Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Four modalities of Doppler echocardiography are currently available for use with a wide variety of applications: pulsed-wave (PW) Doppler, continuous-wave (CW) Doppler, color-flow imaging, and tissue Doppler imaging. The various Doppler modalities each complement M-mode and two-dimensional (2D) or three-dimensional (3D) B-mode structural data with hemodynamic (CW and PW Doppler and color-flow Doppler) and functional (tissue Doppler imaging) data. Doppler echocardiography is the modality on which noninvasive assessment of cardiac hemodynamics depends. The purpose of this chapter is to review the normal antegrade intracardiac flow using PW and CW Doppler.
Christian Johann Doppler (b. 1803) first observed that when a sound source and observer are moving closer together, the observed frequency of the sound is higher than when the source and observer are both not moving, and when the sound source and observer are moving away from each other, the observed frequency is lower than when not moving. The Doppler shift or frequency is proportionate to the velocity of movement between the source and observer. This principle applies equally to ultrasound backscattered by moving blood cells in the beating heart:
In this equation, ΔF represents the Doppler shift, V is the velocity of tissue, F0 is the transducer frequency, cosθ is the cosine of the angle of incidence between the direction of flow and the long axis of the ultrasound beam, and C is the speed of sound in tissue. All commercially available ultrasound machines calculate the velocity of blood flow by assuming that the average speed of sound in the body is 1540 m/s and that the ultrasound beam is parallel to flow so that cosθ=1:
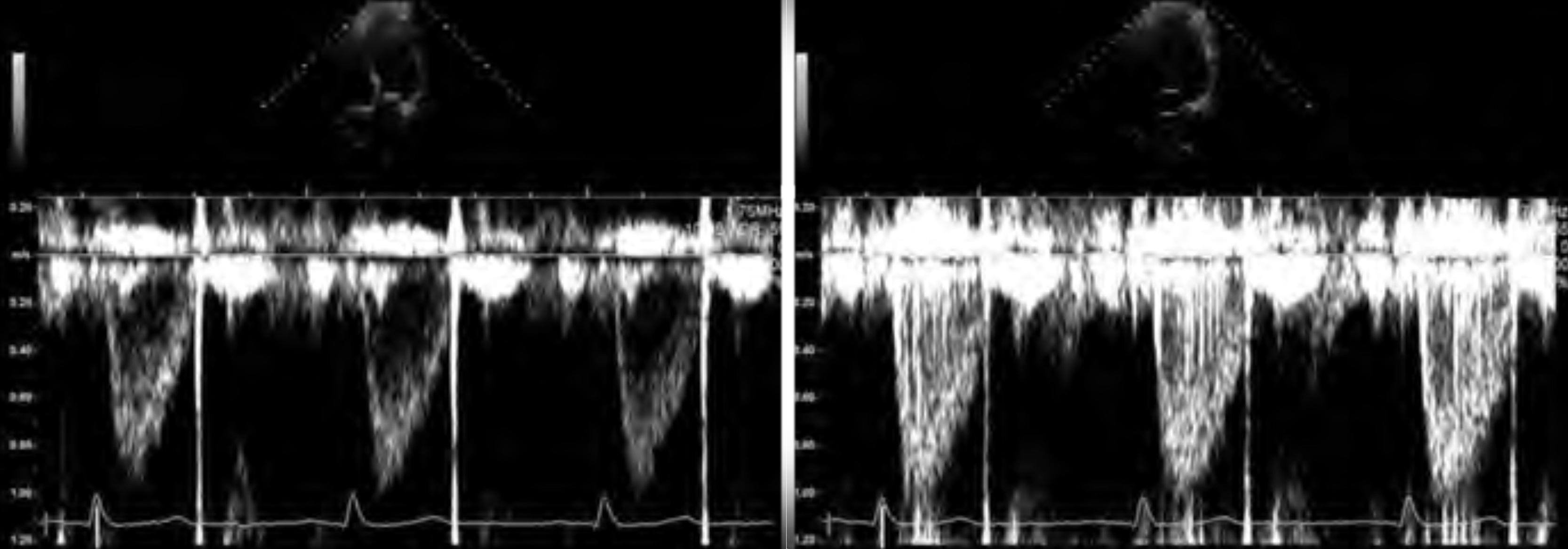
Quantification of flow velocity is obtained with either PW or CW Doppler. PW Doppler records velocity at one specific location, whereas CW Doppler records flow velocity along the entire pathway of the ultrasound beam ( Fig. 11.1 ).

CW Doppler permits accurate measurement of any flow velocity but cannot determine the location of the peak velocity it measures because all velocity signals along the length of the ultrasound beam are merged into one reflected signal. The reflected Doppler signal is converted to a velocity and displayed as a spectrum with velocity on the y -axis and time on the x -axis. By convention, flow toward the transducer is displayed, spectrally, above the zero baseline and flow away, below the zero baseline. CW Doppler is used to measure high velocities across stenotic or regurgitant valves.
PW Doppler can measure flow at a precisely defined location but with a more limited range of measurable velocities. PW Doppler is used to assess velocities across normal valves or vessels to calculate flow and assess cardiac function. PW Doppler velocity spectra can be displayed and measured similar to CW Doppler. Because PW Doppler allows measurement of velocity at a specific anatomic site, the 2D echocardiographic measurements of a valve or orifice can be combined with PW flow data to calculate stroke volume (SV), cardiac output (CO), and measurement of diastolic filling parameters. PW Doppler of multiple sample regions can also be displayed as a color map integrated into a 2D or 3D echocardiogram to screen for flow acceleration (stenosis) or regurgitation.
Daniel Bernoulli (b. 1700) described the phenomenon by which the increase in velocity of a fluid occurs simultaneously with a decrease in pressure (potential energy). Doppler frequencies therefore correspond to pressure gradients in the heart that can be calculated using the simplified Bernoulli equation:
in which ΔP represents the pressure gradient and V represents the blood flow velocity. Common clinical applications include estimation of pressure gradients across valves and estimation of pulmonary artery pressure from the velocity of tricuspid regurgitation.
Ultrasound machines calculate velocity from the Doppler shift with the assumption that flow (or motion) is parallel to the ultrasound beam. Incident angles smaller than 20 degrees produce errors smaller than 6% based on this assumption but more oblique angles produce significant errors as the (unmeasured) cosθ increases rapidly above 30 degrees. Color Doppler and anatomic landmarks may be helpful to identify the likely direction of flow for alignment. Angle-correction tools available on some ultrasound systems for vascular imaging are generally not recommended for cardiac use because the true direction of flow is unknown and often dynamic in 3D space. Any clinically significant flow should be interrogated in at least two windows with different incident angles and the higher observed Doppler shift (velocity) taken as the more accurate measurement. ,
Normal flow through the cardiac chambers and great vessels is laminar, with essentially all blood cells traveling in the same direction and within a narrow range of velocities. Near the walls of vessels or when crossing a stenotic orifice, flow becomes turbulent, with blood cells moving in many directions across a wide range of velocities. Doppler sampling should be performed as near the center of the stream of flow as is feasible with adjustment of the PW sample size to capture a dense modal flow velocity with minimal spectral broadening.
Gain should be adjusted to display a smooth flow signal with a clear modal velocity. Generally, the background should show slight speckling to ensure adequate sensitivity. High gain settings may emphasize weak signals outside of the modal velocity and reduce reproducibility of measurements. The width of the PW sample volume must be adjusted to avoid spectral broadening. The wall filter removes high-intensity, low-velocity signals from Doppler spectra but can obscure the exact onset and end of the flow signal of interest when set too high ( Fig. 11.2 ).
Larger signals are more easily measured than small ones. The velocity scale should allow the Doppler tracing to be displayed as large as possible without aliasing. This generally means adjusting the baseline up or down the screen, depending on the direction of the flow signal, in addition to adjusting the scale to accommodate the observed velocity in the available height of the display. Automated tools are available on many ultrasound platforms and can quickly position the baseline, gain, and wall filter as a “starting point” for further refinement by the echocardiographer.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here