Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Peripheral arterial occlusive disease (PAD) is a major cause of disability, loss of work, and lifestyle changes. The natural history of PAD is often characterized by slow progression in symptoms over time. However, 70% of patients will remain stable or improve over time, approximately 30% will require an intervention, and 10% will require amputation. Limb loss is the tragic final outcome of PAD and is associated with a significant degree of disability and a poor overall prognosis. The aging of the population, continued tobacco abuse, high-fat diets, sedentary lifestyles, and rising prevalence of obesity parallel the increasing prevalence of PAD. The prevalence of PAD in the general population is 3% to 10%, and it is 15% to 20% among patients older than 70 years. This prevalence probably underestimates the true burden of disease, however, as PAD may be asymptomatic. Because of the rising prevalence of PAD, many cardiovascular specialists have adopted a strategy of “global vascular management” for their patients. In this strategy, the evaluation, care, and intervention plan is more comprehensive in its scope, and it includes the management of vascular disease in all of its manifestations and anatomic locations. This chapter reviews the general aspects of peripheral vascular disease, with particular emphasis on the angiographic and percutaneous interventions after medical evaluation.
The purpose of peripheral angiography is to define the vascular anatomy and to identify significant arterial narrowing that requires revascularization (either percutaneous or surgical). As with any invasive diagnostic test, the risk-benefit ratio should be evaluated before angiography to identify patients who might fully benefit from imaging.
Lower extremity claudication is classified according to the level of debilitation or restriction of activities. It is important to select the appropriate patient for angiography, given that the morbidity from vascular access might be particularly high among patients with PAD. The most commonly used clinical grading system for PAD is the Rutherford-Becker scale, a 7-point scale from 0, which denotes asymptomatic disease, to 6, which denotes major tissue loss ( Table 74-1 ). In general, patients with Rutherford scale 2 and higher and noninvasive studies that demonstrate evidence of significant disease are likely to benefit from angiography and revascularization. Any patient with symptomatically limiting lower extremity claudication should undergo angiography to fully define the anatomy with a consideration toward revascularization.
| Grade | Category | Clinical Description | Objective Criteria |
|---|---|---|---|
| 0 | 0 | Asymptomatic |
|
| 1 | Mild claudication | ||
| I | 2 | Moderate claudication | More moderate symptoms |
| 3 | Severe claudication |
|
|
| II | 4 | Ischemic rest pain |
|
| 5 | Minor tissue loss | Resting ankle pressure <40 mm Hg | |
| Nonhealing ulcers | Pulse volume recording moderately decreased | ||
| III | 6 | Major tissue loss | As noted in category 5 |
| Loss above the metatarsal limb no longer salvageable |
Angiography is indicated in patients with threat of limb loss owing to acute thromboembolism. Patients with acute onset of a cool, pulseless extremity after catheterization or trauma require angiography to define the anatomy and site of occlusion in addition to allowing the direct infusion of intra-arterial fibrinolytic therapy or mechanical or rheolytic thrombectomy if necessary.
Angiography may be warranted among patients with an abdominal aortic aneurysm or thoracic aneurysm to fully delineate the anatomy, particularly if endovascular repair is considered. However, given current noninvasive imaging techniques, such as magnetic resonance angiography and computed tomographic angiography, it is unlikely that invasive angiography is necessary to define anatomy among patients who are at low surgical risk, in whom an open repair may be most beneficial. Only if invasive angiography answers a particular question (e.g., the angle of the aneurysm neck) that cannot adequately be answered with noninvasive imaging should peripheral catheterization be pursued.
Magnetic resonance angiography may also be useful in the evaluation of coarctation of the aorta. When angiography is needed, anteroposterior (AP) and lateral images are the most useful for patients with coarctation who have not been operated on. Angiography usually confirms the anatomic coarctation, invariably seen just distal to the origin of the left subclavian artery. Further, if the head and neck vessels are imaged with the thoracic aorta, an idea of collateral flows can be inferred as well (i.e., carotid or mammary).
Invasive renal angiography is indicated in patients who have evidence of significant stenosis on noninvasive testing, such as magnetic resonance angiography and Doppler ultrasonography. Other indications include new uncontrolled hypertension in patients younger than 30 years or older than 55 years, refractory hypertension, rising creatinine concentration (specifically after the institution of angiotensin-converting enzyme inhibitor therapy), or unexplained acute pulmonary edema. The prevalence of renovascular hypertension may be as high as 5% in the general population and 30% among patients with coronary artery disease or other PAD.
Because of the multiple-source blood supply to the upper extremity, which is derived principally from the subclavian and vertebral arteries, upper extremity claudication is rare. Upper extremity claudication symptoms include an inability to perform activities with the affected limb, such as combing hair, brushing teeth, or repeated lifting. Another constellation of symptoms indicating obstructive disease in the upper extremity may come from significant obstruction in the posterior circulation. In this situation, there is a reversal of flow from the vertebral artery in a patient with disease in the ipsilateral vertebral artery, leading to dizziness or difficulties with gait. Among patients who have undergone coronary artery bypass graft surgery with use of the internal mammary artery, persistent angina and anterior ischemia on noninvasive testing may suggest left subclavian stenosis as the cause of coronary ischemia. Therefore, any patient with symptoms of upper extremity claudication, anterior ischemia after coronary artery bypass grafting with the use of the left internal mammary artery, or posterior circulation events and a difference in upper extremity blood pressures should be evaluated for the possibility of subclavian stenosis and undergo evaluation, including angiography.
A critical stenosis of one or both carotid arteries on noninvasive imaging or evidence of transient ischemic attack or stroke and a critical stenosis identified on noninvasive testing is an indication for invasive carotid or cerebral angiography.
The principal contraindications to peripheral angiography are bleeding diathesis, renal failure (true or impending), fever, ongoing infection, and severe anemia ( Box 74-1 ).
Bleeding diathesis or inability to take aspirin or adenosine diphosphate inhibitor
Concurrent febrile illness
Severe renal insufficiency or anuria without dialysis planned
Severe allergy to contrast agents
Severe hypokalemia or digitalis toxicity
Severe hypertension or ongoing unstable coronary syndrome
Complications of invasive peripheral angiography primarily involve vascular access site complications, catheter manipulation within atherosclerotic vessels, emboli, clot formation, stroke, myocardial infarction, worsening renal function, or congestive heart failure ( Box 74-2 ). A particularly devastating complication of catheter manipulation within the arterial tree is an atheroembolic event. In its most severe form to the lower extremities, it may cause loss of limb or digits. Likewise, emboli to the renal circulation can lead to acute renal decompensation or failure requiring dialysis. Pseudoaneurysm or vascular access complications can be as high as 3% in patients with severe peripheral occlusive disease.
Vascular access dissection or perforation: 0.1%-0.2%
Bleeding or hematoma: 1.5%-2.0%
Allergic reaction: 0.5%-2.0%
Vasovagal events: 1.0%-2.0%
Death: 0.1%-0.2%
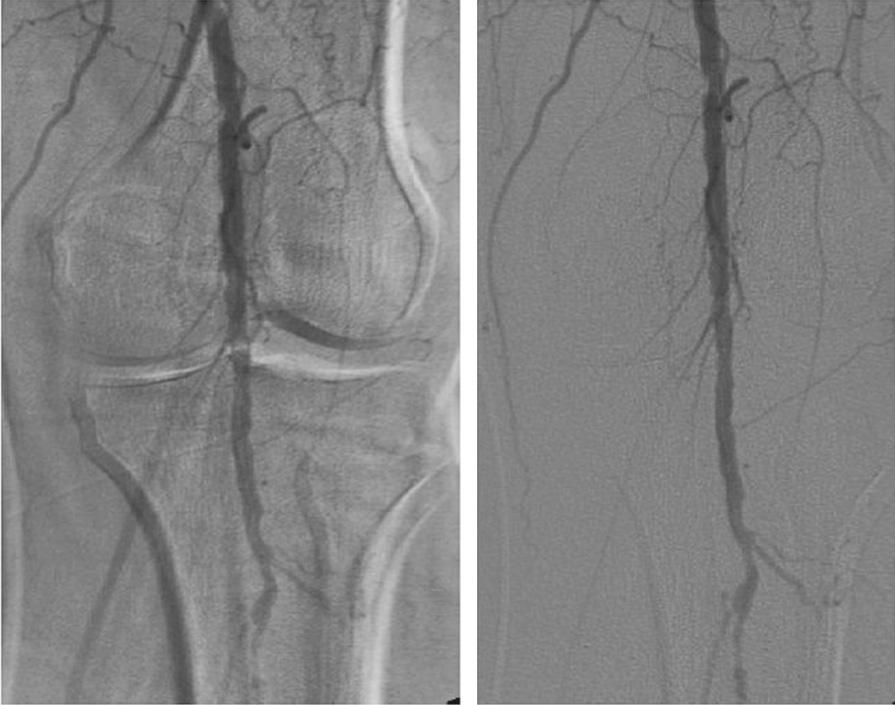
There are several important differences in imaging of peripheral vascular structures and coronary arteries. Peripheral angiography commonly uses a larger image intensifier field (14 inches [36 cm]) to encompass larger regions of interest. Digital (not film-based) angiography allows online display of acquired images as well as advanced processing techniques to enhance brightness, contrast, or shift of underlying bone structures to enhance the final image ( Fig. 74-1 ). Frequently, digital subtraction angiography is used. With this imaging method, a baseline background image, referred to as a mask, is obtained immediately before injection of contrast material to digitally subtract bone, calcifications, air, or soft tissues from the final image, leading to the best image quality with the most definition of vascular anatomy. Another advantage of digital subtraction angiography is that it can reduce the volume of contrast material and imaging acquisition time required.
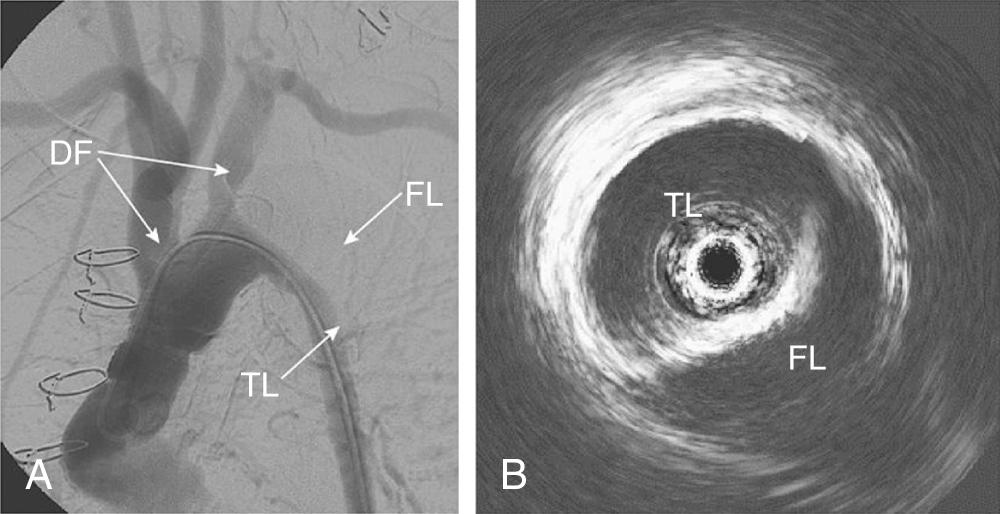
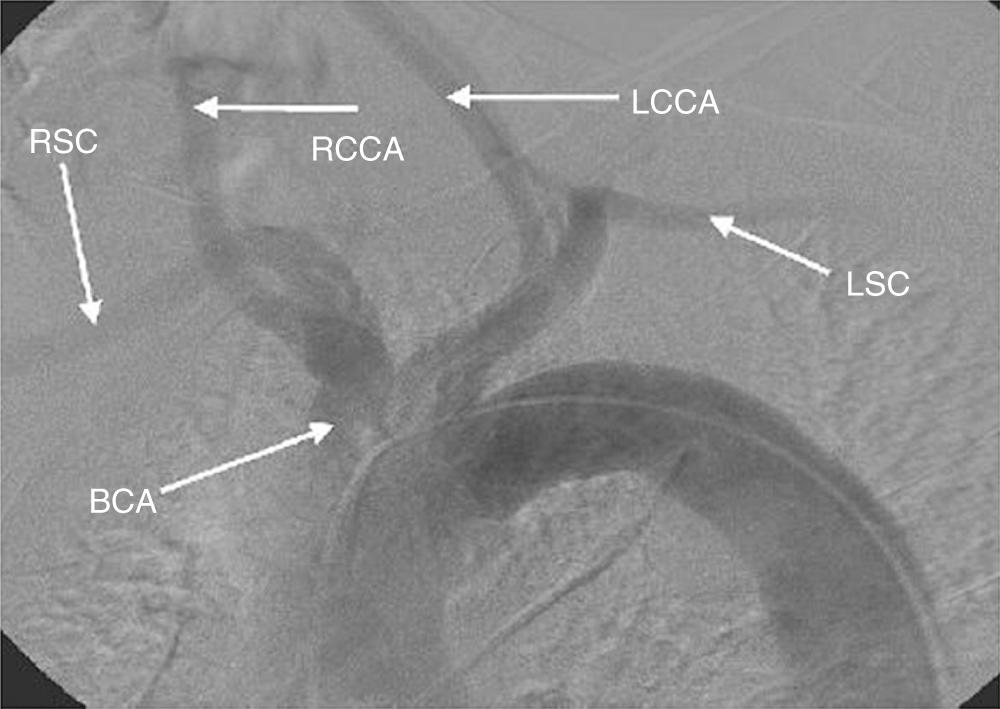
Thoracic aortography is used to define the anatomic relation of the aortic arch and the great vessels, to determine the diameter of the thoracic aorta, to obtain evidence of dissection ( Fig. 74-2 ), and to evaluate for trauma or other vascular injuries. The optimal view of the aortic arch is obtained in the left anterior oblique projection at 30 to 40 degrees oblique. The injection of 30 to 40 mL of contrast material at 20 to 30 mL/sec generally opacifies the vessels for adequate imaging. If digital subtraction angiography is used, the patient should be instructed to hold his or her breath to avoid artifacts caused by motion or breathing. The three principal vessels originating from the arch are (1) the brachiocephalic (innominate), leading ultimately to the right subclavian and right carotid arteries; (2) the left common carotid; and (3) the left subclavian artery ( Fig. 74-3 ). The most common normal variant of this anatomy is the so-called bovine arch, in which the left common carotid artery originates from the brachiocephalic trunk. This normal variant occurs in approximately 10% of patients.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here