Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Head injury is a major source of disability and mortality worldwide. The CDC reports that in 2017 there were 224,000 head injury-related hospitalizations in the United States. Unintentional falls accounted for nearly 50% of these hospitalizations, motor vehicle crashes 25%, and strikes by an object, intentional self-harm, and assault accounted for the remaining 25% (CDC, Traumatic Brain Injury). Head injury may result in a variety of mild-to-severe neurologic deficits and can impair an individual's ability to communicate normally. Auditory dysfunction can frequently occur as a consequence of head injury and requires a thorough evaluation to localize the problem and permit appropriate rehabilitation.
Conductive hearing loss is a common type of auditory dysfunction that may occur following head injury. Often overlooked in the initial trauma assessment, head injury patients may present with conductive hearing loss in a delayed fashion. Conductive hearing loss may be transient from fluid or blood in the ear canal or middle ear. High-impact head trauma may result in temporal bone fractures that can damage the external auditory canal or middle ear structures and result in persistent conductive hearing loss. In the absence of temporal bone fractures, a small subset of head injury patients has also been shown to sustain conductive hearing loss. Close follow-up of patients with conductive hearing loss following head trauma is necessary to understand persistent external and middle ear issues and manage hearing loss appropriately.
The severity of head injury typically dictates the location of initial consultation and the resources available for patient evaluation. In cases of severe head trauma, patients may be either incapable or impaired in their ability to participate with clinical history, examination, and audiologic evaluation. The clinician must prioritize patient stabilization, and as such, otologic evaluation may be only rudimentary or may be necessarily delayed. Mild cases of head injury may be primarily evaluated in the otolaryngologists' clinic if the sole complaint is hearing loss. Evaluation of conductive hearing loss following head trauma typically includes a history, physical exam, and audiometry. In some cases, imaging of the temporal bones is also necessary.
If the patient is awake and alert, a complete auditory history and examination should be performed at the bedside or in the outpatient clinic. Important aspects of the history include the nature and timing of the head injury, whether the trauma was blunt or penetrating and any direct injury to the ear or temporal bone. Complaints of hearing loss, ear pain, otorrhea, tinnitus, imbalance, nausea, dizziness, vertigo, facial weakness, rhinorrhea, and other neurologic changes should be assessed. In patients with hearing loss, the time course and any transience or gradual improvement should be documented.
In settings of severe head trauma, the priority must be patient stabilization, including airway management, and assessment of breathing, hemorrhage, neurological status, and additional exposures. Patients with significant injury sustained during head trauma may have spinal precautions in place, and the spine should be evaluated and stabilized prior to manipulation of the head. When the patient is deemed hemodynamically stable, an otologic examination can occur. Performed by an otolaryngologist, the evaluation should include a focused head and neck exam including detailed otomicroscopic exam, bedside hearing evaluations, and subsequent referral for additional testing, when appropriate.
For patients with severe head trauma, the initial otologic exam may occur at the bedside in the emergency department or intensive care unit, and patients may have limited ability to participate. In settings of less severe head trauma, the otologic exam may occur in an otolaryngologists' clinic, with the patient typically able to participate more actively.
A full head and neck examination should be performed to assess for sequelae of head injury. After ensuring the patient is stable, a detailed otologic exam is completed. Examination begins with a thorough inspection of the external auricle looking for any signs of trauma, such as swelling, lacerations, erythema, and discharge from the external auditory canal. If otorrhea is present, the onset, quality, color, and volume should be documented ( Fig. 6.1 ). A cerebral spinal fluid (CSF) leak may mix with blood from the middle ear or ear canal; thus, a large persistent volume leak from the ear should raise suspicion for a CSF leak. A sample should be collected to check for the presence of beta-2 transferrin. Given the typical long time frame for test results to return, a “‘halo sign” may be assessed at the bedside. Here, a drop of fluid may be placed on tissue paper and examined for signs of a ring of clear fluid around a drop of blood, indicating the presence of CSF.

Every effort should be made to clear the external auditory canal to permit an examination of the tympanic membrane (TM). If the TM is intact, pneumatic otoscopy may be used to determine TM mobility. Immobility of TM on pneumatic otoscopy, air/fluid levels, and dullness of landmarks may suggest middle ear effusion or hemotympanum. Hemotympanum (and a conductive hearing loss) may be the only sign the patient has a temporal bone fracture and should prompt a high-resolution CT scan of the temporal bones ( Fig. 6.2 ). If there is a visible perforation in the TM, assessment of size, location and any epithelial debris within the middle ear should be noted. Relative location of the ossicular chain should also be documented.

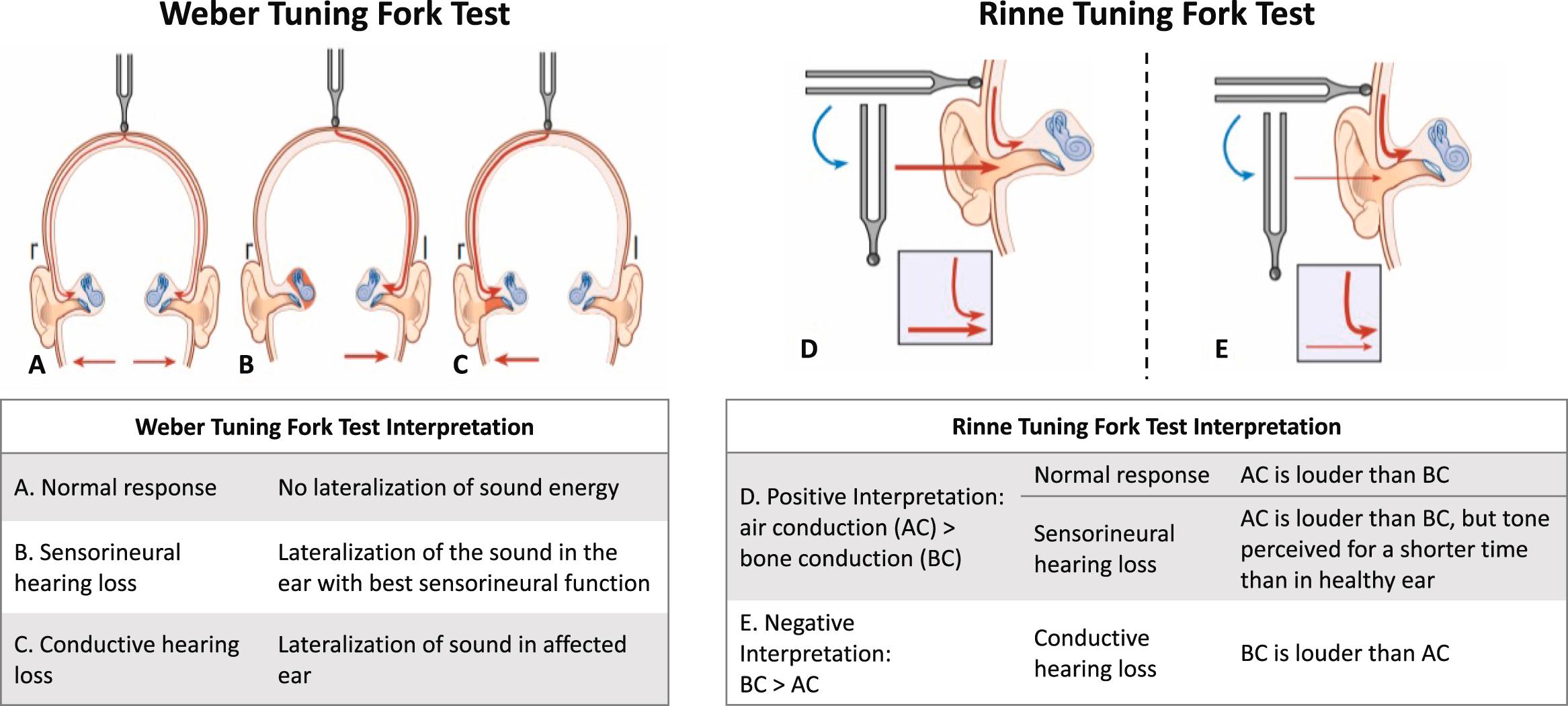
Hearing evaluation including tuning fork tests and bedside speech reception thresholds should be performed to determine the type and severity of hearing loss. The Weber and Rinne tests can be performed as an early assessment of hearing loss ( Fig. 6.3 ). Both tests can be performed at the bedside typically with a 512-Hz tuning fork. A Weber test is suggestive of conductive hearing loss if the fork is heard loudest in the affected ear. A negative Rinne test is suggestive of a conductive hearing loss of at least 30 dB at 512 Hz if bone conduction is heard louder than air conduction. Interpretation of full Weber and Rinne test results may be found in Fig. 6.3 . Whispered word tests can also screen for a drop in speech intelligibility, which may suggest a sensorineural hearing loss. While tuning fork and whispered word tests can be a first step in determining the nature of hearing loss, they alone are insufficient for diagnosis of hearing loss type and severity. Ideally, patients should be referred for behavioral pure tone audiometry.
Threshold audiogram —Alert, responsive patients should be tested via pure tone audiometry to further assess for conductive hearing loss. Ideally, testing is performed in a sound-treated booth, although bedside threshold and speech testing is also possible in some centers. Both air and bone conduction testing should be completed to determine the type of hearing loss. Because head trauma may result in conductive hearing loss from a variety of sources, the degree and frequency dependence of the air–bone gap (ABG) may differ based on hearing loss etiology. For example, a small TM perforation may result in a small ABG, while ossicular discontinuity with an intact TM may result in a maximal conductive hearing loss. In most cases, speech discrimination will not be affected by pure conductive pathology, and when speech is presented at an appropriate loudness for the patient's hearing loss, discrimination should be excellent. Fig. 6.4 outlines an example audiogram showing an air/bone gap from a 37-year-old patient with left-sided ossicular chain discontinuity following temporal bone fracture. Table 6.1 shows typical hearing loss severity and frequency dependence by the type of conductive lesion.

| Classification | Expected loss |
|---|---|
| Perforation of TM | 10–40 dB, worse at low frequency and proportional to size of perforation , |
| Perforation of TM with ossicular interruption | >35 dB, greater losses imply discontinuity |
| Intact TM with partial (fibrous) ossicular interruption | 30–40 dB, worse at high frequencies, primarily above 1 kHz (Farahmand et al. 2016) |
| Hemotympanum | 10–30 dB |
| Ossicular interruption with intact TM | 55–60 dB |
Tympanometry —Tympanometry may be performed to measure middle ear immittance, providing a quantitative measure of middle ear compliance that is more reliable than pneumatic otoscopy. The tympanometric waveform is typically obtained at 226 Hz and provides information about how sound energy enters the middle ear as a function of ear canal pressure. Head trauma may lead to conductive pathology that can be detected and differentiated via tympanometry. A normal, type A tympanogram indicates an intact TM and ossicular chain with middle ear pressure that is similar to ambient pressure ( Fig. 6.5A ). An ossicular discontinuity will result in a hypercompliant TM with a “sharp peak” as is seen in Fig. 6.5B . Middle ear fluid, such as hemotympanum, will result in a flat waveform with a normal ear canal volume, whereas a flat waveform with elevated ear canal volume is indicative of a TM perforation ( Fig. 6.5C and D ).

Otoacoustic emissions testing and auditory brainstem — Otoacoustic emissions (OAE) testing and auditory brainstem response (ABR) are objective audiometric tests that can be performed on patients who cannot undergo conventional audiometry, as neither test requires recording a patient's subjective response to sound. Otoacoustic emissions are low-amplitude sound waves produced by the cochlea, transmitted across the middle ear to the external ear where they can be recorded. A healthy cochlea produces OAEs, and both conductive and sensorineural hearing loss can affect OAEs. Auditory brainstem response testing consists of an electrical response to an auditory stimuli to assess the auditory pathway from the ear through the brainstem to the auditory cortex. ABR testing can distinguish between conductive and sensorineural hearing loss if bone conduction stimulation is used ; however, measurement of conductive losses with ABR is limited in frequency resolution, and severity and must be coupled with behavioral audiometry whenever possible.
Temporal bone imaging is frequently necessary in the evaluation of conductive hearing loss associated with head injury. Imaging allows for the evaluation of trauma to the temporal bone and soft tissues of the entire auditory pathway. Imaging can be performed with magnetic resonance imaging (MRI) or computed tomography (CT). Advantages to MRI include the avoidance of radiation exposure and sensitivity to soft tissue as well as central auditory abnormalities, while CT allows for precise spatial resolution of bony anatomy of the external, middle, and inner ear.
High-resolution computed tomography without contrast, including fine cuts in both the coronal and axial planes (0.6 mm), should be obtained in patients who are found to have obvious head, outer/middle ear trauma, peripheral nerve dysfunction, hemotympanum, periorbital or retroauricular hematoma, otorrhea or rhinorrhea containing CSF, or new-onset posttraumatic vestibular symptoms. Fractures of the temporal bone are associated with a high incidence of conductive hearing loss in the acute phase due to blood within the external auditory canal or middle ear (hemotympanum). Persistent conductive hearing loss after temporal bone fracture should be evaluated radiographically to look for ear canal collapse or ossicular chain disruption. The radiologist and practitioner must work closely together to assess for subtle findings associated with posttraumatic conductive hearing loss. If patients are found to have conductive hearing loss that does not improve after resolution of hemotympanum, repeat imaging may be indicated. See Fig. 6.6 for examples of ear trauma viewed on high-resolution CT.

Management of conductive hearing loss associated with head injury depends on the source of conductive pathology. If the source of conductive hearing loss is transient, for example, from hemotympanum or an ear canal laceration, simple observation, or treatment with ototopical drops, is sufficient. However, persistent conductive hearing loss may require management with amplification or surgery. While conductive hearing loss is frequently seen following temporal bone fracture, a fracture is not necessary for many conductive lesions in head injury as will be discussed in the following. It is also important to note that immediately following injury, more than one lesion affecting the conductive pathway is frequently present in the same patient. Repeat examination and audiometry after a duration of 6–8 weeks is important to ensure resolution or to identify persistent lesions that need further evaluation and management.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here