Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The relevance of lesions derived from the glandular portions of the endocervical canal has increased in recent years. There has been a reported increase in the incidence of preneoplastic and neoplastic endocervical lesions, both absolute and relative, when compared with the more common squamous lesions. In a study of US Surveillance, Epidemiology, and End Results (SEER) databases, incidence rates of squamous and adenocarcinomas of the cervix compared with a variety of demographic factors, such as age and race, were studied. Overall, cervical cancer incidence rates decreased by 54% from 13 to 6/100 000, with reductions in white and black populations of 51% and 70%, respectively. For squamous carcinoma, the overall decline was 61%. For adenocarcinoma, the incidence rate increased from 1.1 to 1.4/100 000, or by 32%. This increase was noted in white populations only, with black women showing an overall decline. Adenocarcinoma in situ (AIS) increased in both populations by about seven-fold. This increase in incidence of endocervical glandular lesions reported in the SEER databases is undoubtedly real, as numerous additional reports from many countries have found similar results on review of their own databases. However, this phenomenon is not universal with a small number of countries showing actual recent declines in adenocarcinoma rates (Finland, France, Italy) and others showing no change. Interestingly, the most recent data suggest that levels are universally plateauing or even declining in the later years of data. Any increase in incidence of endocervical glandular lesions is undoubtedly multifactorial. Rising incidence of preinvasive AIS may be linked, in part, as in squamous lesions, to better recognition of precursor lesions via improved sampling, better preparation techniques, changes in nomenclature, evolving methods of treatment, and advancing understanding of the morphologic features, and hence criteria for diagnosis, of early dysplastic lesions. In addition, changing patterns of hormone use in the modern population may also account for increases in glandular neoplasia. This phenomenon has been noted as a “birth cohort” effect. Recent declines have been postulated to be primarily due to better screening technology and improved recognition of the features of glandular neoplasia. Possible biologic mechanisms for the link between hormone use and the rise of glandular carcinomas will be detailed later.
This chapter will detail the histology of the normal endocervical canal, followed by the epidemiology and pathogenesis of endocervical glandular neoplastic lesions. Well-established morphologic criteria for cytologic diagnosis will be discussed.
One of the byproducts of improved sampling of the upper portions of the endocervical canal has been the emergence of new patterns of cytologic appearance of benign and reactive cells that may be present in these areas. This leads to a discussion of glandular “atypias,” which are described in The Bethesda System nomenclature as “atypical glandular cells,” with several subcategorizations. These cellular presentations can lead to significant confusion with regard to not only interpretation, but also to clinical management algorithms. The approach to differential diagnostic possibilities and the morphologic features that may help in their discrimination will be presented.
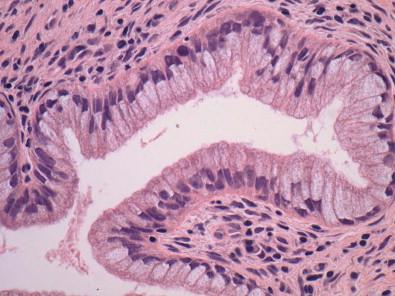
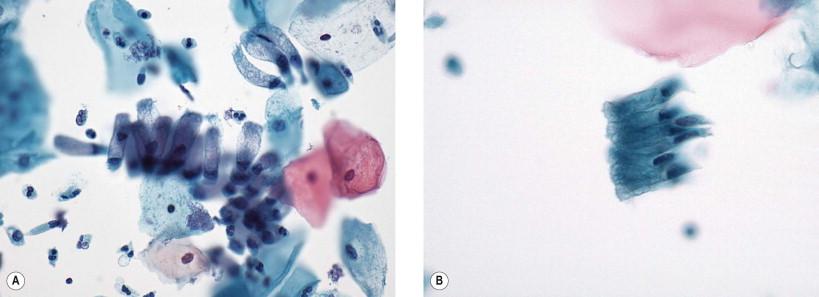
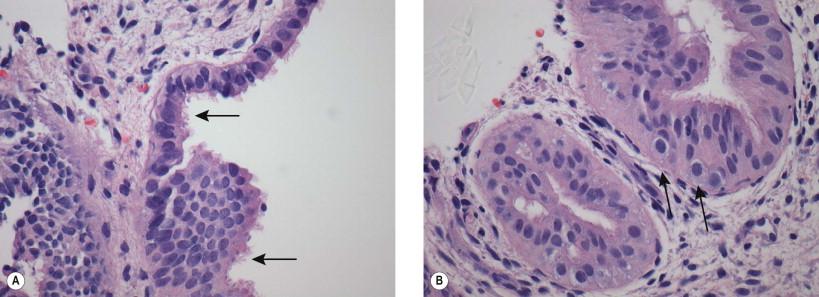
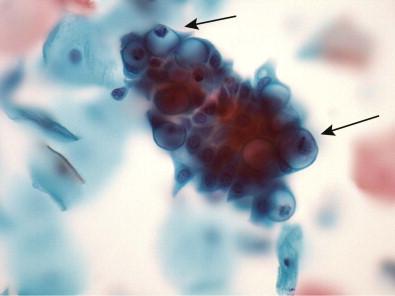
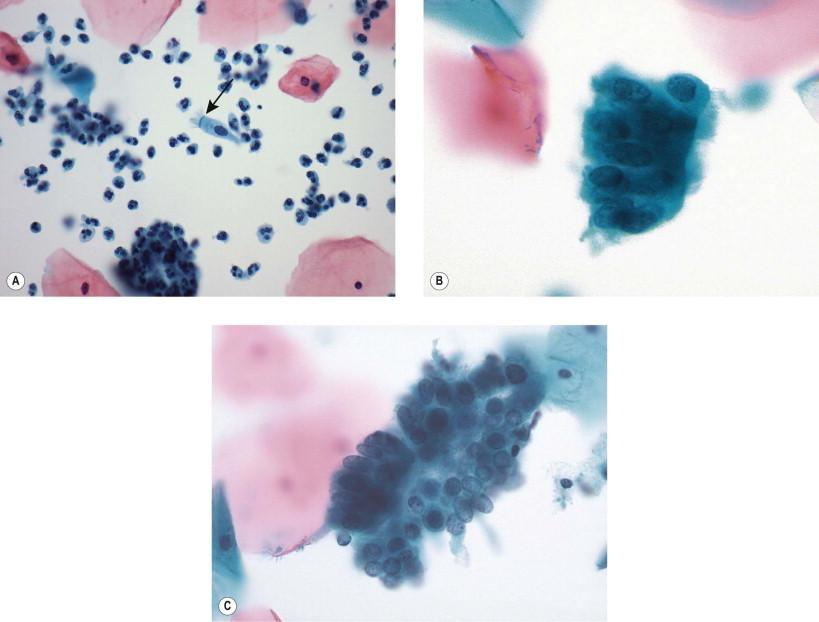
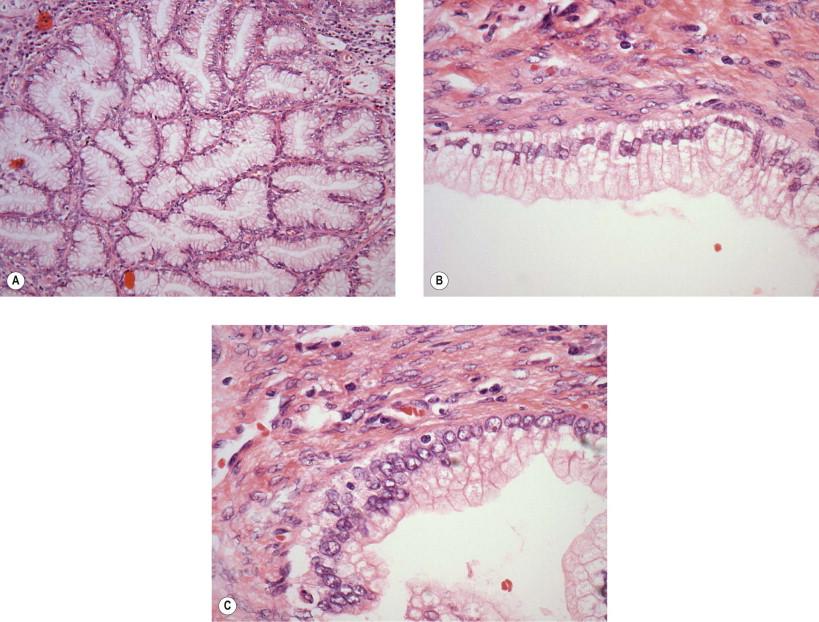
In order to recognize the cytologic appearance of endocervical glandular neoplasia with maximal sensitivity and specificity, a solid understanding of the normal and variant normal morphology of the epithelial surface of the canal is necessary. The normal endocervical canal has multiple histologic patterns depending on the proximal to distal location within the canal, and the age and hormonal status of the individual. Near to the area of the squamocolumnar junction, the endocervical mucosa shows the classically described pattern of tall columnar cells, with basally placed nuclei, and cytoplasm which contains clear or pale mucin contents ( Fig. 9-1 ). This translates into cytologic preparations having similar features of tall columnar cells arranged in a “picket-fence” appearance when viewed from the side ( Fig. 9-2 ), and the “honeycombed” appearance when viewed end-on ( Fig. 9-3 ). However, along its entire length, the histology of the endocervical canal will gradually change into the classic histology of the lower uterine segment. Therefore, along this gradient, the epithelium will change into a pattern more closely resembling endometrium. Cell and nuclear sizes gradually become smaller, the nuclei become more pseudostratified, and the cytoplasmic content becomes darker as mucin production fades. In addition, endocervical glands increase in number in the midportions of the canal and thus sampling from this area will produce more endocervical cellularity and greater numbers of endocervical groupings. A histologic example of endocervical/lower uterine segment epithelium shows an example of the striking nuclear pseudostratification that may be present in this area ( Fig. 9-4 ), with its concurrent cytologic appearance ( Figs 9-5 , 9-6 ). In women in the later childbearing age group and older (beginning in the mid- to late 30s), the endocervical canal can show yet further changes from these classic patterns, with increasing involvement by tubal metaplasia, as is also noted in this time period commonly involving the endometrium. Tubal metaplasia is the changing of the normal endocervical appearance to that mimicking the normal epithelium of the uterine tube. This pattern consists of three comingled cell types: ciliated columnar cells, goblet type mucin-producing cells, and slender intercalated cells. On cytologic examination, all three cell types can be seen. Tubal metaplasia may present as hyperchromatic crowded groups of cells ( Fig. 9-7 ), often with pseudostratification ( Fig. 9-8 ), and this pattern can lead to concerns about atypia and even neoplastic processes. These features and their importance in differential diagnosis with neoplastic entities will be further covered in “Atypical glandular cells,” below.
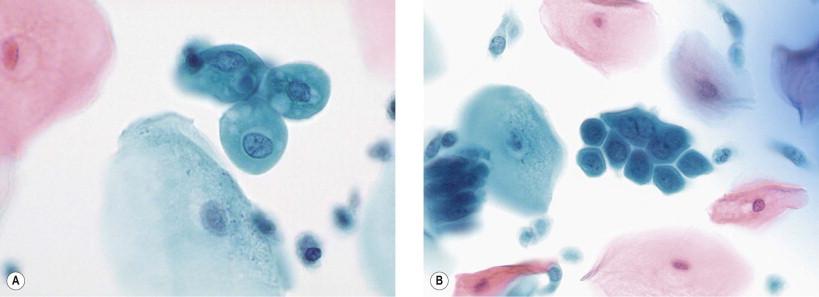
Another appearance of benign endocervical cells that must be considered is that of spontaneously exfoliated endocervical cells. These are individual cells that detach from the epithelial surface and travel in the mucus of the endocervical canal before being “picked up” by the sampling device. The “fluid” medium of the mucus causes the columnar cells to round up, giving them a configuration akin to squamous metaplastic cells. Close attention to cellular features such as frothy granular cytoplasm, perinuclear vacuoles, and fine granularity of nuclear chromatin with distinctive small nucleoli will help in the distinction from cells of squamous metaplasia, or, more importantly, from cells of squamous metaplastic “atypia” ( Fig. 9-9 ).
Squamous and glandular neoplastic lesions of the cervix are thought to be derived from a common progenitor cell, that being the undifferentiated reserve cells that may normally mature along both lines. When measured by sensitive detection methods, adenocarcinomas of endocervical origin and their precursors are virtually always associated with high-risk human papillomavirus (HPV) types (94% and 100%, respectively). The finding of a small percentage of HPV-negative invasive adenocarcinomas points to a low-incidence alternate pathway, most likely akin to endometrial or gastrointestinal neoplasia. HPV infection of these primitive cells is thought to be the primary and necessary event leading along the lengthy pathway that culminates, in a very small number of cases, as invasive carcinomas. The overall oncogenic sequence and the underlying molecular biology of cellular transformation have been previously covered in Chapter 1 and will not be repeated here. Being of specific importance to endocervical neoplasia, however, some additional features are worth reviewing. In addition to HPV association, there are distinctly identified risk factors associated with the development of glandular (as opposed to squamous) lesions. The two types of cancers share cofactors associated with the sexually transmitted nature of an HPV-associated disease, such as number of sexual partners and age of first intercourse. However, epidemiologic studies have determined that other cofactors for adenocarcinoma appear to be more similar to those noted for endometrial adenocarcinomas. Endocervical adenocarcinoma is more highly associated with non-smokers and lower parity than are squamous carcinomas. Adenocarcinomas and their precursors have been shown to be associated with hormonal factors, such as use of oral contraceptives and hormone replacement therapy. These types of cofactors suggest that, while oncogenesis may be primarily associated with the effects of HPV, differentiation along glandular or squamous lines may be more closely tied to the effects of these cofactors, and their interactions with the HPV-mediated process (see below).
High-risk HPV types 16 and 18 are the most prevalent oncogenic viruses found in cervical specimens and together constitute the viral types associated with over 70% of high-grade lesions and invasive carcinomas. Squamous cell carcinomas are associated, in a large predominance of cases (70+%), with HPV 16. Cervical adenocarcinomas are most commonly associated with HPV 18; however, HPV 16 is also present in a percentage ranging between approximately 30% and 40%. Interestingly, geographic variants of HPV 16 and 18 appear to be preferentially present in adenocarcinomas as opposed to squamous carcinomas. Data from differing geographic populations studied also suggest that geographic variants may react differently in various populations. This suggests that, because viral and human evolution appear to be linked, unknown mechanisms of interaction between virus and host (e.g., HLA status) may alter phenotypic outcomes. Adenocarcinomas have been shown to be more commonly associated with non-European (specifically Asian American) variants of both HPV types 16 and 18. Variant HPVs have been postulated to have differing performance characteristics in terms of oncogenicity (e.g., p53 degradation and cellular transformation efficiency may be different between variants, and may account for differing behaviors among carcinomas). In addition, poorly characterized risk cofactors as mentioned earlier, such as smoking and hormone use, may interact in different ways with variant forms of HPVs, leading to alternative differentiation patterns – providing some insight into why progenitor cells infected by HPV might differentiate as squamous or adenocarcinomas. In that vein, investigators have identified variants of HPV commonly associated with adenocarcinomas that have structural changes in portions of the genome involved with estrogen responsive elements. This finding may begin to explain why adenocarcinomas of the cervix have risk factors more akin to the “hormone-related” risk factors of endometrial carcinogenesis, including exogenous hormone use, nulliparity, and obesity. Interestingly, some variants are more commonly associated with preinvasive lesions but less commonly associated with invasive carcinomas, again indicating that some variants may be more powerful in their transforming capabilities. Needless to say, studies into these areas are ongoing at present and are likely to lead to new discoveries regarding the interaction of virus type, type variants, and other cofactors which may control both cancer development and the ultimate histogenesis.
Endocervical AIS represents the most differentiated neoplastic lesion that can be specifically recognized on histologic and cytologic preparations. AIS was originally described in 1953 by Friedell and McKay. Although many attempts have been made to identify precursor lesions to AIS, no system has yet been devised to reliably classify and predict the behavior of so-called “low-grade endocervical dysplasias.” Of note, in the first edition of The Bethesda System manual published in 1994, AIS itself was not felt to be well enough defined morphologically as to be reproducible enough to warrant its own cytologic classification. Hence, it was placed in the category of “atypical glandular cells of undetermined significance, probably neoplastic.” In the explanatory notes the authors make the following statement which accurately reflected the general state of practice at the time:
The category of atypical endocervical cells encompasses a broad morphologic spectrum of changes that exceed reactive change but fall short of frankly invasive adenocarcinoma. Accordingly, lesions in this category can range from benign, but atypical-appearing reactive processes, to adenocarcinoma in situ (AIS).
In the conference leading up to the second edition of The Bethesda System published a decade later, a review of the ensuing literature and practice in cytopathology made clear that recognition of the cytologic features representative of AIS and the reliability and reproducibility with which they could be detected in routine conventional or liquid-based specimens made a separate categorization of AIS appropriate. However, based on review of available data, lesions less than AIS could still not be reliably detected and categorized, and hence such cytologic presentations remained in the “atypical glandular cells” category (see below).
AIS has been well characterized as a precursor lesion of invasive endocervical adenocarcinoma. Its mean age of presentation is substantially lower than that of invasive adenocarcinoma, with reported ranges as much as 12 years to 18 years earlier, indicating that it long precedes the development of the invasive lesion. AIS shares many of the same epidemiologic risk factors as invasive endocervical adenocarcinoma, is associated with HPV in virtually all cases, and shows HPV type 18 to 16 ratios similar to those of its invasive counterpart. In addition, resected specimens of invasive adenocarcinoma typically show adjacent areas of well-defined AIS. Squamous dysplasias are commonly identified in association with AIS. Some studies report the figure to be as common as 50%, although, in recent experience, this author has noted more than 50% of cases unassociated with a squamous component.
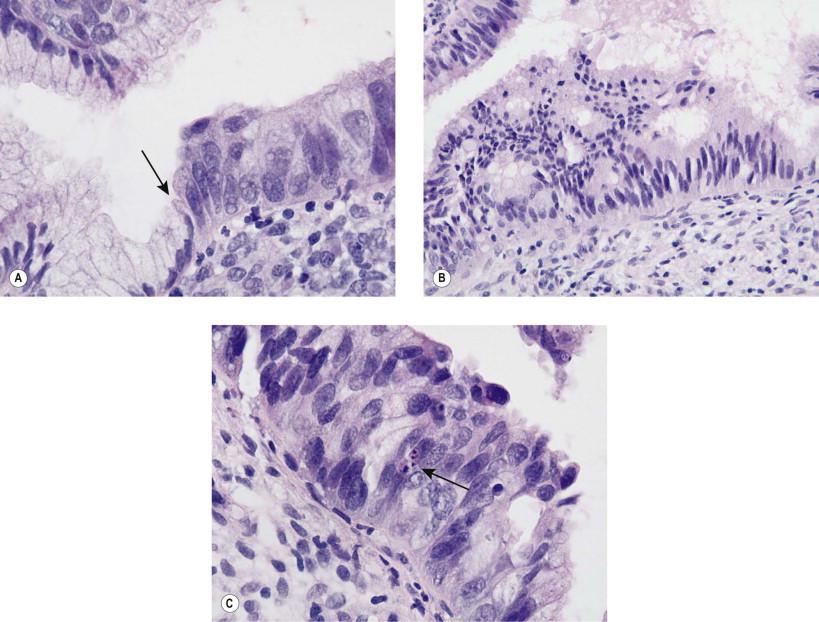
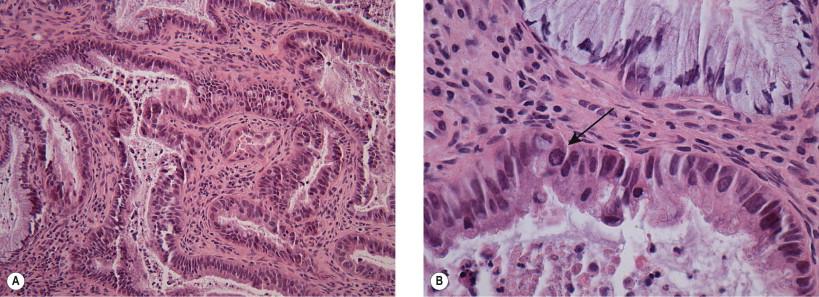
Histologically, the characteristic features of AIS involve a completely or partially replaced area of surface epithelium and/or endocervical glands, with no evidence of stromal invasion. The epithelium is typically pseudostratified, with nuclei that are enlarged and elongated, showing hyperchromasia and an evenly distributed, but coarsely granular chromatin. Architecturally, intraepithelial gland formation and cribriform features can be seen. Mitoses and apoptotic bodies are commonly noted ( Fig. 9-10 ).
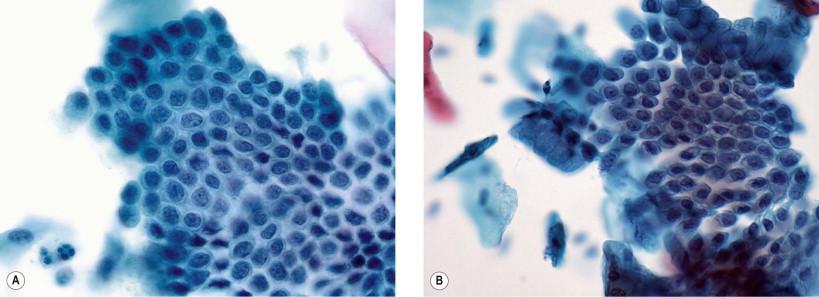
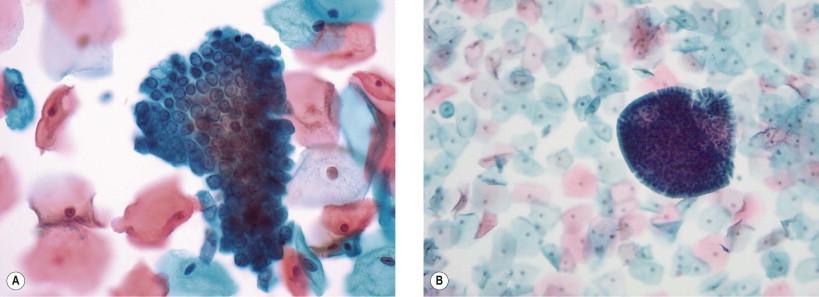
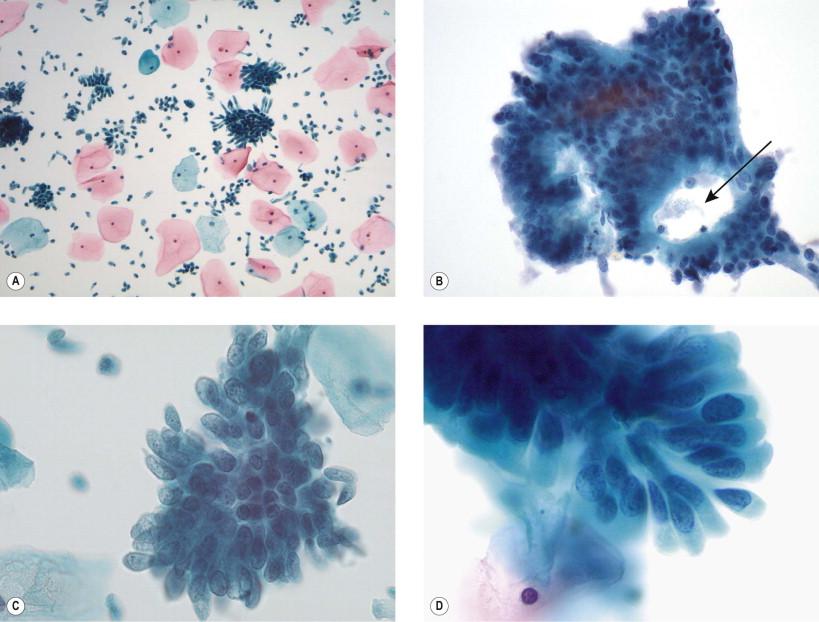
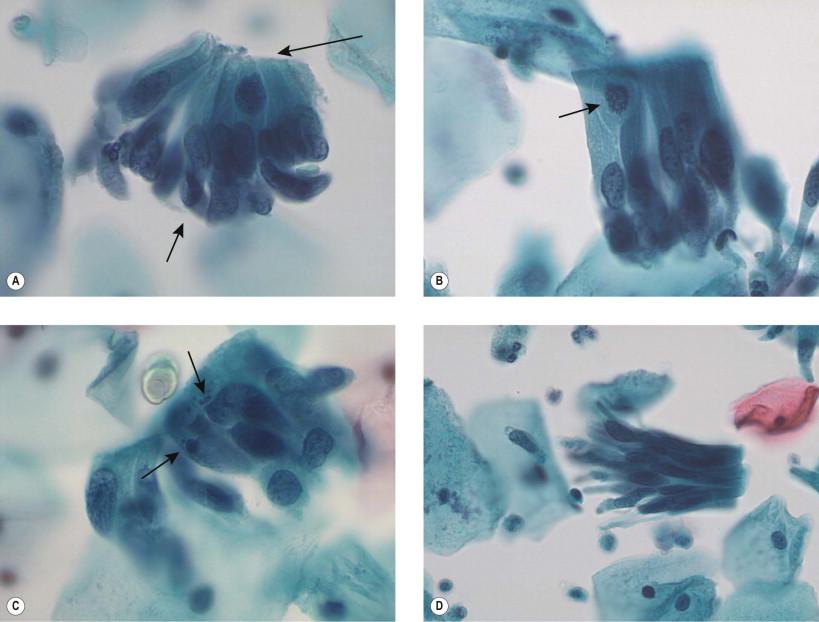
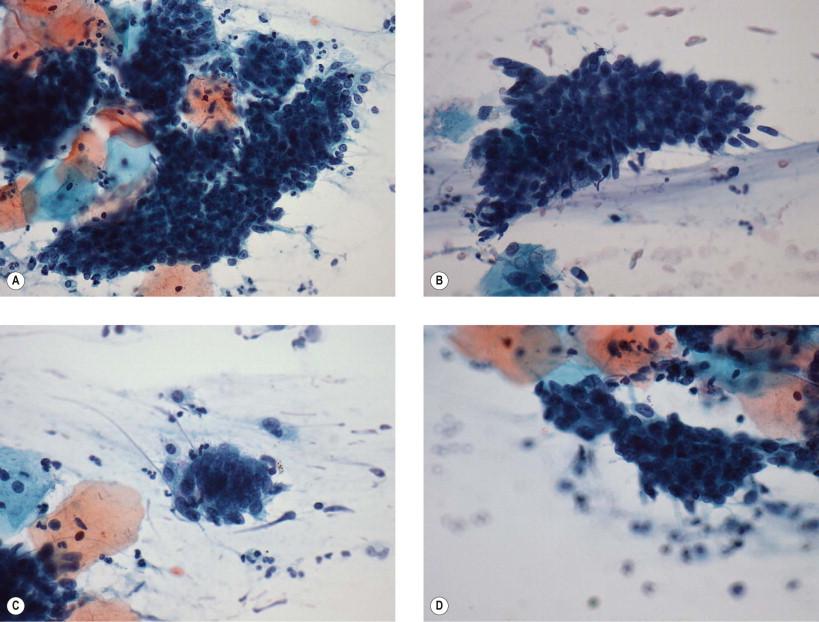
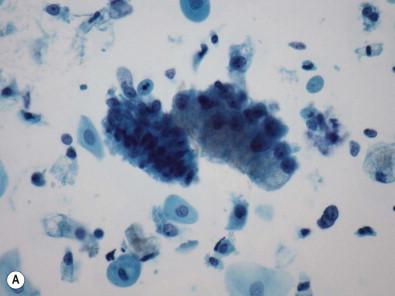
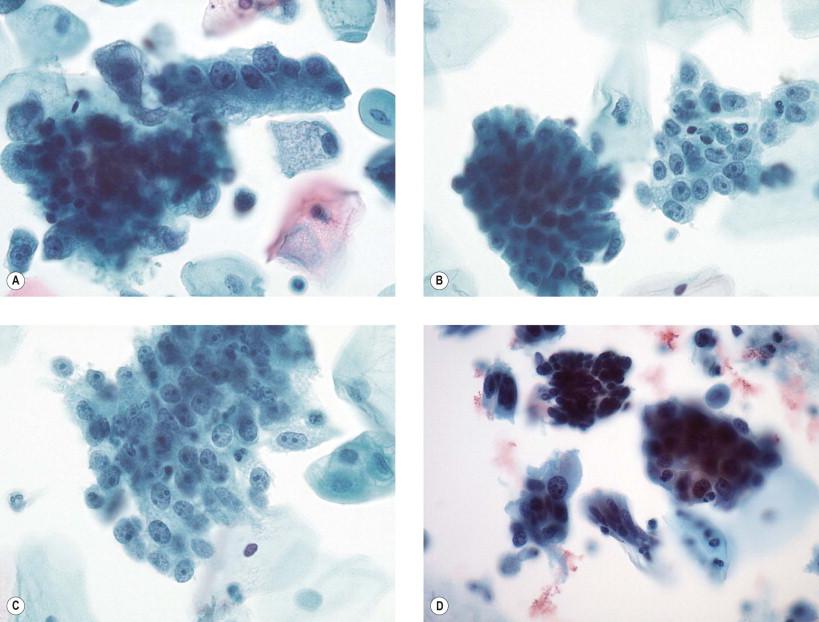
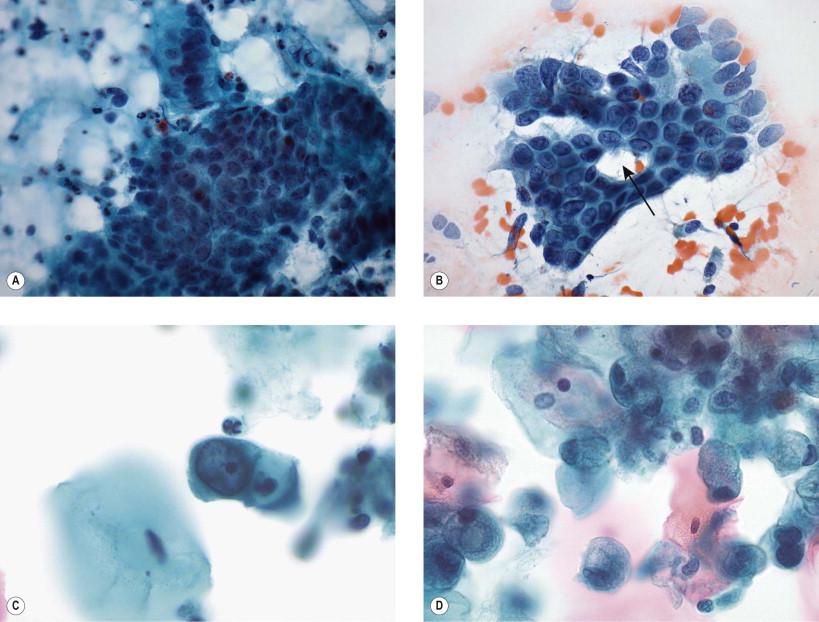
The cytologic features were described (if not well recognized or applied) in the early 1970s. The first organized descriptions of the cytologic features of AIS appeared in the late 1970s and 1980s. Derived from these earlier works, the currently recognized cytologic criteria for AIS are compiled in the second edition of The Bethesda System and include both architectural and cytologic features. Architectural features include the presence of hyperchromatic crowded groupings of cells with prominent cellular and nuclear overlapping. Additional groupings may include pseudostratified strips of cells, the formation of epithelial rosettes, and honeycombed arrangements with disorganization and nuclear overlapping (not showing the uniform rigidity noted with honeycombed groupings of benign endocervical cells). Margins of the groupings may show palisading and a characteristic protrusion of cytoplasmic and nuclear “tags,” a feature aptly named “feathering.” This change occurs when the basal portion of the cell is stripped from the underlying basement membrane, leaving a portion of the cell elongated. Nuclei are enlarged – on average about two-fold the size of the intermediate squamous cell nucleus – but significant size pleomorphism can be present. The nucleus to cytoplasmic (N : C) ratio is higher than for normal endocervical cells. The nuclei are oval to elongate, hyperchromatic, and show chromatin patterns which are evenly dispersed, but coarsely granular. Nucleoli are small and inconspicuous. Mitoses and apoptotic bodies are commonly found. Occasional isolated abnormal columnar cells can be present, but these are generally far less in number than cells that present as groups. Slide backgrounds are generally clean, but occasionally an inflammatory background can be noted. Examples of these criteria are illustrated in Figs 9-11 and 9-12 . Dysplastic squamous cells are present in association in a significant number of cases, and focusing on this more commonly seen lesion can lead to lack of identification of the extant abnormal glandular process.
Hyperchromatic crowded groupings of cells
Pseudostratified strips of columnar cells
Epithelial rosettes (gland formations)
Nuclear and cytoplasmic “feathering”
Nuclear size two-fold greater than normal endocervical nuclei
N : C ratio increased beyond normal endocervical cells
Coarsely granular, evenly distributed hyperchromatic chromatin
Possible presence of small nucleoli
Presence of mitotic figures and apoptotic bodies
Not associated with a background “tumor” diathesis.
Most original reports of the cytologic features of AIS were from conventionally smeared Papanicolaou slides. Recently, reports detailing the differences that can be present in the now far more common liquid-based cytology preparations have appeared. Although virtually all reports have indicated that AIS can be identified in liquid-based specimens with a high degree of accuracy and reproducibility, the Bethesda System reported liquid-based preparation criteria that indicated that AIS may present in smaller and denser 3-dimensional groupings, making visualization of individual cells (and hence their specific cytology features) more difficult. Pseudostratified strips of cells, often in a “bird-tail”-like arrangement ( Fig. 9-12 ), as opposed to the more commonly identified feathered hyperchromatic crowded groups seen in conventional smears, may be a more characteristic feature of AIS presenting in liquid-based preparations. Liquid-based fixation has been postulated to blunt the feathered edges of such groups, which in conventional slides were accentuated due to the flattening and smearing of the specimen. Nuclear chromatin is more often noted to be finely granular, and nucleoli are more prominent, both results of early and more complete fixation than can routinely take place in conventional slides. Although perhaps not less sensitive for the detection of glandular entities (grouped together), exact classification of glandular lesions as AIS, as opposed to atypical glandular cells, not otherwise specified (AGC, NOS), or atypical glandular cells, favor neoplasia (AGC, favor neoplastic), has been found by this author to be at times more challenging in liquid-based specimens than with conventional slides. Other studies have documented changes in appearances of AIS and AGC on liquid-based specimens. One study described improvements in nuclear features on liquid-based preparations, but more “subtle” architectural changes.
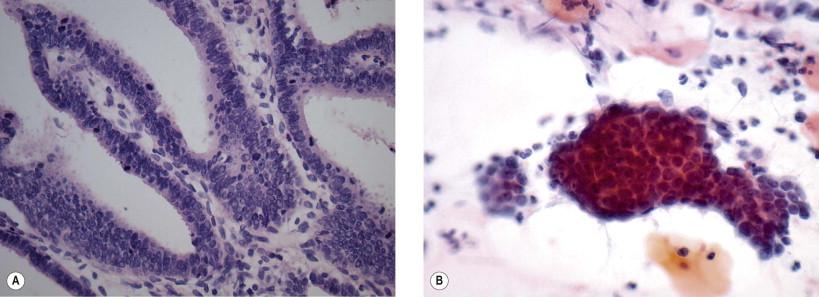
Although most endocervical AIS are of the usual “endocervical” type, recapitulating the characteristic endocervical epithelium described and illustrated in the histology section ( Fig. 9-1 ), it is important to recognize that rarely other variants of Mullerian and gastrointestinal differentiation can occur. These include endometrioid, serous, and intestinal variants. Of these, the most significant from a differential diagnostic point is the endometrioid pattern ( Fig. 9-13 ). In a study of cases of AIS of the endocervix, this pattern contained small cells in densely packed groups, having coarse nuclear chromatin, and showing lack of pleomorphism. These groups were more commonly misinterpreted as of benign endometrial or endocervical origin. Criteria were developed to identify these cases as abnormal (at least to the level of atypical glandular cells):
The absence of endometrial stromal cells and endometrial-like tubules
Coarse chromatin patterns
Extreme nuclear crowding
Mitotic figures
Marginal feathering.
Serous forms of AIS are hypothesized to exist but are extremely rare. They may show typical “hobnail” groupings and reportedly may also have ciliated cells intermixed. However, personal experience of this author would suggest that ciliated cells are far more commonly found in benign processes, with some putatively malignant conditions actually representing “false-positive” benign mimickers. Intestinal variants show the presence of goblet cells; however, one study notes that goblet cells may be difficult to identify in cytologic preparations and these lesions show otherwise similar nuclear and architectural features when compared to the usual type of “endocervical” AIS.
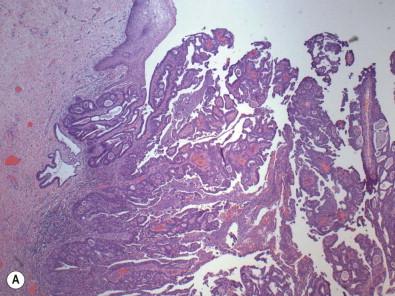
A very comprehensive review of endocervical adenocarcinoma and its histologic variants was performed by Young and Clement in 2002 ( Table 9-1 ). The “typical endocervical type” of endocervical adenocarcinoma constitutes about 80% of primary cervical adenocarcinomas, and is most often “mucin poor” ( Fig. 9-14 ). Variants exist in which variable amounts of mucin are present, up to and including so-called “mucinous” variants showing abundant intracytoplasmic mucin. These neoplasms are generally moderately differentiated and composed of glands of medium size. Cells have a characteristic eosinophilic cytoplasm, are columnar, and show architectural stratification. Invasive components may show small irregularly spaced glands or glands in lobular units. Occasional solid areas may be noted. Usual types of endocervical adenocarcinomas may show papillary surface features, but should not be confused with the villoglandular variant that shows predominantly tall thin surface papillae that have stromal fibrous cores ( Fig. 9-15 ). In this variant, invasive components show elongated branching glands separated by fibrous stroma, occasionally showing a desmoplastic or myxoid stromal reaction. Individual cells show features similar to well, or at worst moderately, differentiated usual types of adenocarcinomas, and also often show adjacent areas of AIS. Typically only minimal invasion is noted in these tumors and they are generally noted to have a better prognosis than usual types. The authors mention that this designation should be reserved for tumors with no areas showing the more usual type of adenocarcinoma and should always be morphologically low grade, to ensure that a better than expected prognosis is not given to a more aggressive neoplasm. Villoglandular variants typically present in a younger age population (median in the mid-fourth decade) and, because of the exophytic nature of this tumor, present with abnormal cervical cytology in up to 75% of cases.
| TYPICAL ENDOCERVICAL TYPE |
|
| MUCINOUS |
|
| ENDOMETRIOID |
|
| CLEAR CELL |
| SEROUS |
| MESONEPHRIC |
Gastric-type mucinous carcinomas are rare variants which have been associated with mutations in the STK11 tumor suppressor gene on chromosome 19p (associated with Peutz–Jeghers syndrome). These tumors show evidence of pyloric-type differentiation including pyloric-type mucin production (MUC6 and HIK1083). So-called “adenoma malignum” or minimal deviation adenocarcinoma is a very well-differentiated gastric-type mucinous carcinoma which has a deceptively bland histologic appearance ( Figs 9-16–9-18 ). Gastric-type mucinous endocervical adenocarcinoma is the tumor most commonly noted to be non-HPV-associated for which an alternative pathogenesis is suggested. Microscopically, it consists of close to widely dispersed glands within the stroma which vary in size and may be round to irregular with occasional papillary infolding. Glands are lined by mucin-producing cells showing cuboidal configuration and bland nuclear features. In most cases, however, areas of more malignant epithelium will be noted and a desmoplastic stromal reaction is commonly identified.
Intestinal variants of endocervical adenocarcinoma show goblet or signet ring cells which may be intermixed with Paneth and argentaffin cells. Young and Clement note that true endometrioid carcinomas of the endocervix are rare, accounting for about 7% in a recent series. When present, these tumors show endometrioid tubular and villous formation akin to endometrial adenocarcinomas ( Fig. 9-19 ). Clear cell and serous carcinomas of the endocervix closely resemble their counterparts in other locations in the gynecologic tract. Clear cell carcinoma of the cervix shows one or a mixture of tubulocystic, solid, and papillary architecture. Serous carcinoma shows the typical hobnailing papillae and slit-like glandular spaces seen in ovarian neoplasms of this type.
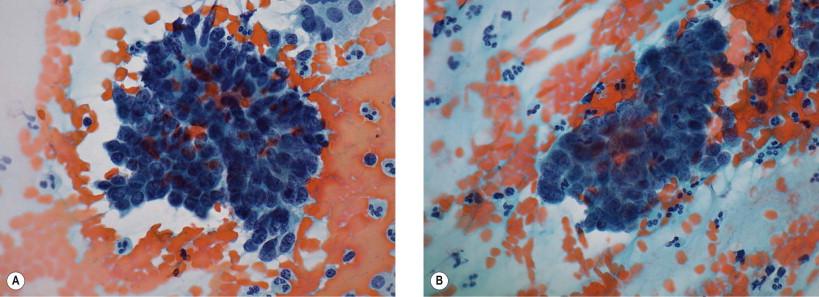
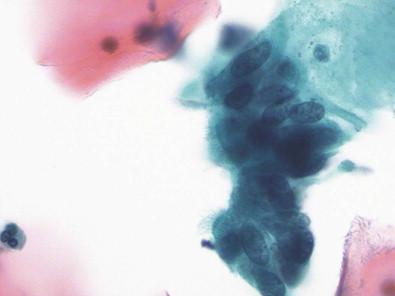
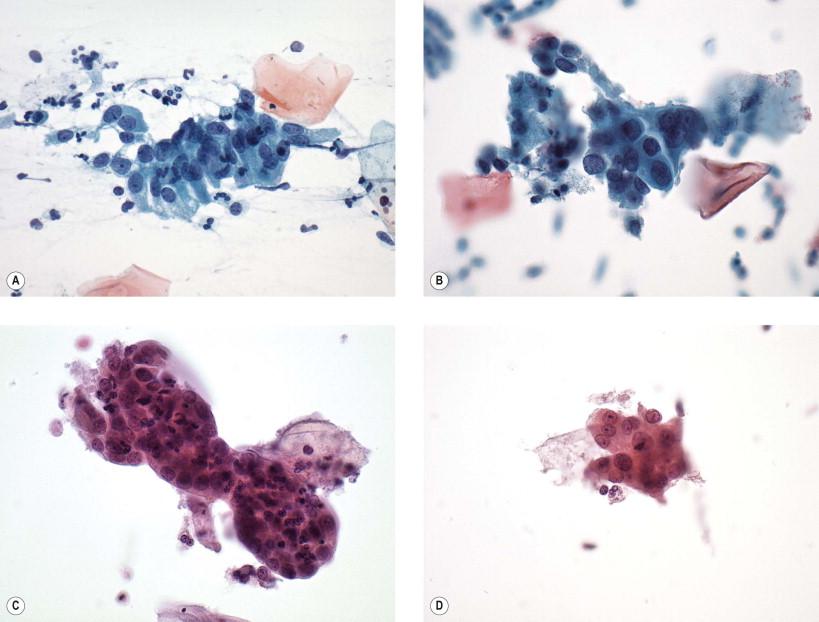
In the most common forms of endocervical adenocarcinoma, the stated Bethesda System cytologic criteria for diagnosis may overlap with those for AIS. Particularly, in well-differentiated variants of invasive adenocarcinoma, cytologic features distinguishing in situ from invasive lesions may be subtle and include changes in nuclear chromatin and background patterns. In addition, AIS is often found in association with invasive carcinoma and hence cells may be sampled from both lesions and will be intermixed on the slide. Because endocervical adenocarcinomas are likely to be found within reach of the sampling device, cells are most often configured architecturally as “traumatically” or directly sampled presentations. These architectural patterns include abundant abnormal cells, showing evidence of a columnar configuration – including pseudostratified strips of cells or honeycombed 2-dimensional sheet-like arrangements ( Fig. 9-20 ). Three-dimensional groupings or syncytia can also be present particularly when lesions exfoliate cells from higher in the endocervical canal. Such cells have “exfoliative” features and will “ball-up” into more dense, spherical shapes as they float in the endocervical mucus. The typical architectural features of AIS, including epithelial rosette formation, pseudostratified strips of cells, and marginal feathering of cells in groups, may be noted, but these features will become ill-defined and more difficult to recognize as lesions become more poorly differentiated. Nuclei are enlarged (generally >2–3 times the size of an intermediate squamous cell nucleus) and pleomorphic, and show irregular chromatin with areas of “clearing.” Macronucleoli are commonly evident. The cytoplasm is finely vacuolated to granular and may show columnar configuration. Again, in tumors of poorer differentiation, the nuclear features will increase in their atypicality. Mitoses and apoptotic bodies are commonly noted. Individual tumor cells are present due to the discohesive nature of these lesions. Tumor diathesis is generally present, indicative of tumor and host necrosis and concurrent inflammatory reaction ( Fig. 9-21 ). However, in low-grade and minimally invasive tumors, diathesis may be absent or minimal.
Large numbers of abnormal cells present with many isolated cells
Cells present in “directly sampled” architectural patterns
Disorganized honeycomb sheets
Pseudostratified and stratified strips
Isolated cells with columnar configuration
Papillae or villous formations possible in variants
Cells from high canal lesions may present in “exfoliative” patterns
Spherical hyperchromatic crowded groups
Syncytial groups
Isolated round to oval cells
Architectural features of AIS may be retained in well-differentiated lesions
Feathered group edges
Rosette formation
Pseudostratified strips
Necrotic and bloody tumor diathesis commonly present
Nuclei enlarged (>2–3 times the size of an intermediate squamous cell nucleus) and may show pleomorphism of size and shape
N : C ratio is increased
Chromatin is coarsely granular with heterogeneity and clearing
Macronucleoli are common
Mitoses and apoptotic bodies are commonly seen
Cytoplasm is generally granular and finely vacuolated
Variant types can show abundant mucin, signet ring, goblet cell, and/or serous types of differentiation.
In liquid-based preparations, adenocarcinomas show accentuated 3-dimensionality of groups due to the liquid medium immersion and fixation. This feature may make evaluation of central cells in hyperchromatic crowded groupings difficult to interpret. Again, excellent and rapid fixation leads to a more open chromatin pattern with less chromatin irregularity. Tumor diathesis may be less prominent and when present will take on a clumped or “clinging” nature adhering to cells, rather than as a diffuse background appearance as seen in conventionally prepared slides.
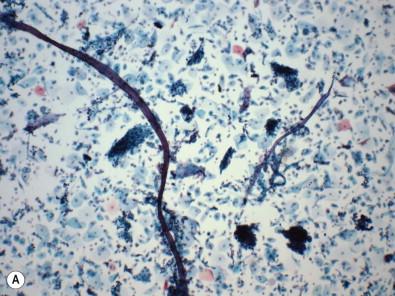
The cytologic features of some of the rare variants of endocervical adenocarcinoma have been documented. The villoglandular pattern shows palisading of nuclei within tufted groups, with nuclei that may be spindled or columnar. Well-differentiated mucinous adenocarcinoma (adenoma malignum or minimal deviation adenocarcinoma) has been described and shows abundant mucin-rich endocervical cells arranged in a variety of patterns including mono- and multilayered sheets and 3-dimensional aggregates ( Fig. 9-18 ). The groups show significant nuclear overlapping and some degrees of pseudostratified strip formation. The individual cells show nuclear atypia, which ranges from subtle to frankly malignant, with nucleoli present. Two reports stress the presence of “golden-yellow” appearing mucin within cells, which was found to be a distinctive cytologic feature in cases of adenoma malignum ( Fig. 9-18A,B ). In a report studying the cytology from seven cases of adenoma malignum, the authors concluded that abnormal cells would be difficult to distinguish from reactive endocervical cells in cases where a more poorly differentiated component was not present within the tumor. They did state, however, that large numbers of endocervical cells in sheets with nuclear enlargement is a key feature to note in difficult cases. Suffice it to say that close attention to cellularity and a careful search among the abundant cells present for features of malignancy, or at a minimum, atypicality are key to making an appropriate interpretation of at least “atypical glandular cells” which would prompt appropriate further investigation. Differentiation of primary endocervical from metastatic adenocarcinoma, particularly from the colon, can be difficult. Colonic adenocarcinomas can show many of the same features as endocervical lesions, including pseudostratified architecture and the presence of goblet cells. Because most colonic metastasis is via direct extension, or via a fistula tract into the vagina or cervix, the background can be very important in the assessment. Colonic adenocarcinoma can show abundant degrees of necrosis and the presence of vegetable material from the colon. A background pattern containing these elements should bring metastasis into the differential diagnosis ( Fig. 9-22 ).
The detection of glandular lesions of the cervix is a secondary role (after squamous lesion detection) of the Papanicolaou test. As has been noted earlier, endocervical neoplastic processes are a minority of lesions as compared to the more common squamous cancers and their precursors. That being said, endocervical glandular neoplasias can and should be identified on cervical cytology examinations when appropriate cytologic features are present. The morphologic characteristics of these lesions are now well described and have been shown to be reliably predictive. Improvements in sampling devices and techniques for analyzing the upper regions of the endocervical canal have increased the sensitivity for detection and interpretation, but have also presented new challenges to the specificity of interpretation. Just as in squamous lesions, there has always been a level of morphologic uncertainty in some (often a majority) of specimens showing not completely normal endocervical cytology, but yet not having the absolutely specific features of a diagnosable AIS or invasive carcinoma. In the 1991 version of the Bethesda System (TBS 1991), such changes were referred to as “atypical glandular (endocervical) cells of undetermined significance (AGUS).” In the current 2001 Bethesda System (TBS 2001) terminology, this nomenclature has changed to “atypical glandular (endocervical) cells (AGC).” The dropping of the “of undetermined significance” was done as a practical consideration of the difficulties faced in busy practitioners' offices, based on confusion with the far more prevalent “atypical squamous cells of undetermined significance” (ASC-US) slide designation. In addition, the general categorization portion of the cervical cytology report was further divided into “Epithelial cell abnormality – squamous or glandular” to indicate the broad designation of lesion class prior to the more specific interpretation. As will be noted, AGC is clinically a more significant interpretation requiring more rigorous and different follow-up than ASC-US, and hence a non-overlapping name was felt to be required.
In TBS 1991, AGUS was subdivided into three categories related to a morphologic assessment of the risk that a true neoplastic lesion was present. These included “favor reactive,” “not otherwise specified,” and “favor neoplastic” distinctions. Data presented at the 2001 Bethesda conference showed that the “favor reactive” and “not otherwise specified” categories had similar and significant (in terms of high-grade neoplastic lesions) clinical follow-up ( Table 9-2 ). Hence, the “favor reactive” category was merged into the “not otherwise specified” category with the proviso that changes interpreted as being truly reactive or reparative should be classified into the overall negative for intraepithelial lesion or malignancy (NILM) category. This leaves current TBS AGC terminology modifiers as “not otherwise specified” or “favor neoplastic.” Classification into cell of origin (endocervical, endometrial, or other) should be done when possible, with the generic “glandular” designation held for cases in which this cannot be resolved.
| Follow-Up Result | ||
|---|---|---|
| Any High-grade Lesion | High-grade Glandular Lesion | |
| AGUS, favor reactive | 5–39% | 1–8% |
| AGUS, NOS | 9–41% | 0–15% |
| AGUS, favor neoplastic | 27–96% | 10–93% |
Atypical endocervical cells are defined in TBS 2001 as “endocervical-type cells (that) display nuclear atypia that exceeds obvious reactive or reparative changes, but that lack unequivocal features of endocervical adenocarcinoma in situ or invasive adenocarcinoma.” Criteria that can be present with atypical endocervical cells (AEC), not otherwise specified, include endocervical type cells in sheets or strips with some crowding and nuclear overlap, nuclear enlargement (3–5 times the size of normal endocervical cell nuclei) with variability of size and shape, mild hyperchromasia and nucleoli, and mitoses. The N : C ratio may be increased ( Fig. 9-23 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here