Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A bedside nurse initiated a rapid response code for a patient who appeared to be in acute respiratory distress and was hypoxic. On arrival of the condition team, the patient was short of breath, sitting on the side of his bed. Per the bedside report, the patient was a 60-year-old male with a history of end-stage renal disease admitted earlier in the day for a two- to three-day history of dyspnea on exertion because of multiple missed dialysis sessions. Since calling the rapid response code, the patient’s dyspnea had worsened acutely, and his shortness of breath was unrelieved by albuterol nebulizations.
Temperature: 98.6 °F, axillary
Blood Pressure: 240/140 mm of Hg
Respiratory Rate: 32 breaths per min
Heart Rate: 120 beats per min
Oxygen Saturation: 82% on room air; 97% on 8L/min (LPM) nasal cannula.
A quick exam showed a middle-aged male in severe respiratory distress, tachypneic, and using accessory muscles of respiration. Significant crackles were present in all lung fields on auscultation, with trace edema present in the lower extremities. His cardiac exam showed tachycardia with no new murmurs. Trace bilateral lower extremity edema was present.
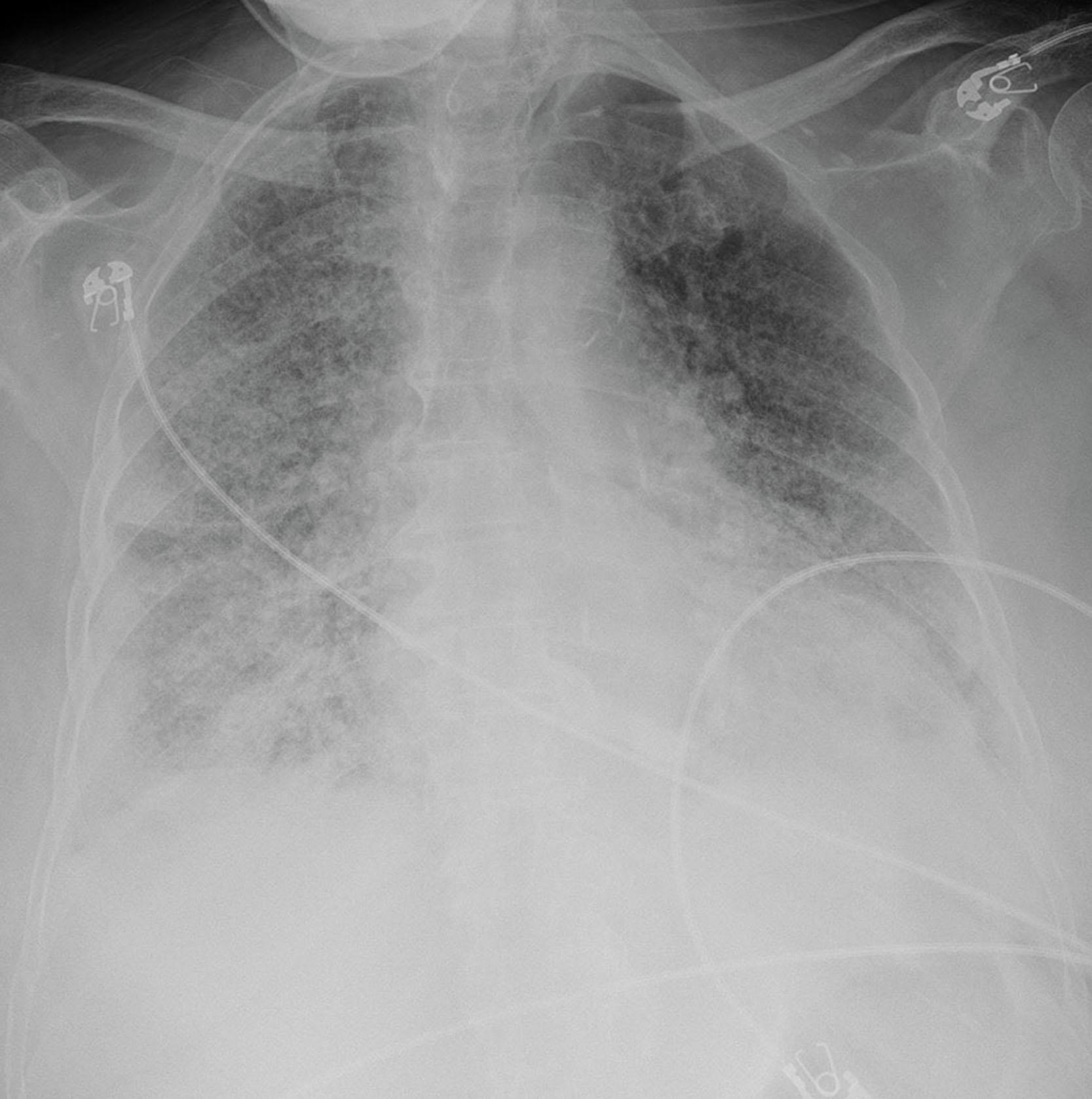
A cardiac monitor and associated pads were attached to the patient. Stat troponin, arterial blood gas (ABG), and chest X-ray were obtained. Possible causes of presentation were considered, including flash pulmonary edema in the setting of hypertensive crisis, acute exacerbation of congestive heart failure, acute coronary syndrome, or pulmonary embolism. ABG showed a pH of 7.55, paO2 of 70, paCO2 of 25, and oxygen saturation of 94% on 8 LPM. The chest X-ray was significant for bilateral pulmonary vascular congestion ( Fig. 25.1 ), and telemetry showed sinus tachycardia. A point-of-care ultrasound (POCUS) exam done by an in-house intensivist showed Kirley B-Lines in bilateral lung fields. Based on the available information, the most likely differential diagnosis was flash pulmonary edema in the setting of uncontrolled hypertension. The patient was started on non-invasive positive pressure ventilation via continuous positive airway pressure and transferred to the intensive care unit for monitoring and emergent dialysis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here