Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The fetal lungs are well-visualized either in the axial planes at the level of the four-chamber view ( Figure 15-1A ), the three-vessel view ( Figure 15-1B ), the upper abdomen transition to the chest ( Figure 15-2A ) or in a parasagittal plane ( Figure 15-2B ). In a right parasagittal view the lung length can be best appreciated showing the typical convex-shaped upper border and the concave-shaped lower border being the hypoechoic line of the diaphragm ( Figure 15-2B ).


The fetal lungs are generally subjectively assessed on ultrasound unless a suspicious finding is found. By virtually drawing a line from the spine to the anterior chest wall and dividing the chest into equal halves, the cardiac axis lies at a 45-degree angle to the left of the midline ( Figure 15-1A ). The right lung is larger than the left, since it has three lobes and the left lung two lobes, and by drawing this axis ![]() of the heart lies in the left hemithorax and
of the heart lies in the left hemithorax and ![]() on the right ( Figure 15-1A ). Heart size and lung size relationship is best assessed by subjectively estimating or directly measuring the ratio of cardiac circumference or cardiac area to the chest circumference or area obtained at the level of the four-chamber view. The cardiothoracic (C/T) circumference is nearly constant throughout gestation, with a mean value between 0.45 and 0.50. The echogenicity of the lungs is subjectively analyzed by comparing both lung lobes with each other and with liver echogenicity ( Figure 15-2B ), the lungs appearing slightly homogenously echogenic during the mid-trimester, with a reduction in echogenicity during gestation.
on the right ( Figure 15-1A ). Heart size and lung size relationship is best assessed by subjectively estimating or directly measuring the ratio of cardiac circumference or cardiac area to the chest circumference or area obtained at the level of the four-chamber view. The cardiothoracic (C/T) circumference is nearly constant throughout gestation, with a mean value between 0.45 and 0.50. The echogenicity of the lungs is subjectively analyzed by comparing both lung lobes with each other and with liver echogenicity ( Figure 15-2B ), the lungs appearing slightly homogenously echogenic during the mid-trimester, with a reduction in echogenicity during gestation.
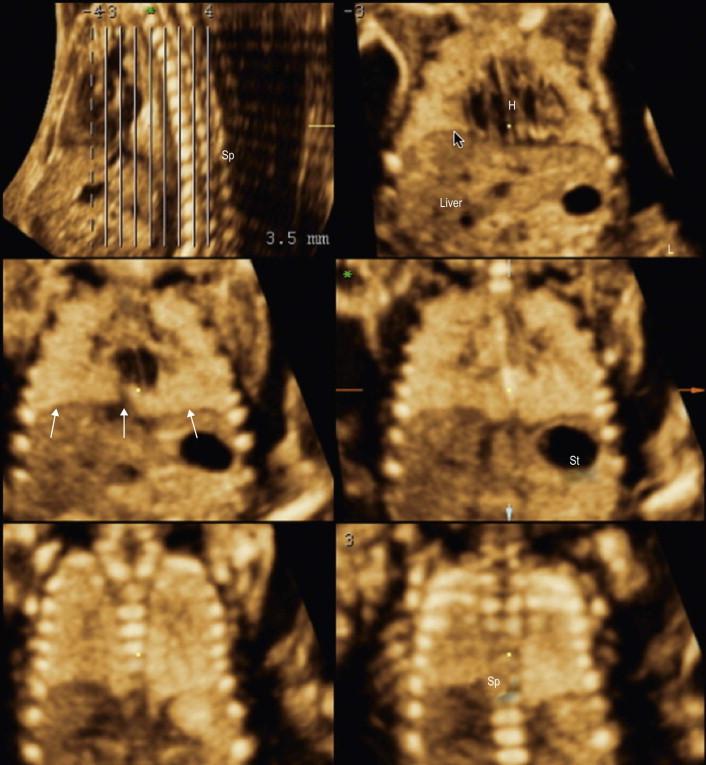
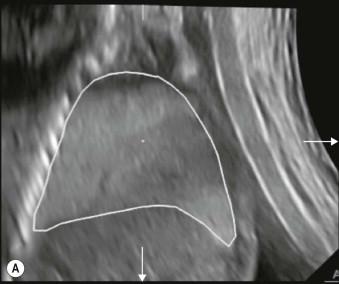
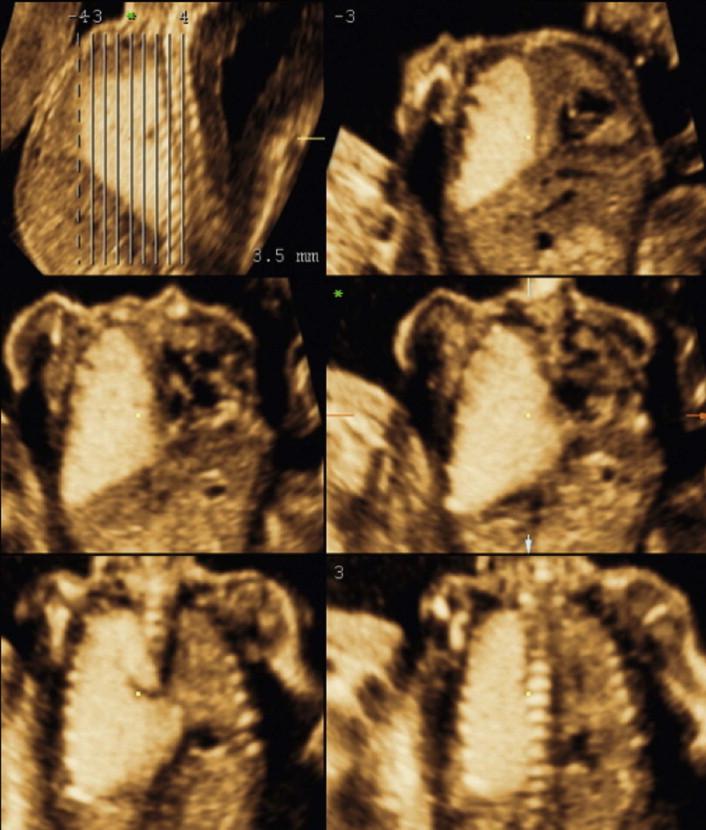
Using three-dimensional ultrasound the shape of the lungs and the relationship to other neighbouring organs can be best examined with the tomography display either in axial planes ( Figure 15-3 ) or in reconstructed coronal views ( Figure 15-4 ) demonstrating the clear border to the diaphragm and the normal conal shape of the thoracic cavity. In very specific conditions a volume measurement of the lung can be performed, but this technique needs specific expertise ( Figure 15-5 A and B ).

Anomalies affecting the fetal lungs are often suspected according to indirect patterns such as:
an abnormal collection of fluid within or around the lung;
an increased echogenicity of a part of the lung;
a mediastinal shifting of the heart.
In addition, extracardiac signs that can be associated with pulmonary anomalies are:
changes in amniotic fluid;
suspicious fetal malformations;
hydrops.
Lung anomalies are often an isolated finding with a low recurrence risk for subsequent pregnancies, apart from a few conditions with lung hypoplasia or when the finding is part of a syndrome as listed in Table 15-1 .
| Syndrome | Pulmonary Abnormality | Characteristic Features | Inheritance/Risk of Recurrence |
|---|---|---|---|
| Fraser syndrome | Tracheal/bronchial atresia (CHAOS) | Cryptophthalmos Microphthalmia Syndactyly Urogenital malformations |
Autosomal recessive 25% recurrence risk |
| Scimitar syndrome | Right lung hypoplasia with dextroposition of the heart | Partial anomalous pulmonary venous drainage of the right pulmonary vein(s) into the inferior vena cava Right pulmonary artery hypoplasia Aortopulmonary collateral artery |
No recurrence risk |
| Pallister–Killian syndrome | Diaphragmatic hernia | Facial dysmorphism Short limbs CHD Tetrasomy 12p detectable on amniocentesis and CVS but not in fetal blood |
Sporadic occurrence Low recurrence risk |
| Fryns syndrome | Diaphragmatic hernia | Facial dysmorphism Short limbs CNS anomalies |
Autosomal recessive 25% recurrence risk |
In this chapter we will focus on selected fetal pulmonary abnormalities as observed during second- and third-trimester ultrasound.
Congenital cystic adenomatoid malformation of the lung (CCAM) is characterized by cystic tissue replacing one part of the lung. The dysplastic bronchopulmonary tissue consists of numerous bronchiolus-like structures of variable size. The finding is usually unilateral and often restricted to one lobe (90% of cases), but can also affect an entire lung or very rarely be bilateral. CCAM of the lungs was proposed to be classified into macrocystic (Type 1), mixed (Type 2) and microcystic (Type 3) forms. Almost all lesions are isolated to the lungs and the combination with extrapulmonary malformations or chromosomal anomalies is rare.
The detection of a CCAM is straightforward once one or several cysts are visualized in the thoracic cavity ( Figure 15-6 A and B ), often associated with a deviation of the mediastinum ( Figure 15-7 and Figure 15-8 ).
Multiple cysts of different size (2 mm to 2–4 cm) within echogenic lung tissue ( Figure 15-9 ).
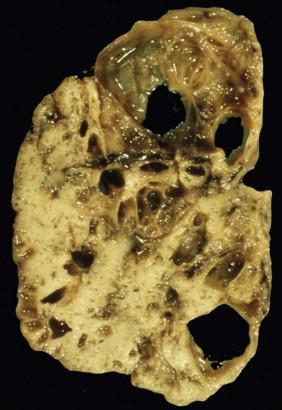
The whole affected lung is often enlarged ( Figure 15-8 ).



The heart can be slightly shifted to the contralateral side but when the affected lung is large a compression of the unaffected lung can occur increasing the risk of lung hypoplasia ( Figure 15-8 ).
CCAM is diagnosed after 15 weeks of gestation and rarely fetal hydrops is present at presentation. Three-dimensional ultrasound can provide, with its tomographical view, a general figure of the lesion extent. Volume calculation of the cysts, the affected lung or the remaining lung can complete the information provided by 2D ultrasound.
The differential diagnosis of CCAM depends on the main ultrasound finding.
In cases with an isolated large cyst, a diaphragmatic hernia or a brochogenic cyst are the main differential diagnoses.
In cases with a hyperechogenic lung lesion, the differential lies between a bronchopulmonary sequestration or a transient bronchial obstruction due to a mucous plug. Colour Doppler enables a bronchopulmonary sequestration and a CCAM to be differentiated from each other. An echogenic lung lesion without the presence of anechoic cysts and without an abnormal feeding vessel, could be simply a mucous plug and is not necessarily a microcystic CCAM (see section on Mucous Plug , later in chapter).
An intrathoracic teratoma will present as a heterogeneous cystic lung lesion of irregular outline, the overall size of which will increase throughout gestation (in a macrocystic CCAM it is the cystic element only that may increase in size throughout gestation). Fetal MRI can provide additional information on size and location and may help in the differential diagnosis.
The outcome of antenatally diagnosed CCAM is much better than previously reported with an overall survival rate into infancy of 90%. Outcome depends mainly upon:
the size of the completely affected lung region;
the severity of compression of the contralateral lung;
the presence of hydrops at detection.
The development of hydrops is not an inevitable feature. When hydrops is not present at diagnosis there is only a small chance (<10%) that it will develop.
Fetal interventions such as puncture of cyst or cystic-amniotic shunting are occasionally performed but mainly in cases with fetal hydrops. Postnatal surgery is performed to remove the affected lung and avoid recurrent infections and potential malignant change. Isolated microcystic lesions may resolve in utero, but some of these may have been due to a mucous plug (see also section on Mucous Plug , below). Postnatal evaluation with chest X-ray and spiral CT scan can help to evaluate apparently resolved lesions.
Bronchopulmonary sequestration (BPS) is characterized by a segment of non-functioning bronchopulmonary tissue lacking communication with the tracheobronchial tree. The typical finding of a BPS is the arterial blood supply provided directly by the systemic circulation at the level of descending aorta. Venous return is often to the systemic circulation but can occasionally be to the left atrium. Histologically these lesions are of two types but in the fetus the extralobar sequestration is the most common subgroup which is separated from the remaining lung parenchyma by its own pleural covering. The most common location is the basal region of the left hemithorax ( Figures 15-10 A and B, 15-11 A and B ), but 10% of cases can be present in the upper abdomen below the diaphragm: an infradiaphragmatic extralobar bronchopulmonary sequestration. Most BPS cases are isolated findings but can also be combined with a macrocystic CCAM or very rarely with a diaphragmatic hernia. The size of a BPS is small to moderate and it rarely fills the entire chest but the relative size tends to be reduced in the growing fetus ( Figure 15-12 A and B ).



The detection of a BPS is almost always achieved around 18–25 weeks’ gestation by visualizing a uniformly hyperechogenic lesion in a longitudinal or axial view of the fetal thorax, often resulting in a moderate mediastinal shift with heart displacement to the contralateral side ( Figure 15-10 ). The finding is often left basal and the hyperechogenic BPS can be well-discriminated from the normal echogenicity of the upper and contralateral lung lobe(s) ( Figure 15-10 ). A small number of fetuses may present with a pleural effusion or extremely rarely with non-immune hydrops. Colour Doppler is mandatory to achieve diagnosis by demonstrating the typical feeding artery from the thoracic ( Figure 15-11 ) or abdominal aorta, the latter crossing the diaphragm. Pulsed Doppler pattern shows a spectrum similar to the main pulmonary artery with antegrade flow in both systole and diastole ( Figure 15-11B ). Occasionally the feeding vessel is recognized on gray-scale ultrasound when high resolution probes are used. The hyperechogenicity of the lesion and the degree of mediastinal shift regress during the course of the pregnancy ( Figure 15-12 ) and in these cases the diagnosis can only be confirmed by colour Doppler in the third trimester. Three-dimensional ultrasound demonstrates in an overview, the extent of the lesion in comparison to the remaining lung by using a tomographical view, best in an anterior-posterior projection ( Figure 15-13 ). 3D glass-body mode feature can display the vascular supply ( Figure 15-14 ) and volume calculation can provide the volume of the lesion and if needed of the remaining lung tissue.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here