Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Conjunctivochalasis is a common bilateral condition characterized by redundant, loose, nonedematous conjunctiva.
Its incidence increases with age, and its pathophysiology remains unclear.
It is often asymptomatic; however, it can cause a range of symptoms from ocular irritation, lacrimation, pain, blurry vision, dryness, or redness. A more severe presentation—with subconjunctival hemorrhage and conjunctival protrusion with corneal exposure—is rare.
Conjunctivochalasis is an important differential diagnosis that must be considered in patients with ocular irritation and epiphora. As its symptoms are nonspecific and examination findings are sometimes subtle, the diagnosis is often missed.
Dry eye often coexists and must be treated to ascertain the significance of the conjunctivochalasis.
In symptomatic disease, removal of the redundant conjunctiva is indicated to alleviate symptoms.
Conjunctivochalasis (CCh) is usually a bilateral condition characterized by redundant, loose, nonedematous conjunctiva. It is often asymptomatic and considered a normal variant of aging; however, it can cause a range of clinical symptoms and is an important differential diagnosis that must be considered in patients with ocular irritation and tearing.
The term conjunctivochalasis , taken from the Greek word meaning “relaxation of conjunctiva,” was first coined by Hughes in 1942. However, descriptions of the same entity were reported as early as 1908 by Elschnig, and in 1921 and 1922 by Braunschweig and Wollenberg, respectively. Meller and Tseng divided the history of CCh into three periods. The first period (1908–1942) described severe CCh causing symptoms of pain, corneal ulceration, and subconjunctival hemorrhage due to exposure problems. The second period (1984–1989) focused on moderate CCh causing tear clearance problems. Liu proposed that the more common mechanism of tear flow interference by CCh was due to disruption of the tear meniscus rather than the occlusion of the inferior punctum by redundant conjunctiva. The third period (1990–1995) focused on the relationship between mild CCh and an unstable tear film. Höh introduced a grading system for CCh and found that the degree of CCh had a high predictive value for the diagnosis of keratoconjunctivitis sicca.
CCh typically presents as loose inferior bulbar conjunctiva that prolapses above the lid margin; however, it may also involve the medial, lateral, and superior conjunctiva. Symptoms include irritation, lacrimation, pain, blurry vision, dryness, redness, or subconjunctival hemorrhage. As the examination findings may be subtle, the diagnosis may be missed initially and the symptoms attributed to other common pathologies such as dry eye. As CCh often coexists with other pathologies, especially meibomian gland dysfunction (MGD), it is often necessary to treat and exclude other causes of ocular irritation before the significance of the CCh becomes apparent.
CCh is a common age-related eye disease. Although it can be seen in the first decade of life, its prevalence and severity increase with age. A large community-based study by Zhang in China found a prevalence rate of 44% in subjects older than 60 years of age. Mimura found a much higher prevalence rate of CCh in a hospital-based study in Japan, with 98% of patients older than 60 years having CCh. This study found that increasing age is the most important risk factor for CCh, although it was present even in the first two decades of life. They suggested that allergic conjunctivitis and pterygium may be risk factors for CCh in younger patients. Mimura’s study found an age-related increase in the grade of CCh. Gumus objectively evaluated the grade of CCh using Fourier-domain optical coherence tomography and found that the severity of CCh affecting the temporal and nasal conjunctiva was strongly correlated with age. Contact lens wear, axial length (shorter axial length), pinguecula, and thyroid disease have also been suggested as risk factors for the development of CCh.
CCh is a common cause of epiphora and should be distinguished from other common causes such as MGD, aqueous tear deficiency, dry eye, or nasolacrimal obstruction. In a study by Ishikawa looking at older adult Japanese patients whose main complaint was epiphora, CCh was found to be the main cause in 56 of 220 patients (25%) compared to 96 (44%) due to dry eye and only 30 (14%) with lacrimal obstruction.
The pathogenesis of CCh is unclear. Studies have been limited and at times conflicting. Early publications suggest that CCh is due to senile changes and mechanical forces such as eye movement, eyelid laxity, lid pressure, and eye rubbing. , Other studies have found the increased presence of inflammatory markers in CCh tissue, suggesting that inflammation plays an important role in the pathogenesis of CCh. It could be that there is a pathogenic cycle of conjunctival redundancy, friction, inflammation, and degradation of extracellular matrix.
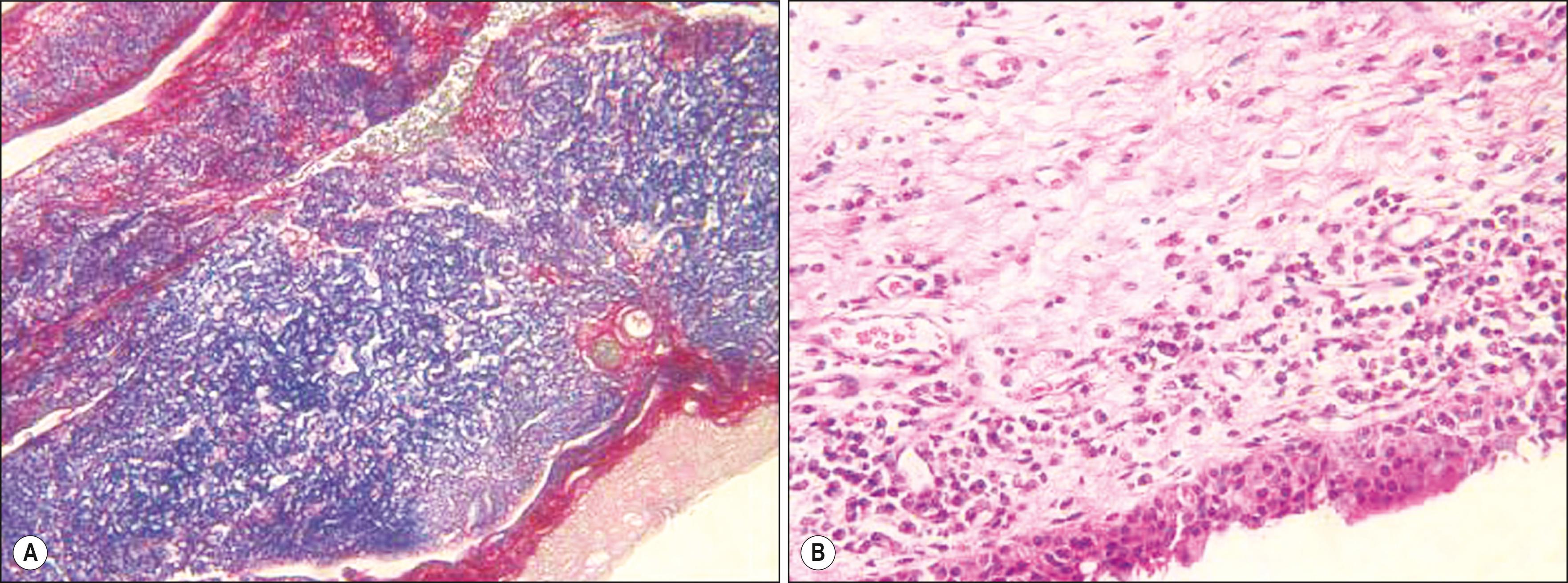
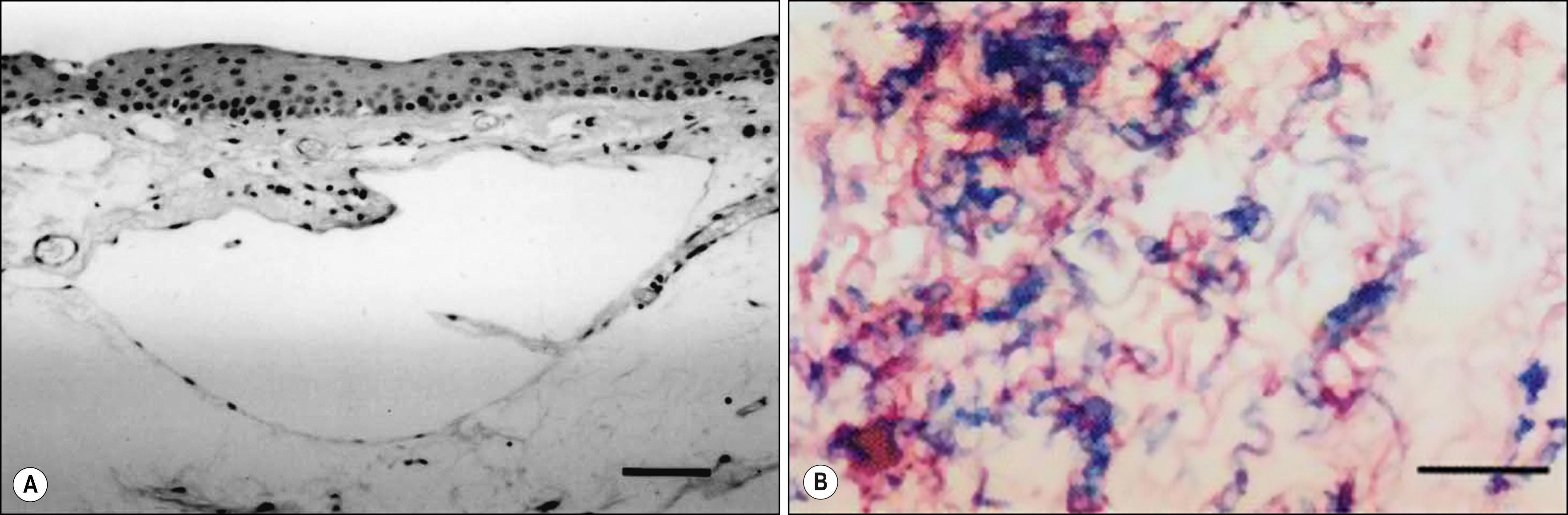
A histopathologic case-control study by Francis et al. found that the majority (22 of 29 specimens) with CCh had normal conjunctiva, whereas only four specimens showed chronic nongranulomatous conjunctivitis and three demonstrated features of elastosis ( Fig. 50.1 ). They concluded that the etiology of CCh is multifactorial and suggested that local trauma, ultraviolet radiation, and the immunologic effects of delayed tear clearance appear to be contributory. In contrast, Watanabe et al. found that 39 of 44 histopathologic specimens of CCh showed microscopic lymphangiectasia and all showed negligible inflammation. In addition, all specimens showed fragmented elastic fibers and sparsely assembled collagen fibers ( Fig. 50.2 ). They hypothesized that the mechanical forces between the lower eyelid and conjunctiva caused chronic, prolonged obstruction of lymphatic flow and lymphatic dilation, eventually giving rise to clinical CCh.
Several studies suggest that a shift in the normal balance of conjunctival metalloproteinases (MMPs) and tissue inhibitors (TIMPs) causes degradation of the extracellular matrix and results in the loose redundant tissue in CCh. Li et al. demonstrated overexpression of MMP-1 and MMP-3 by CCh fibroblasts compared with normal conjunctival fibroblasts, whereas levels of tissue inhibitors, namely TIMP-1 and TIMP-2, remain unchanged. This is supported by another study by Xiang et al. comparing 46 eyes with CCh to 27 control eyes that showed significantly higher expression of MMP-1 and MMP-3 levels in the CCh group compared with controls. TIMP-1 and TIMP-3 expression did not differ between groups. Inflammatory cytokines such as interleukin-1β (IL-1β) or tumor necrosis factor-α (TNF-α) may initiate increased expression of MMPs in CCh fibroblasts. IL-6 and IL-8 have been found to be significantly higher in tear samples of patients with CCh, and higher levels were also positively correlated with severity of grade of CCh. Ward et al. also found increased levels of proinflammatory cytokines TNF-α, IL-1β, IL-6, IL-8, and IL-12 in tears of patients with CCh. Immunohistochemistry staining demonstrated increased numbers of conjunctival epithelial cells and stromal fibroblasts that stained positively for MMP-3 and MMP-9. In addition, they demonstrated that conjunctival tissue samples from CCh patients showed the presence of oxidative stress, as evidenced by a significantly higher number of cells positively stained for a marker of lipid oxidative damage and a marker of DNA oxidative damage.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here