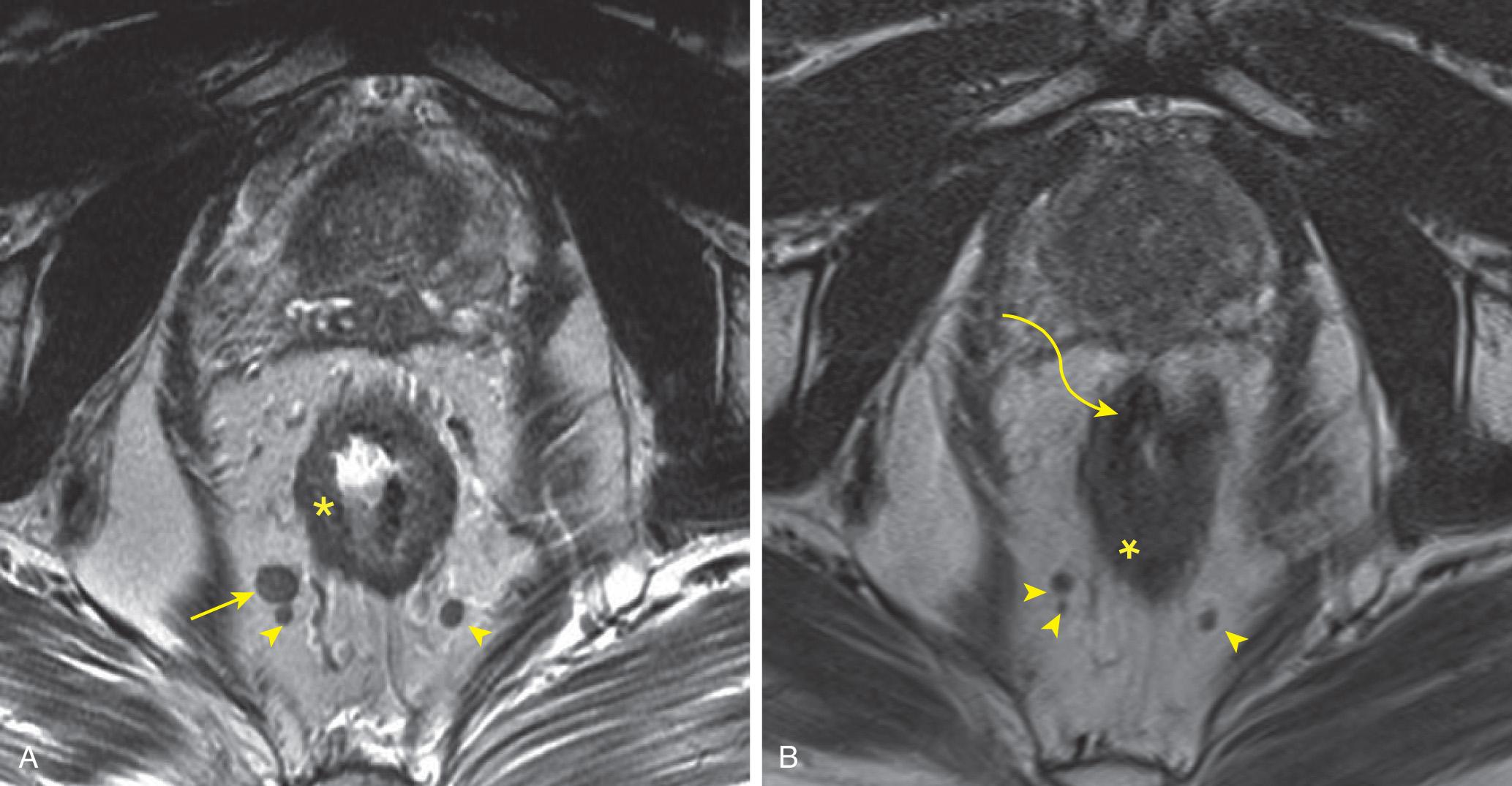
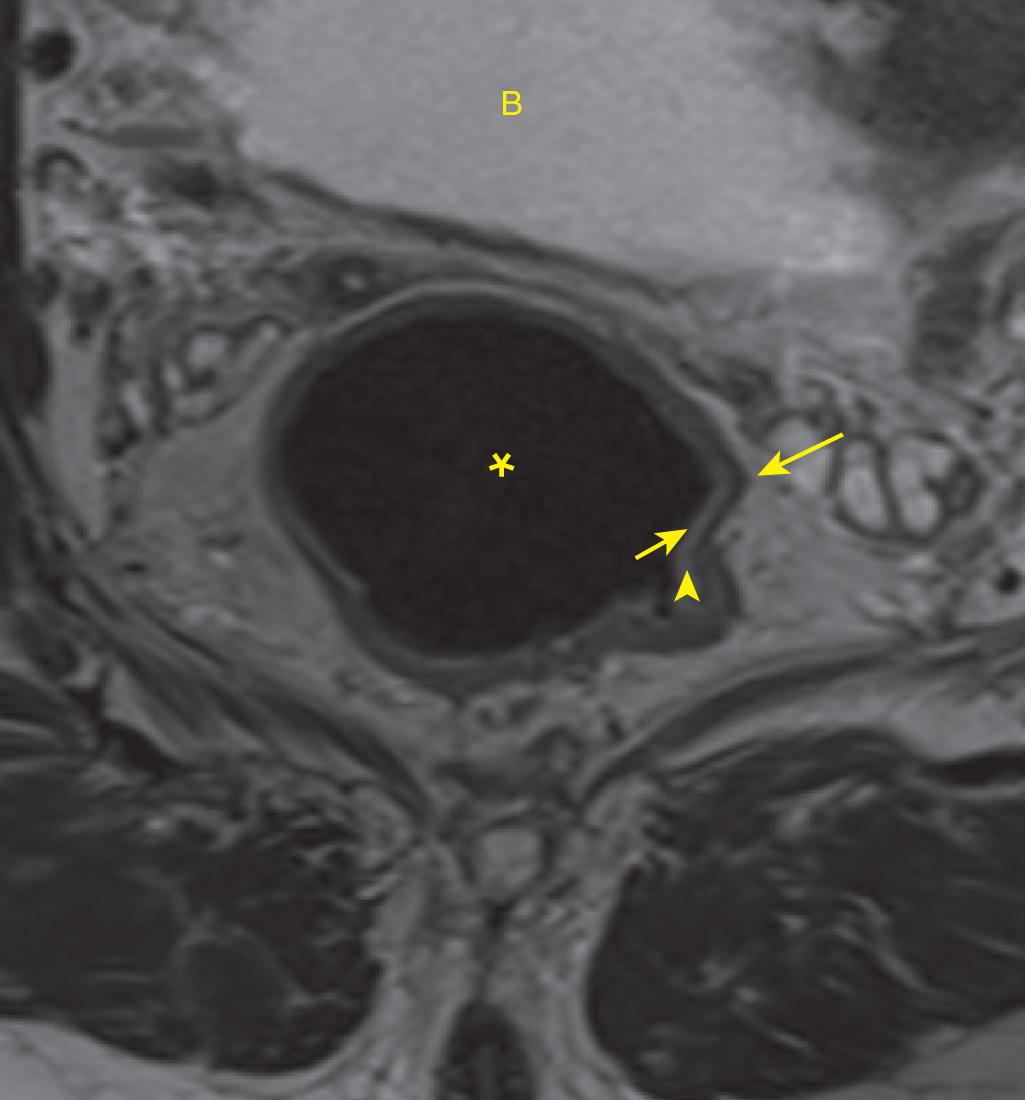
The extent of the tumor and its relationship to the mesorectal fascia as determined by MRI has been shown to correlate to the pathologic margin, allowing assessment of the CRM prior to surgery. The primary tumor, extramural vascular invasion, metastatic nodes, and tumor deposits may all involve the CRM. By MRI criteria, the CRM is taken to be positive if one of these entities is less than 1 mm from the mesorectal fascia, and the CRM is considered threatened when less than 2 mm ( Fig. 146.9 ). For low rectal tumors, violation of the intersphincteric plane is considered a positive CRM.
The peritoneal reflection is an important landmark for defining tumor location ( Fig. 146.10 ). It can be accurately identified in greater than 90% of cases. A tumor that is present below the peritoneal reflection is considered a low rectal tumor. Knowledge of the tumor location relative to the peritoneal reflection is necessary if considering TAMIS (transanal minimally invasive surgery) or TEMS (transanal endoscopic microsurgery) procedures (see Fig. 146.1 ).

The presence of EMVI is readily detectable on noncontrast MRI and is now a part of the standardized report for rectal cancer (see Fig. 146.9 ). EMVI is prevalent in 30% to 40% of patients with rectal cancer. Imaging findings of EMVI include irregularity or expansion of vessels, loss of normal vascular flow void, and intraluminal intermediate tumor signal intensity contiguous or separate from the main tumor. MRI is more sensitive at detecting EMVI than evaluating the pathologic specimen, as multiplanar assessment of the mesorectal fat and pelvic sidewall in their entirety is possible. Pathologic evaluation of EMVI is limited based on the slices taken and the single plane of analysis. Accurate assessment of EMVI requires pathologists to reference the MRI findings to direct their search. If EMVI is not initially confirmed on hematoxylin and eosin staining, elastin staining can be of benefit to confirm diagnosis. Some new data suggest that IV contrast administration may increase reader confidence with EMVI detection, but noncontrast imaging remains the standard. These findings underscore the importance of MRI in the evaluation of EMVI, given its prognostic indication of local recurrence and distant metastatic disease rather than nodal disease—the latter with a five-fold increased risk compared to patients without EMVI.
The accurate assessment of lymph node status is becoming more predictable. Although metastatic nodes are generally larger than benign counterparts, metastasis can be present in very small nodes. Nodes larger than 8 mm short axis are virtually all neoplastic, but using this size threshold alone is insensitive for detecting metastatic nodes. Short-axis size cutoffs for suspected malignancy are not as useful as nodal morphologic features in predicting malignancy. Irregular node border and mixed signal intensity are the most reliable predictors of nodal metastases. The precise relationship of perirectal nodes to the mesorectal fascia can be determined (see Figs. 146.9 and 146.10 ). MRI also identifies nodes outside of the mesorectum (see Fig. 146.7 ). Posttreatment MRI evaluation of lymph node status and pathologic correlation with the breadloafing of specimens allows node for node evaluation (see Figs. 146.4 and 146.11 ).
MRI reporting should identify the distal tumor edge and the encroachment of the tumor on the pelvic muscle floor (see Figs. 146.2 and 146.6 ). This also helps to distinguish candidates for sphincter-saving procedures from those requiring abdominal perineal resection (APR) for complete clearance of the tumor.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here