Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
† Deceased.
In this chapter, we provide a brief overview of cardiac structure as it is relevant for the cardiac surgeon. We describe the heart as it is located in the body in its anatomic, or attitudinally correct, position. Whenever possible, however, we illustrate the cardiac components as they would be viewed by the surgeon during an operative procedure, whether the pictures were taken in the operating room or are of anatomic specimens. In some instances, information is best presented with the heart photographed in a nonsurgical orientation. When this occurs, it is clearly stated.
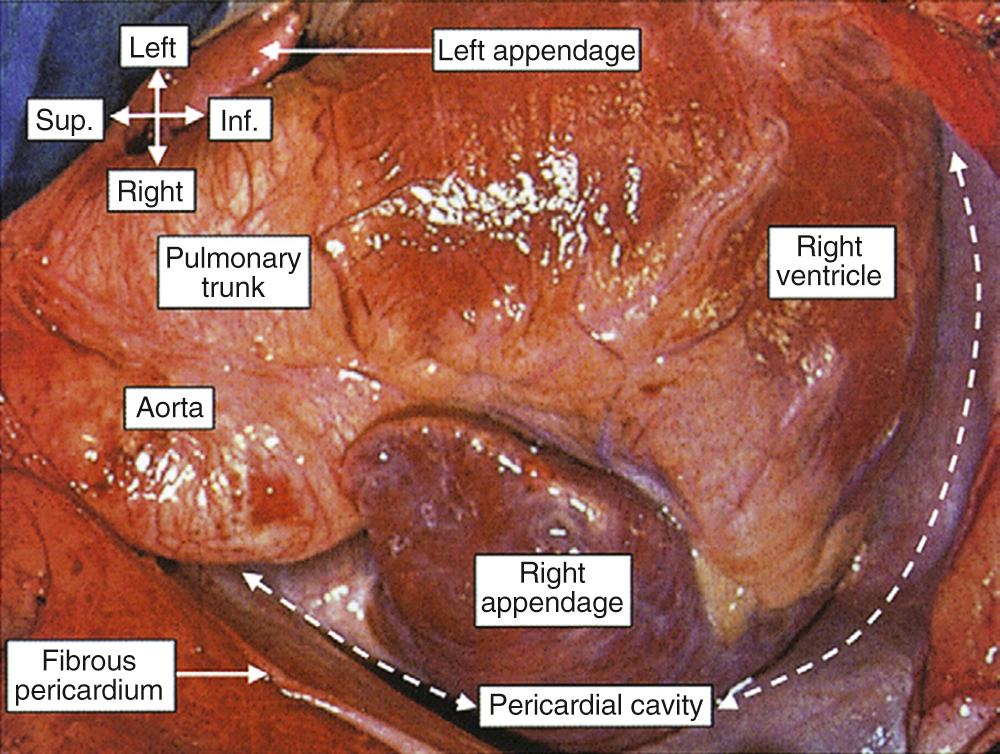
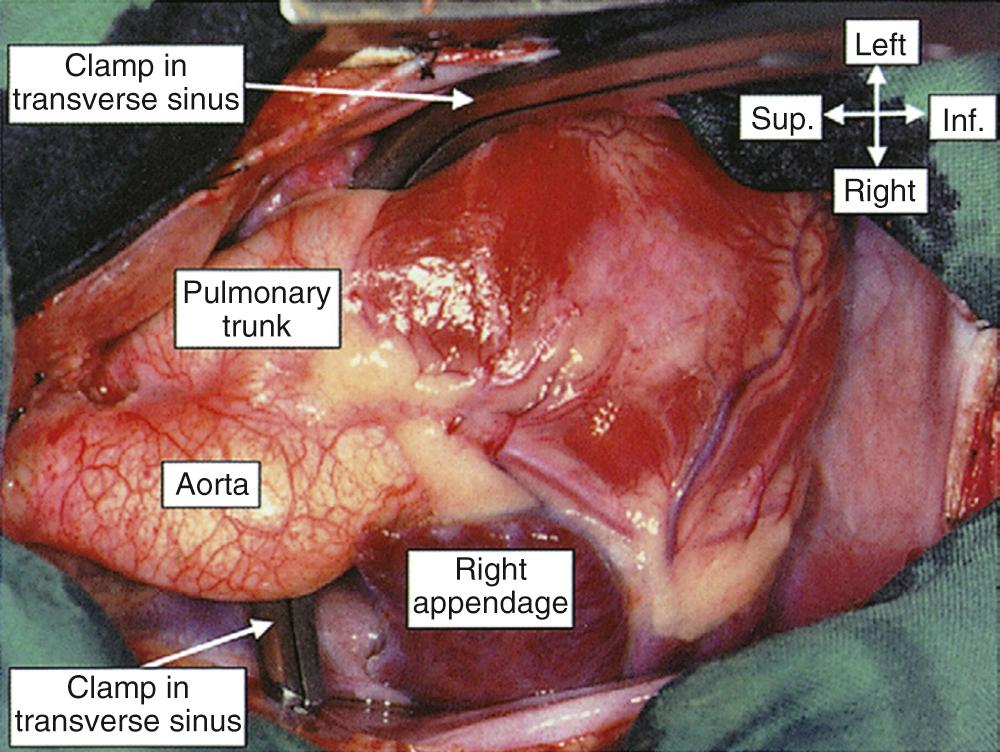
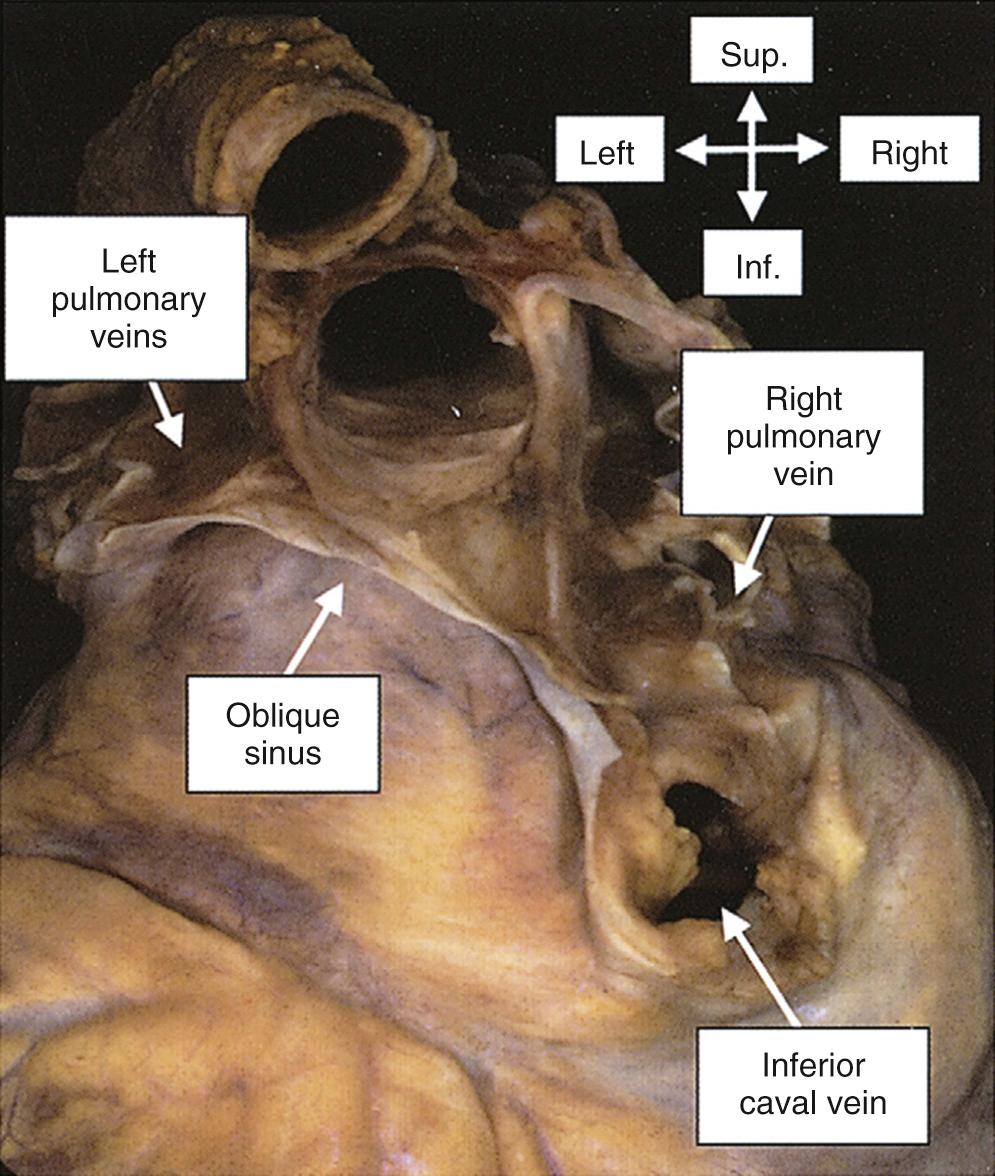
Regardless of the surgical approach, the surgeon who enters the mediastinum is confronted by the heart enclosed in its pericardial sac. The sac is freestanding around the atrial chambers and the ventricles, but it becomes adherent to the adventitial coverings of the great arteries and veins at their entrances to and exits from the heart, where these attachments close the pericardial cavity. The pericardial cavity is contained between the two layers of the serous pericardium, a thin-walled sac folded on itself within the fibrous cavity. The inner layer, or epicardium, is firmly attached to the myocardium, whereas the outer layer is adherent to the fibrous pericardium. The pericardial cavity, therefore, is the space between the inner lining of the fibrous pericardium and the surface of the heart ( Fig. 47-1 ). By virtue of the shape of the cardiac chambers and the great arteries, there are two recesses within this cavity that are lined by serous pericardium. The first is the transverse sinus, a horseshoe-shaped space behind the great arteries and in front of the atria ( Fig. 47-2 ). Laterally on each side, the ends of the transverse sinus are in free communication with the rest of the pericardial cavity. The second pericardial recess is the oblique sinus, a blind-ending cavity behind the left atrium ( Fig. 47-3 ).
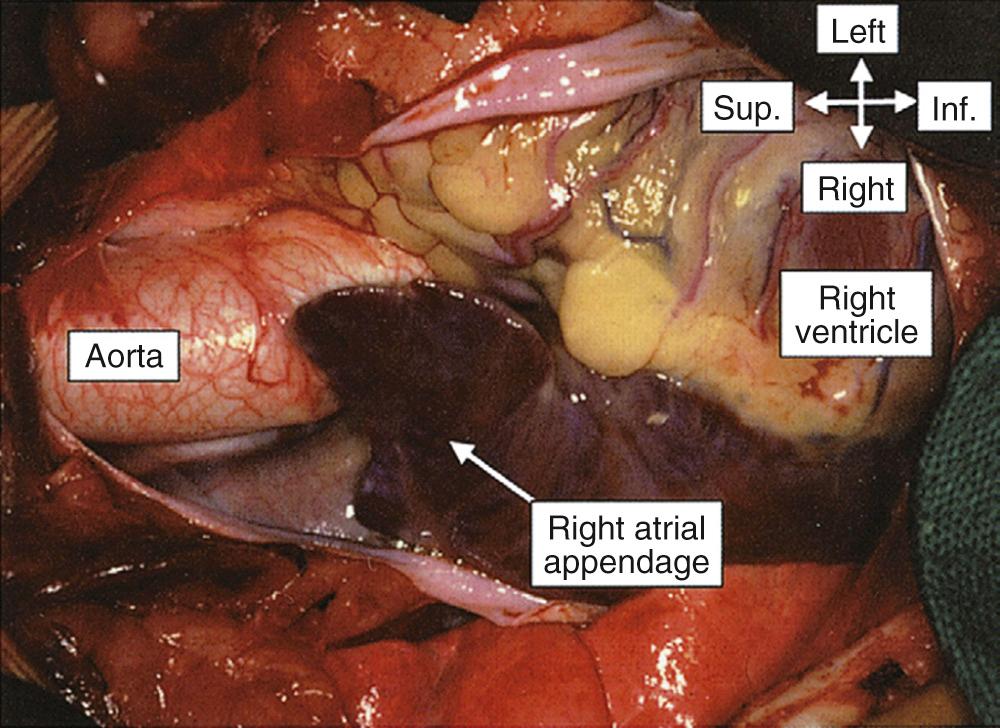
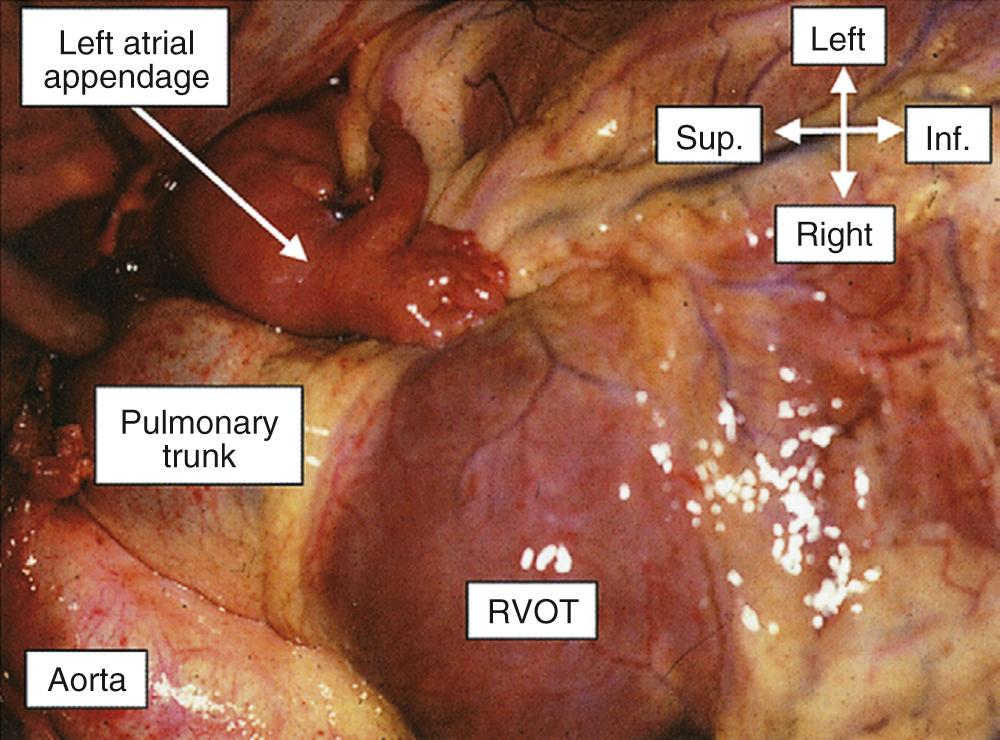
Most of the cardiac surface facing the surgeon is occupied by the so-called right heart, which in reality is anterior. Thus, the surgeon is confronted by the extensive appendage of the right atrium, receiving the superior caval vein at its superior border. To the left are the aorta and the pulmonary trunk, exiting from the base of the heart and extending in a superior direction, with the aortic root in an inferior and rightward position. When the aortic root is not in this “normal” relationship, the ventriculoarterial connections are almost always abnormal. The morphologically right appendage has a characteristic shape, being triangular and possessing a broad junction with its venous component ( Fig. 47-4 ). The morphologically left appendage might not be seen immediately. If searched for, it is found as a tubular, meandering structure at the left border of the pulmonary trunk ( Fig. 47-5 ), having a narrow junction with the rest of the atrium.
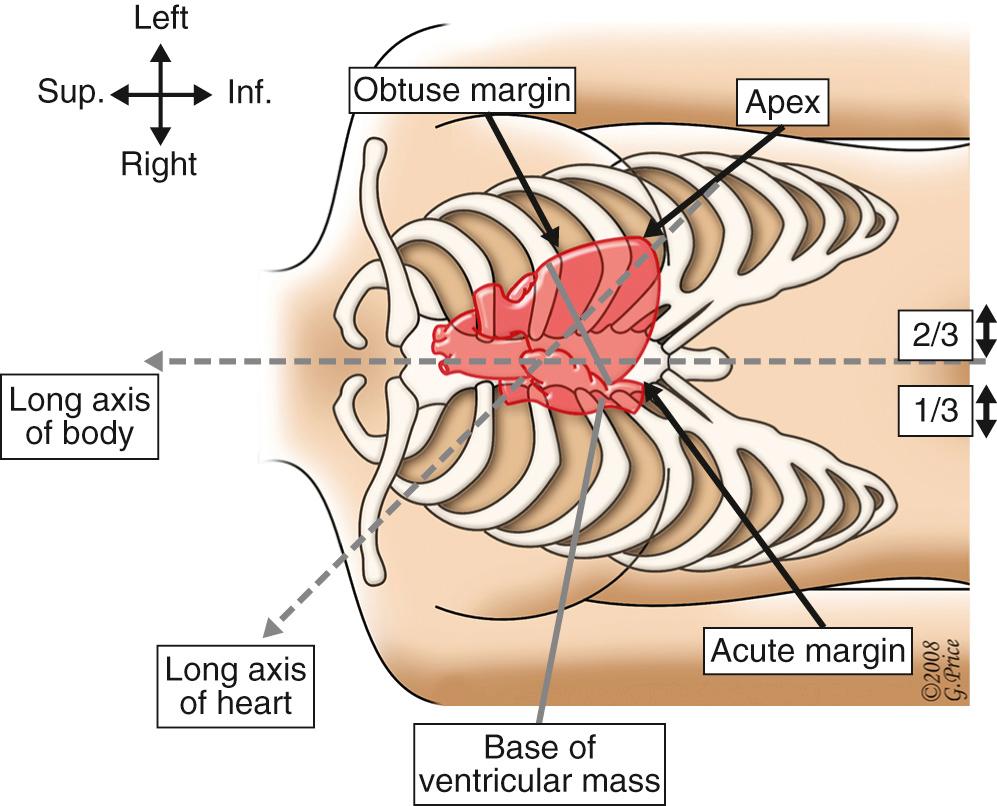
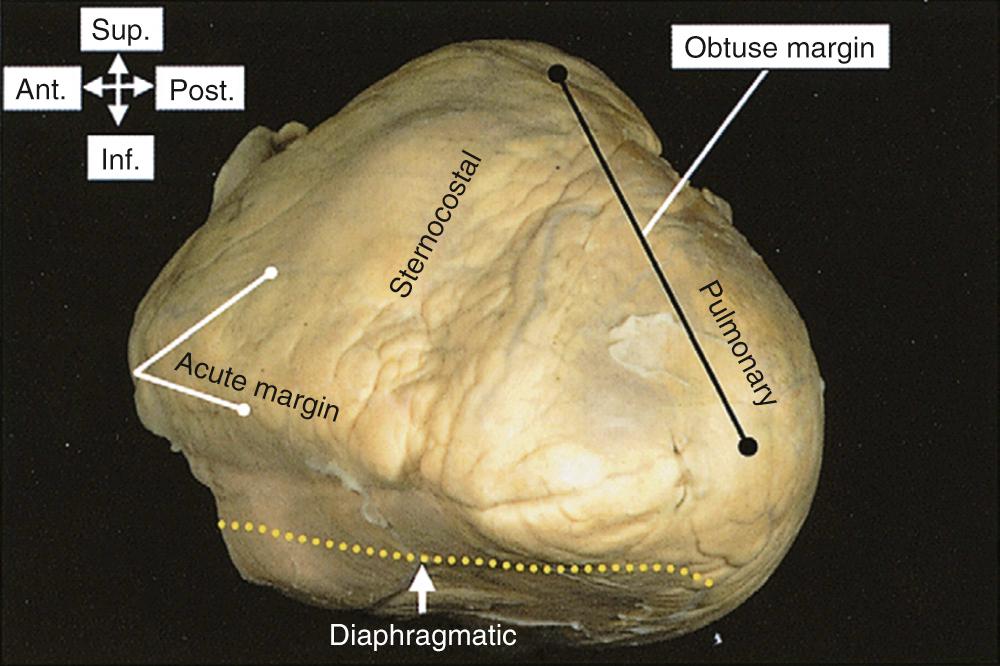
The ventricular mass then extends to the cardiac apex, which normally reaches into the left hemithorax. The overall cardiac silhouette is usually positioned with one third of its bulk to the right and two thirds to the left of the midline ( Fig. 47-6 ). An anomalous position of either the ventricular mass or the apex is highly suggestive of the presence of congenital cardiac malformations, although not always. In shape, the ventricular mass is a three-sided pyramid, having (1) diaphragmatic, (2) anterior or sternocostal, and (3) left or pulmonary surfaces. The margin between the first two surfaces is sharp; therefore, it is called the acute margin. The transition between the sternocostal and pulmonary surfaces is more gradual and rounded. For the surgeon, it is the pulmonary surface that is considered to be the obtuse margin, as it is irrigated by the obtuse marginal arteries ( Fig. 47-7 ). The greater part of the anterior surface of the ventricular mass is occupied by the morphologically right ventricle. Its left border is marked by the anterior interventricular, or descending, branch of the left coronary artery, and its right border is marked by the right coronary artery, which runs obliquely in the atrioventricular groove.
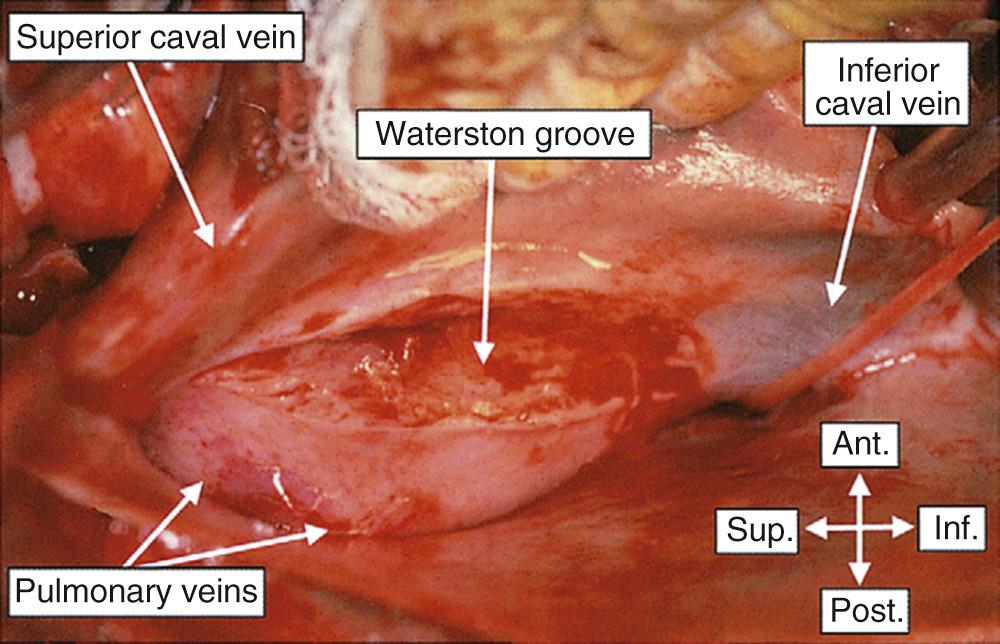
Appreciating the surface anatomy of the heart is helpful in determining the most appropriate site for an incision to gain access to a given cardiac chamber. For example, the relatively bloodless outlet portion of the right ventricle just beneath the origin of the pulmonary trunk affords ready access to the ventricular cavity. The important landmark for the right atrium is the terminal groove, or sulcus terminalis, which marks the border between the appendage and the venous component ( Fig. 47-8 ). The sinus node is typically located in this groove, usually laterally in the superior cavoatrial junction inferior to the crest of the appendage. Posterior and parallel to the terminal groove is a second, deeper groove between the right atrium and the right pulmonary veins. Dissections into this deep interatrial groove, also known as Waterston or Sondergaard groove, permit incisions to be made into the left atrium ( Fig. 47-9 ).
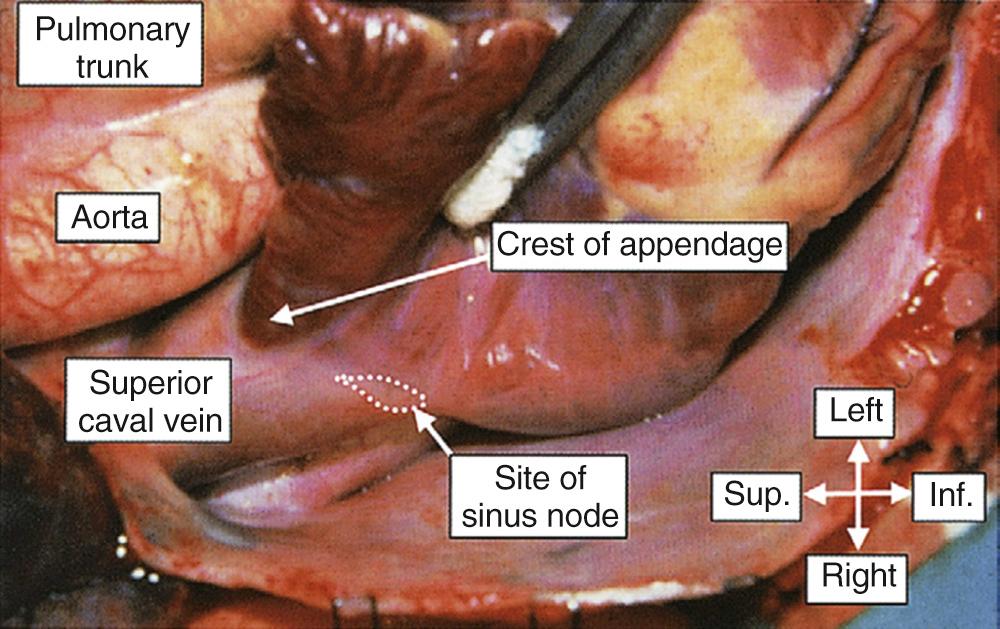
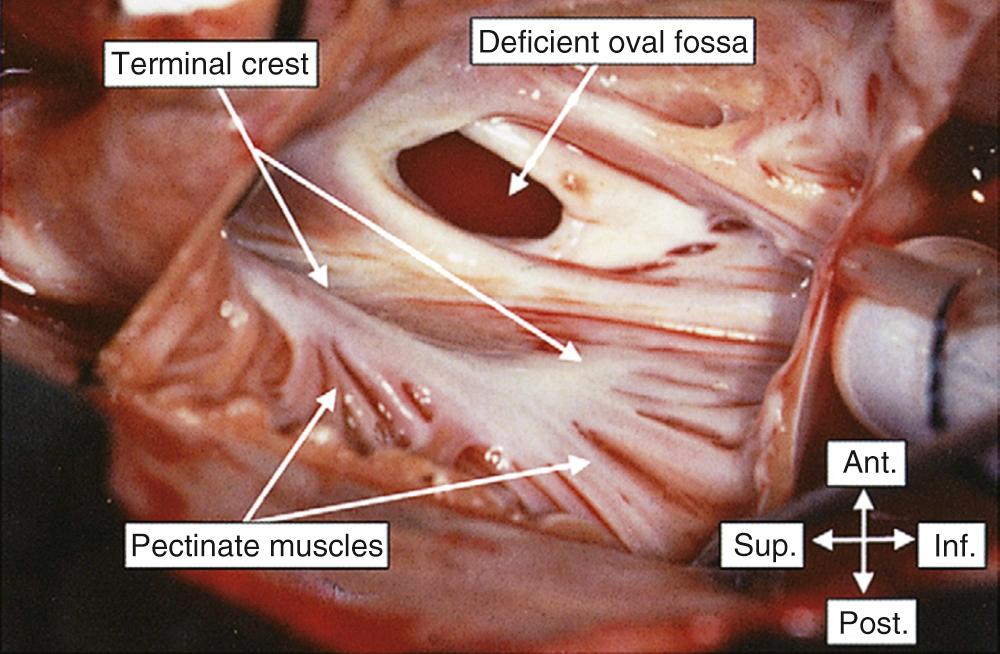
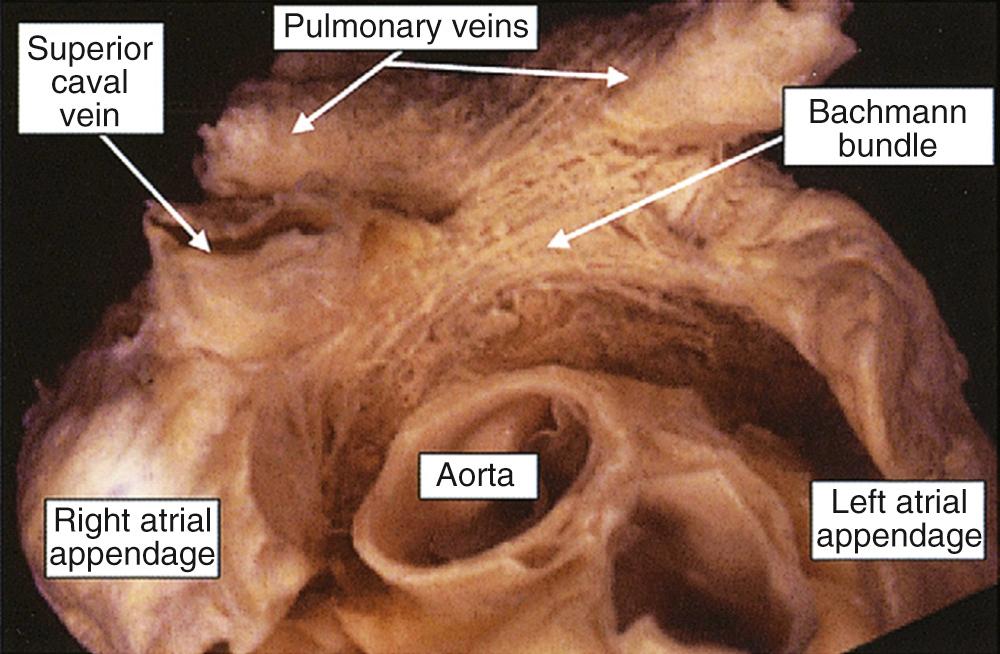
The right atrium has three components: the appendage, the venous sinus receiving the systemic venous return, and the vestibule. It is separated from the left atrium by the septum. As mentioned, the junction between the appendage and the venous sinus is marked externally by the prominent terminal groove. Internally, the groove corresponds with the position of the terminal crest (crista terminalis), which gives origin to the pectinate muscles of the appendage ( Fig. 47-10 ). Significantly, the pectinate muscles within the appendage encircle the full extent of the third component, the vestibule, which is the smooth muscle encircling the orifice of the tricuspid valve ( Fig. 47-11 ). This extensive array of pectinate muscles serves to identify an atrium as being morphologically right even when abnormally located, or when duplicated as seen in isomerism. Superiorly and anteriorly, the appendage terminates in a prominent crest that forms the summit of the terminal groove and continues in the transverse sinus behind the aorta across the interatrial groove as Bachmann bundle ( Fig. 47-12 ). The sinus node lies in the terminal groove in an immediately subepicardial position. It is a spindle-shaped structure that usually lies to the right of the crest—that is, lateral to the superior cavoatrial junction. In approximately one tenth of cases, the node extends across the crest into the interatrial groove, draping itself across the cavoatrial junction in horseshoe fashion. For the surgeon, the artery to the sinus node is also of significance. It is a branch of the right coronary artery in approximately 55% of individuals and a branch of the circumflex artery in the remainder. Regardless of its origin, it usually courses through the anterior interatrial groove toward the superior cavoatrial junction, frequently running within the atrial myocardium. Having reached the cavoatrial junction, the artery may cross the crest of the appendage, course retrocavally, or even divide to form an arterial circle around the junction.
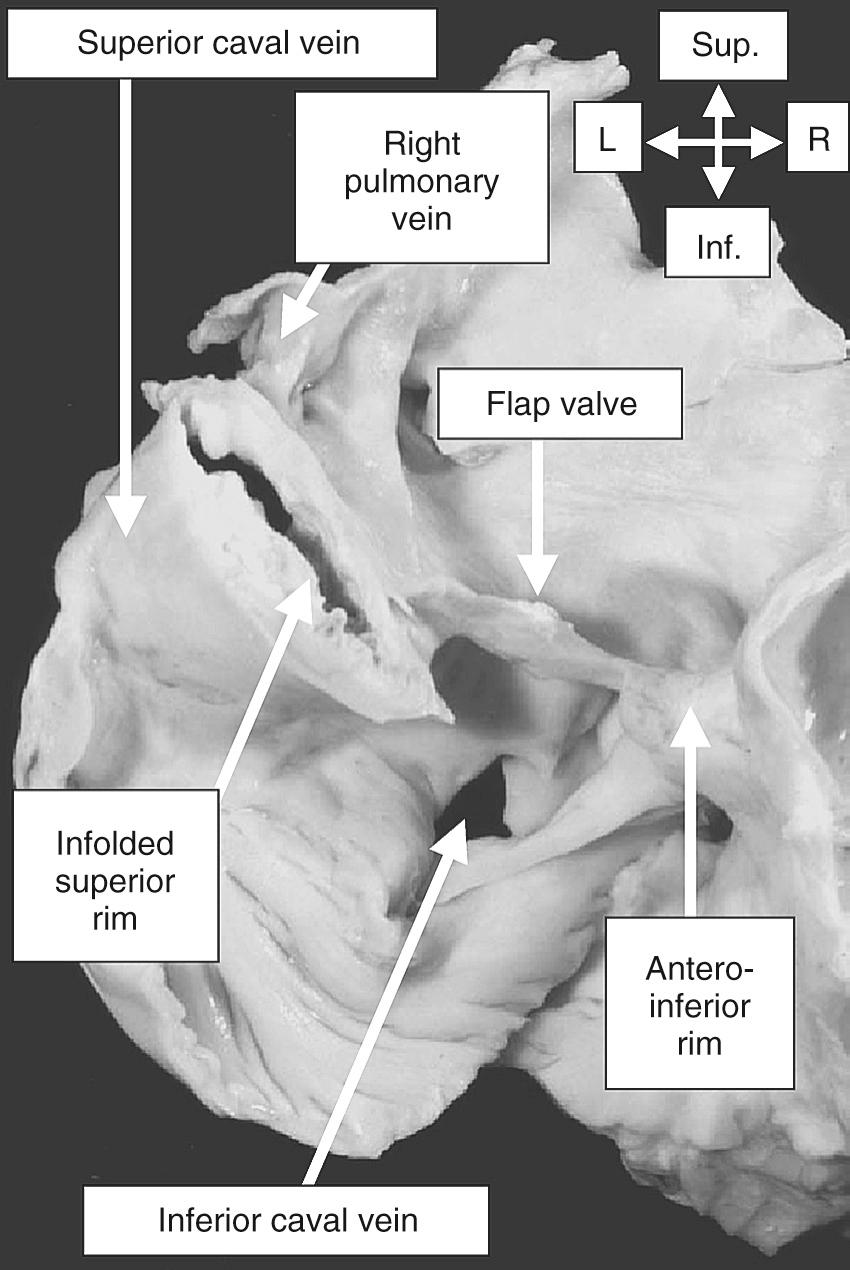
On first sight, when inspecting the internal morphology of the right atrium, there appears to be an extensive septal surface between the orifices of the caval veins and the orifice of the tricuspid valve. The apparent extent of this septum is spurious. The true septum between the right and left atrial chambers is formed by the floor of the oval fossa (derived from the fetal flap valve), and its adjacent anteroinferior muscular rim. The extensive superior rim, or the so-called septum secundum, is formed by a deep interatrial fold extending between the systemic and the pulmonary veins ( Fig. 47-13 ). The larger part of the anterior atrial wall is folded around the aortic root. That the margins of the true atrial septum are limited is of major surgical importance, as it is easy to pass outside the heart when attempting to gain access to the left atrium through a right atrial approach.
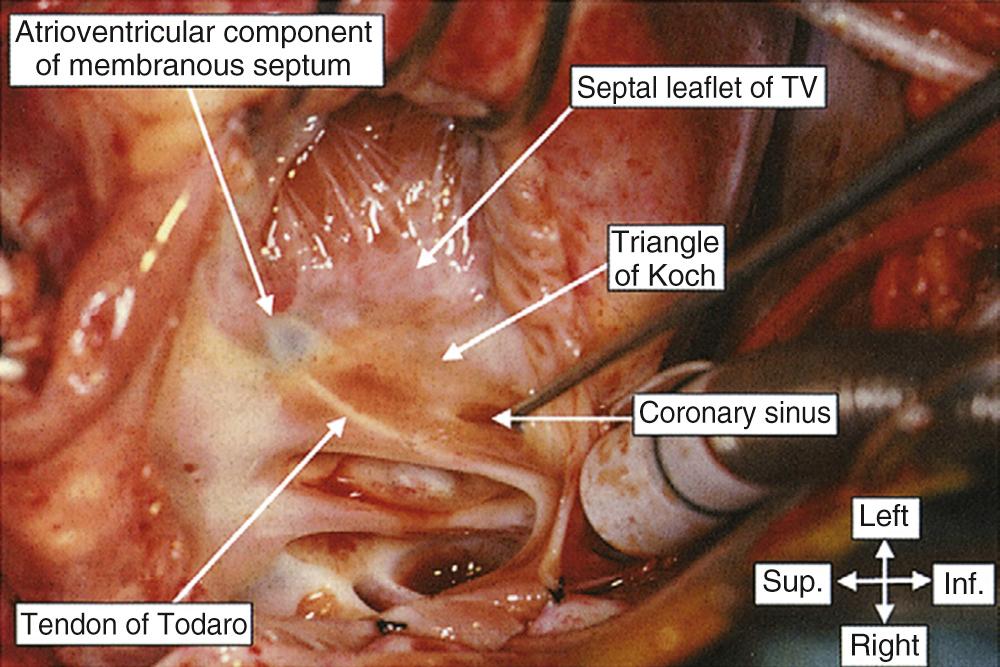
In addition to the position of the sinus node, and the extent of the atrial septum, the other major area of surgical significance in the right atrium is the site of the atrioventricular node. This is contained within the triangle of Koch ( Fig. 47-14 ). This important landmark is demarcated by the tendon of Todaro, the attachment of the septal leaflet of the tricuspid valve, and the orifice of the coronary sinus. The tendon of Todaro is a fibrous structure formed by the union of the eustachian and thebesian valves. The fibrous extension of these two valvar remnants buries itself in the tissue separating the oval fossa from the mouth of the coronary sinus, and it runs medially as the tendon of Todaro, which inserts into the central fibrous body. The entire atrial component of the axis of atrioventricular conduction tissues is contained within the confines of the triangle of Koch. If, in hearts with normal segmental connections, this area is scrupulously avoided during surgical procedures, the atrioventricular conduction tissues will not be damaged. The node itself, located in the smooth atrial musculature of the triangle, is some distance above the hinge point of the septal leaflet of the tricuspid valve. The atrioventricular bundle, however, penetrates more or less directly at the apex of the triangle of Koch.
Much has been written in recent years about the role of “specialized” pathways of tissue in conduction of the sinus impulse to the atrioventricular node. It can now be stated with certainty that there are no insulated or isolated tracts of specialized conduction tissue extending between the nodes that can be avoided surgically, as is possible with the penetrating and branching atrioventricular bundles. The major muscle bundles of the atrial chambers serve as preferential pathways of conduction, but the course of these preferential pathways is dictated by the overall geometry of the chambers. Ideally, prominent muscle bundles, such as the terminal crest or the superior rim of the oval fossa, should be preserved during atrial surgery. But even if they cannot be preserved, the surgeon can be sure that internodal conduction will continue as long as some strand of atrial myocardium connects the nodes, provided that the arterial supply to the nodes, or the nodes themselves, are not traumatized. The key to avoidance of postoperative atrial arrhythmias, therefore, is the fastidious preservation of the sinus and atrioventricular nodes and their arteries.
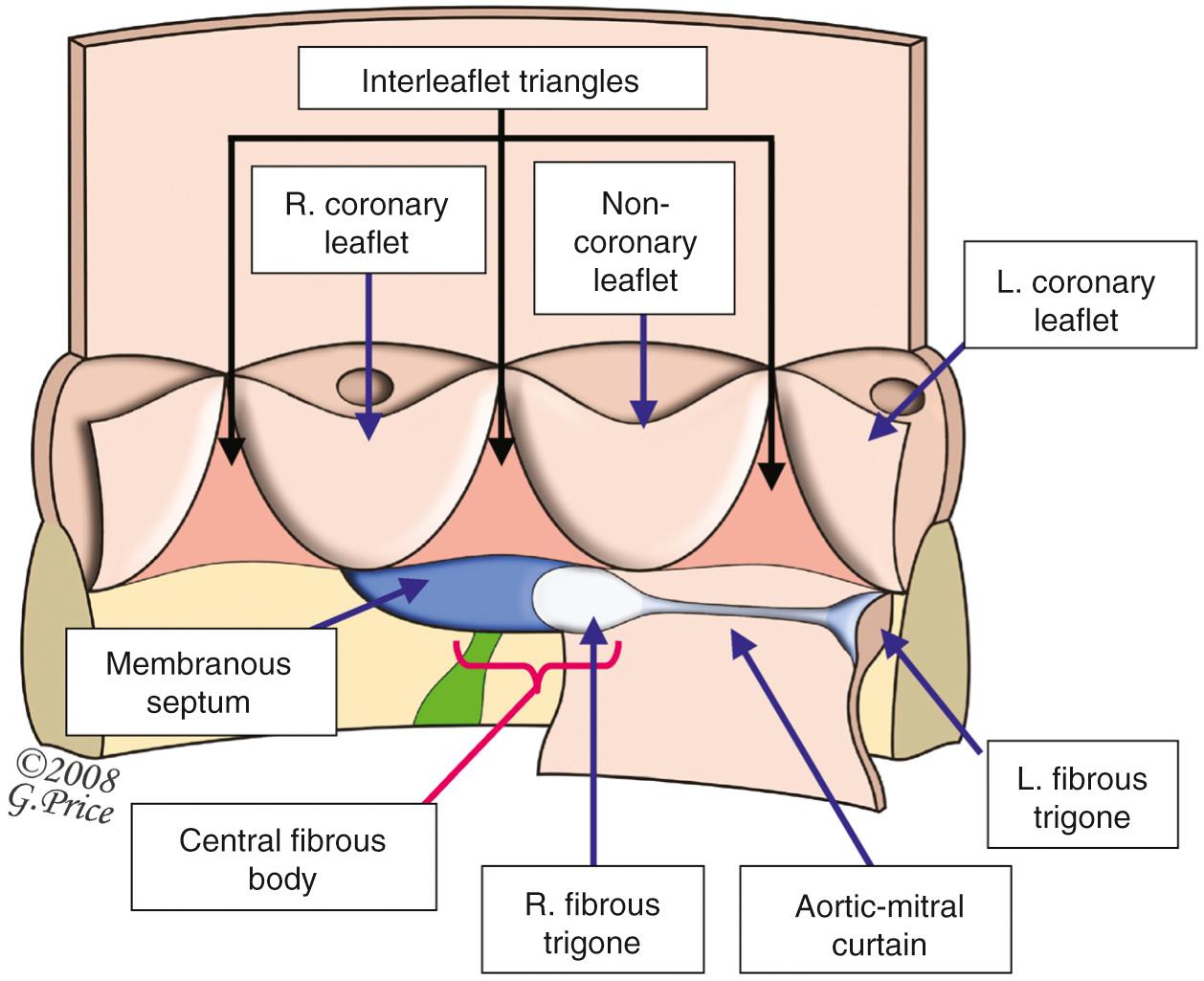
The central fibrous body touches on three of the four cardiac chambers, but it is in the right atrium that it becomes first, and perhaps most clearly, evident to the surgeon (see Fig. 47-14 ). Rather than being a specific body, it is better conceptualized as an area in the heart where the membranous septum and the leaflets of the atrioventricular and aortic valves join in fibrous continuity. When viewed from the left heart ( Fig. 47-15 ), it is possible to assess its proximity to the aortic and mitral valves and to the left bundle branch of the conduction axis. Because of this intimate relationship to so many important structures in the heart, the central fibrous body acts as an anatomic focal point for the cardiac surgeon.
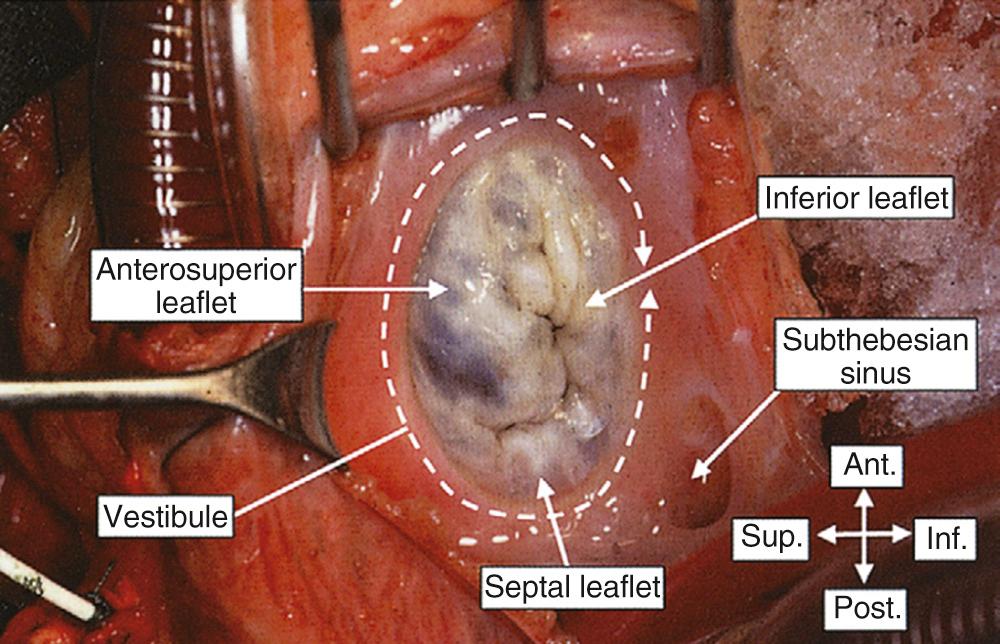
The vestibule of the atrium, surrounding the orifice of the tricuspid valve, is continuous with both the venous component and the appendage of the right atrium. Its anterosuperior part overlies the anteroseptal commissure of the tricuspid valve and continues along the supraventricular crest of the right ventricle. The posteroinferior component extends beneath the orifice of the coronary sinus, where there is usually an extensive trabeculated diverticulum found behind the sinus, the so-called posteustachian sinus of Keith.
Because of its position, only the appendage of the left atrium may be immediately evident to a surgeon upon exposing the heart. Like the right atrium, the left atrium has a venous component, an appendage, and a vestibule, and it is separated from its partner by the septum. In addition, the left atrium possesses a well-formed body, forming the dome of the atrium when the veins are connected anomalously, as in totally anomalous pulmonary venous connection. Unlike that of the right atrium, however, the venous component of the left atrium is considerably larger than the appendage, and the narrow junction between these two parts is not marked by either a terminal groove or a crest ( Fig. 47-16 ). The pectinate muscles are confined within the appendage, and again, unlike on the right side, they do not extend around the vestibule. This difference in the extent of the pectinate muscles always permits the morphologically right appendage to be distinguished from the morphologically left structure. Because of its posterior position and its firm anchorage by the four pulmonary veins, direct access to the left atrium can be difficult; therefore, surgeons must use their knowledge of anatomy to gain the best exposure of the cavity. Probably the most popular route is an incision made just posterior to the interatrial groove. As described, this extensive infolding between the right pulmonary veins and the systemic veins produces the superior rim of the oval fossa. A posteriorly directed incision along this groove takes the surgeon directly into the left atrium. Because the infolding of the interatrial groove also forms the superior border of the oval fossa, much the same access can be gained by approaching through the right atrium and incising just superiorly within the fossa. A further approach to the left atrium is the so-called superior approach, incising directly through the roof.
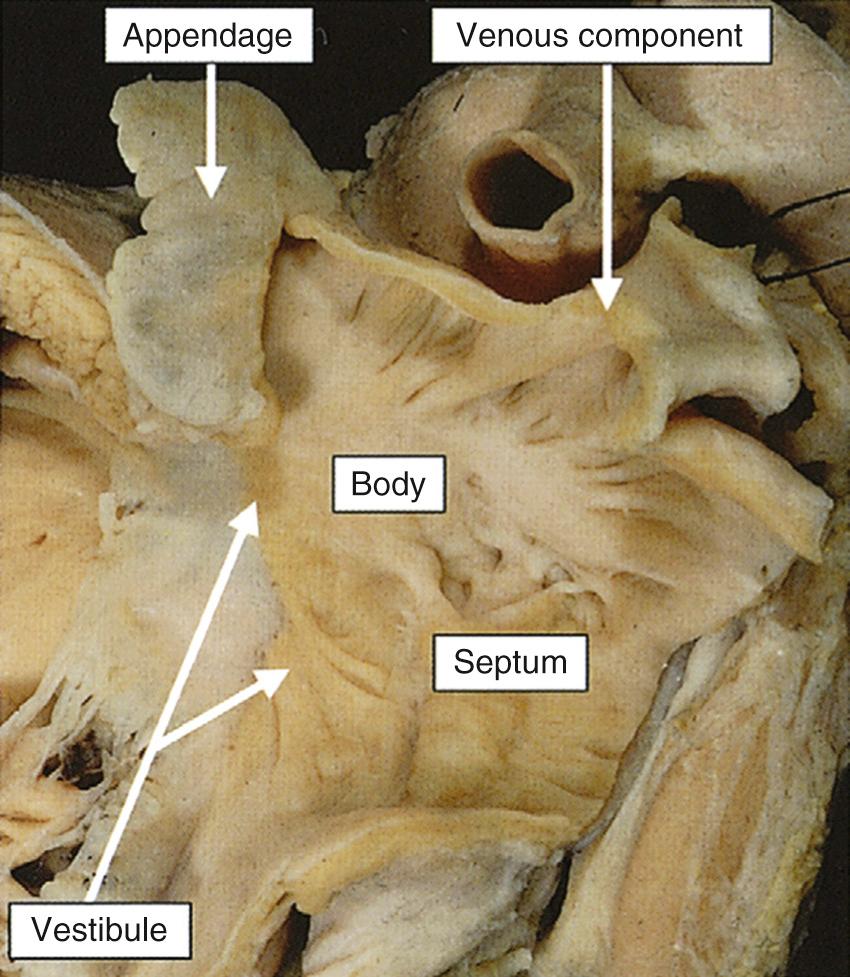
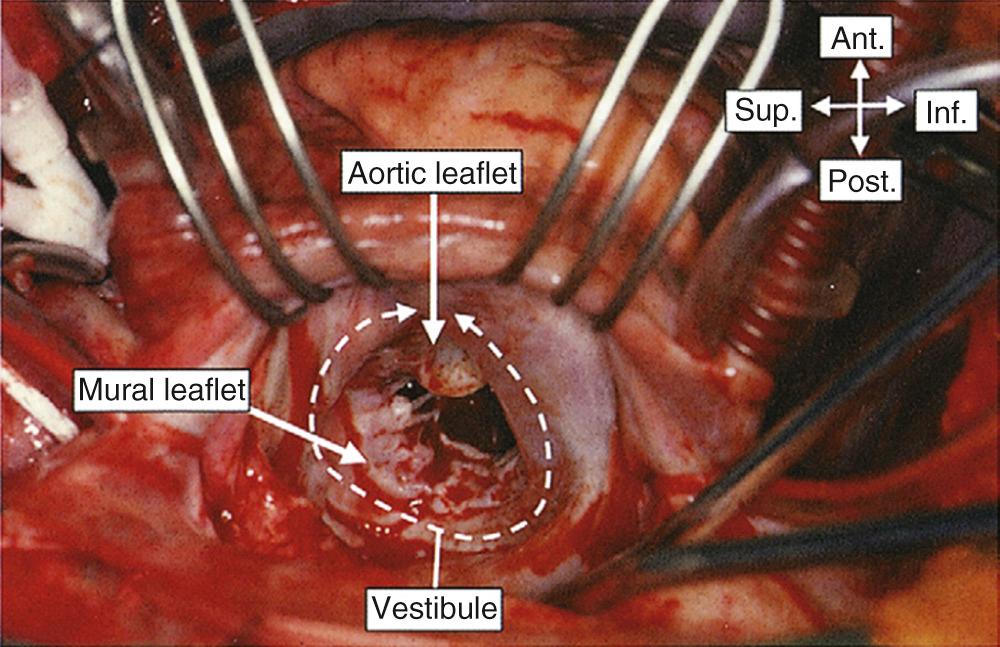
Once access is gained to the left atrium, the small size of the opening of the appendage is apparent, lying to the left of the mitral orifice as viewed by the surgeon. The greater part of the pulmonary venous atrium is usually located inferiorly, away from the operative field, and the vestibule of the mitral orifice dominates the picture ( Fig. 47-17 ). The septal aspect is anterior, exhibiting the typically roughened flap-valve aspect of its left side (see Fig. 47-16 ). The large sweep of tissue between the flap-valve of the septum and the opening of the appendage is the internal aspect of the deep anterior interatrial groove.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here