Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The management of hepatic trauma patients has evolved significantly during the last three decades and is now based on well-defined treatment algorithms. This has highlighted the need for an accurate classification system as a basis for the clinical decision-making process. Fundamental to the development of these classification schemes and the subsequent treatment algorithms based on them is the widespread availability of rapid acquisition computed tomography (CT) imaging in most major trauma centers. This has also led to a diminution in the role of diagnostic peritoneal lavage in the management of the trauma patient. Diagnostic peritoneal lavage has multiple limitations: lack of specificity regarding the source of bleeding; high sensitivity to detection of small quantities of blood, leading to nontherapeutic laparotomy; and inaccuracy for retroperitoneal injuries. Diagnostic peritoneal lavage fails most importantly in its ability to identify the location and extent of intra-abdominal organ injury. Diagnostic peritoneal lavage is valuable mainly in patients in whom ultrasonography or CT scanning is inappropriate or unavailable.
Previous attempts to categorize hepatic injury were mostly anatomic in design and did not incorporate the mechanism of injury or physiologic changes associated with more severe injuries. In 1987, the Organ Injury Scaling Committee of the American Association for the Surgery of Trauma was organized for the purpose of devising injury severity scales for individual organs. These injury severity scales incorporated etiology, anatomy, and extent of injury and correlated it with subsequent clinical management and outcome. The most recently revised clinical classification is listed in Table 58.1 . It has been demonstrated that the CT grade of hepatic injury is not predictive of the need for surgery and that the majority of injuries can be safely managed nonoperatively. The hemodynamic status of the patient may be the most important predictor of injury severity; however, patients with higher-grade injuries (IV or V) are more likely to be unstable and to require surgery, and increasing organ injury severity scale grade in patients with isolated hepatic injuries is associated with increasing mortality. In contrast, patients who are stable may be managed conservatively with close observation in intensive care units. , , Mechanism of injury, radiologic classification, and clinical assessment of hemodynamic stability must all be correlated by the trauma surgeon to guide management decisions.
| Grade | Injury | |
|---|---|---|
| I | Hematoma | Subcapsular, <10% surface area |
| Laceration | Capsular tear, <1 cm parenchymal depth | |
| II | Hematoma | Subcapsular, 10%–50% surface area Intraparenchymal, <10 cm diameter |
| Laceration | 1–3 cm parenchymal depth, <10 cm in length | |
| III | Hematoma | Subcapsular, >50% surface area or expanding; ruptured subcapsular or parenchymal hematoma Intraparenchymal hematoma >10 cm or expanding |
| Laceration | Parenchymal fracture >3 cm deep | |
| IV | Laceration | Parenchymal disruption involving 25%–75% of hepatic lobe or 1–3 Couinaud segments within a single lobe |
| V | Laceration | Parenchymal disruption involving >75% of hepatic lobe or >3 Couinaud segments within a single lobe |
| Vascular | Juxtahepatic venous injuries (i.e., retrohepatic vena cava/central major hepatic veins) | |
| VI | Vascular | Hepatic avulsion |
Approximately 1% to 8% of patients who sustain blunt abdominal trauma have a liver injury. Severe compressive trauma to the liver from a steering wheel injury or direct blow can produce satellite fractures that often involve an entire lobe. Rapid deceleration in motor vehicle accidents produces shearing forces that cause different degrees of parenchymal tears. The hepatic lobes may be torn from each other, or the tears may involve the supporting ligaments, hepatic veins, and inferior vena cava. The most frequent site of hepatic injury is the posterior segment of the right lobe of the liver because of its size and proximity to the ribs and spine. Although they are less common, left lobe injuries are more often associated with retroperitoneal injuries (duodenum and pancreas) and transverse colon injuries. , There is a high incidence of associated extrahepatic injury, including splenic rupture, head injuries, rib fractures, facial fractures, and pelvic fractures.
Major hepatic venous injuries occur in 13% of patients with liver trauma. These are most often a result of blunt trauma. They include, in decreasing order of frequency, right hepatic vein avulsion from the inferior vena cava, upper branch right hepatic vein avulsion, avulsion of accessory veins, avulsion of the left hepatic vein, and avulsion of the middle hepatic vein. The right hepatic vein is at greater risk for sudden acceleration-deceleration injury because it has a relatively long extrahepatic segment before it enters the inferior vena cava. The course is shorter for the middle and left hepatic veins, which usually merge to form a common channel and thus are less frequently injured. , Venous injuries can be suggested by multiple lacerations around the inferior vena cava or porta hepatis. , It is important to identify these findings because they may help prepare the surgeons to expect significant bleeding when the liver is lifted off the inferior vena cava. Multiplanar CT reconstruction and three-dimensional rendering can be helpful in the assessment of vascular involvement, especially the portal vein, hepatic veins, and retrohepatic vena cava. Injuries of the bare area of the liver may not demonstrate peritoneal signs or findings on diagnostic peritoneal lavage or screening sonography for hemoperitoneum but may show retroperitoneal blood on CT examination.
Penetrating wounds are most commonly caused by stabbing, gunshot, or shotgun injury. , Knife stabbings usually cause superficial lacerations, whereas high-velocity projectiles generally cause injury from capsule to capsule, with massive parenchymal damage.
The liver is subject to a number of iatrogenic misadventures that may be caused by any of the various needles, wires, cannulas, and catheters placed by gastroenterologists and interventional radiologists. The liver can also be damaged by external cardiac compression during the course of resuscitation and by inappropriately low insertion of a chest tube.
Diagnostic and interventional procedures can produce a tear of the liver capsule, subcapsular hematoma, bile leak, arteriovenous fistula, pseudoaneurysm, arteriobiliary or venobiliary fistula, hepatic hematoma, hemoperitoneum, and biloma. The prevalence of this problem was well documented in one study in which intrahepatic (77%) and subcapsular (23%) hematomas were found sonographically in 23% of asymptomatic patients evaluated after liver biopsy.
Hepatic rupture and hemorrhage can occur in eclamptic or preeclamptic women during the third trimester due to h emolysis, e levated l iver enzymes, and l ow p latelets, the HELLP syndrome. The maternal mortality rate approaches 60% with hepatic rupture. Because surgery is difficult in these friable livers, hepatic artery transcatheter embolization offers a therapeutic alternative. One report showed good results with absorbable gelatin foam (Gelfoam) embolization in four eclamptic patients. , Bleeding from the liver may also immediately follow delivery in noneclamptic women.
Spontaneous hemorrhage can occur in patients who have sickle cell anemia, peliosis, hepatomas, hepatic adenoma, coagulopathies, B-cell lymphoma, metastases, organophosphate toxicity, or collagen vascular disease and in patients who receive long-term hemodialysis.
Imaging can make a major contribution to the management of trauma patients who are hemodynamically stable and to the postoperative assessment of these patients. , , ,
Multidetector computed tomography (MDCT) is the imaging technique of choice for hepatic trauma and has had an enormous impact on the detection and management of liver injuries. , , , ,
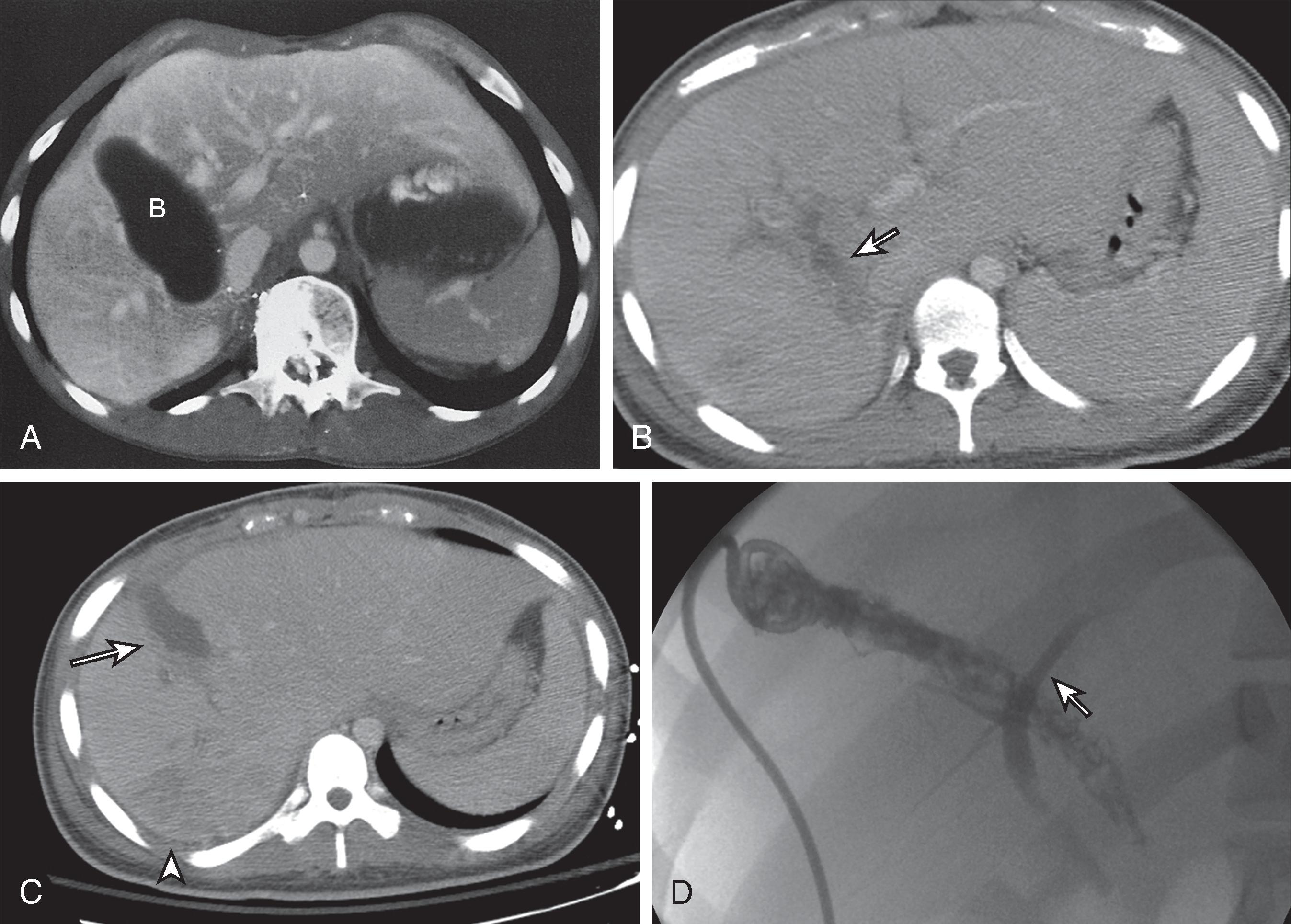
It can reliably diagnose and stage significant hepatic and extrahepatic injuries, document interval healing of hepatic injuries, and diagnose early and delayed complications. It can also detect associated and unsuspected injuries to other organs ( Fig. 58.1 ). Patients who are hemodynamically unstable require immediate surgery; surgical delay secondary to imaging can be fatal. Hemodynamically stable patients can be scanned in a matter of seconds, with better resolution and with multiplanar imaging capabilities, given our current CT technology.
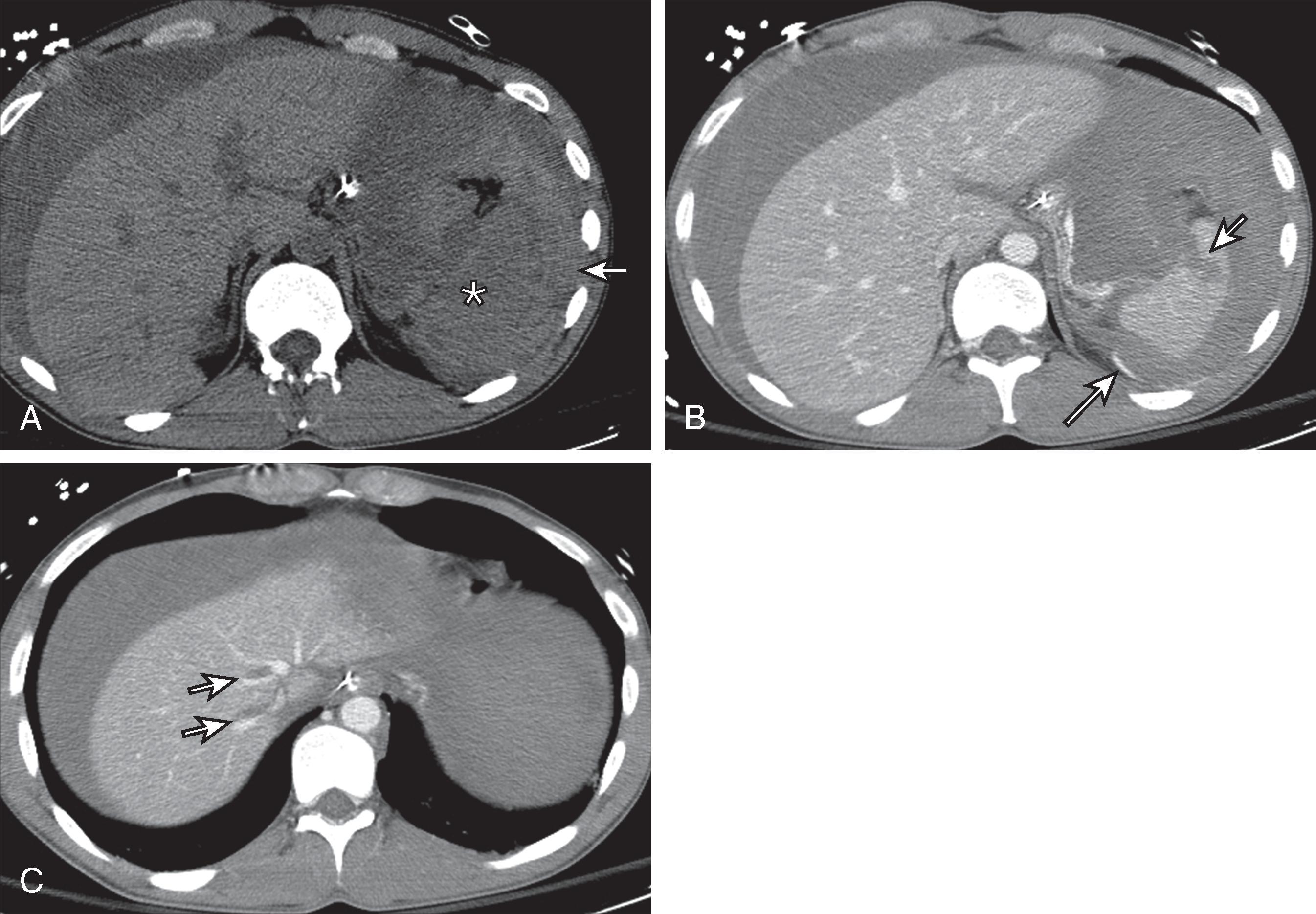
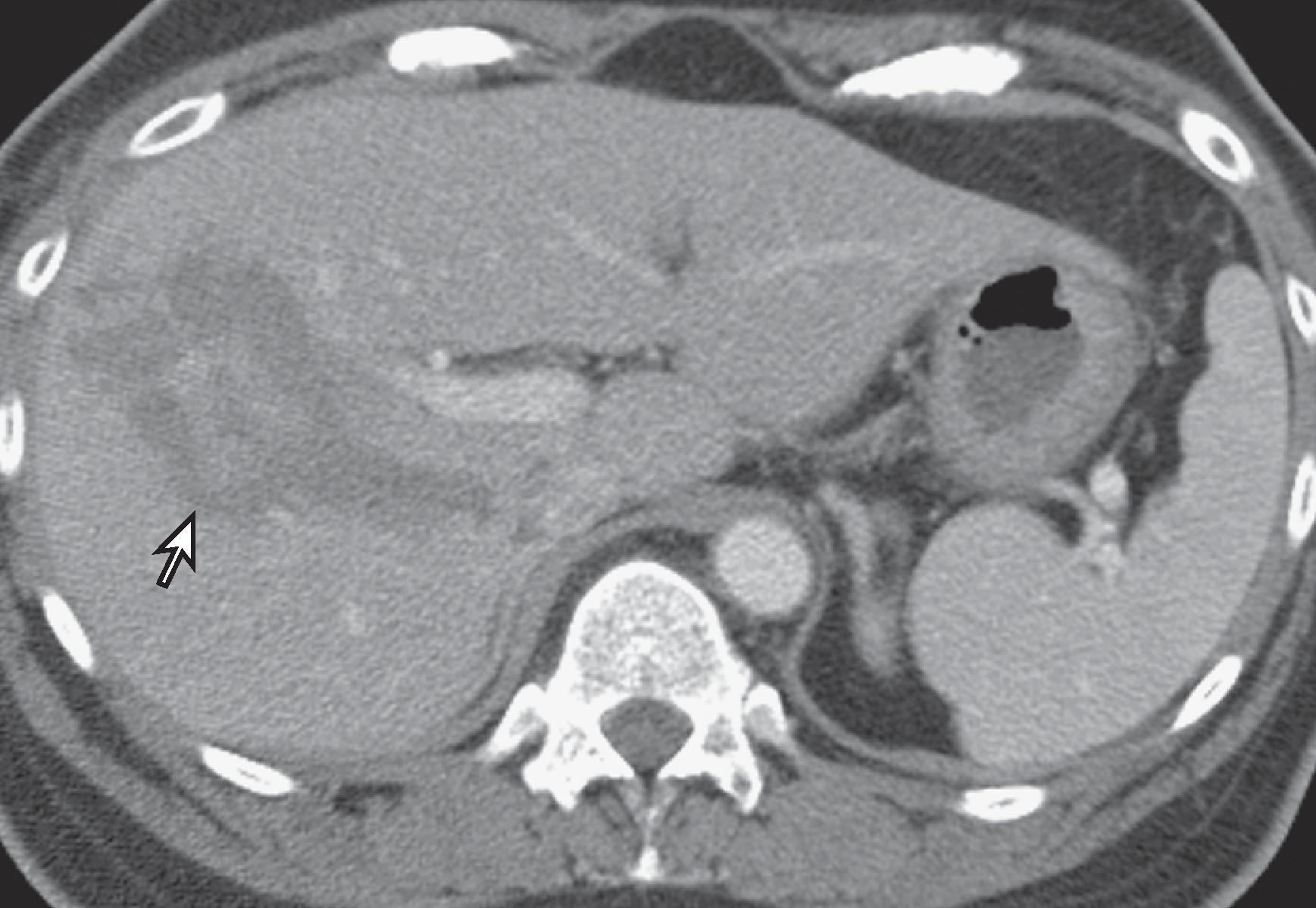
With any type of abdominal trauma, the first finding that should be evaluated is the presence or absence of blood, either parenchymal or intraperitoneal (hemoperitoneum). Immediately after injury, hematomas on noncontrast scans are hyperdense relative to normal hepatic parenchyma ( Fig. 58.2 ). After intravenous administration of contrast medium, unclotted blood is usually hypodense compared with enhancing normal parenchyma but still usually has an attenuation (20–40 HU) greater than that of simple fluid (0–20 HU).

Active hemorrhage is identified as extravasation of contrast material on contrast-enhanced CT. The attenuation values of extravasated contrast material (155 HU, mean value) and hematoma (54 HU, mean value) help distinguish active bleeding from clotted blood. , If the liver is involved by focal or diffuse fatty infiltration, a common finding in intoxicated drivers, parenchymal hematomas may appear isodense on contrast-enhanced examinations but can usually be distinguished with narrow CT window settings. In addition, the attenuation and the distribution of fluid can serve as a clue to the site of injury. This phenomenon has been termed the sentinel clot sign. The sentinel clot is the highest-density blood collection seen and usually lies adjacent to the injured organ ( Fig. 58.3 ). The evaluation of hepatic trauma should also search for other fluid collections, such as bile, as seen in bile leaks and bilomas, which have low attenuation because of their high cholesterol content.
In interpreting CT scans in patients with hepatic trauma, it is important to describe the anatomic site and extent of injury (superficial, deep, lobar, segmental, perihilar), the complexity of the lesion (simple or stellate laceration), and the type of hepatic injury (parenchymal laceration or subcapsular hematoma). , , ,
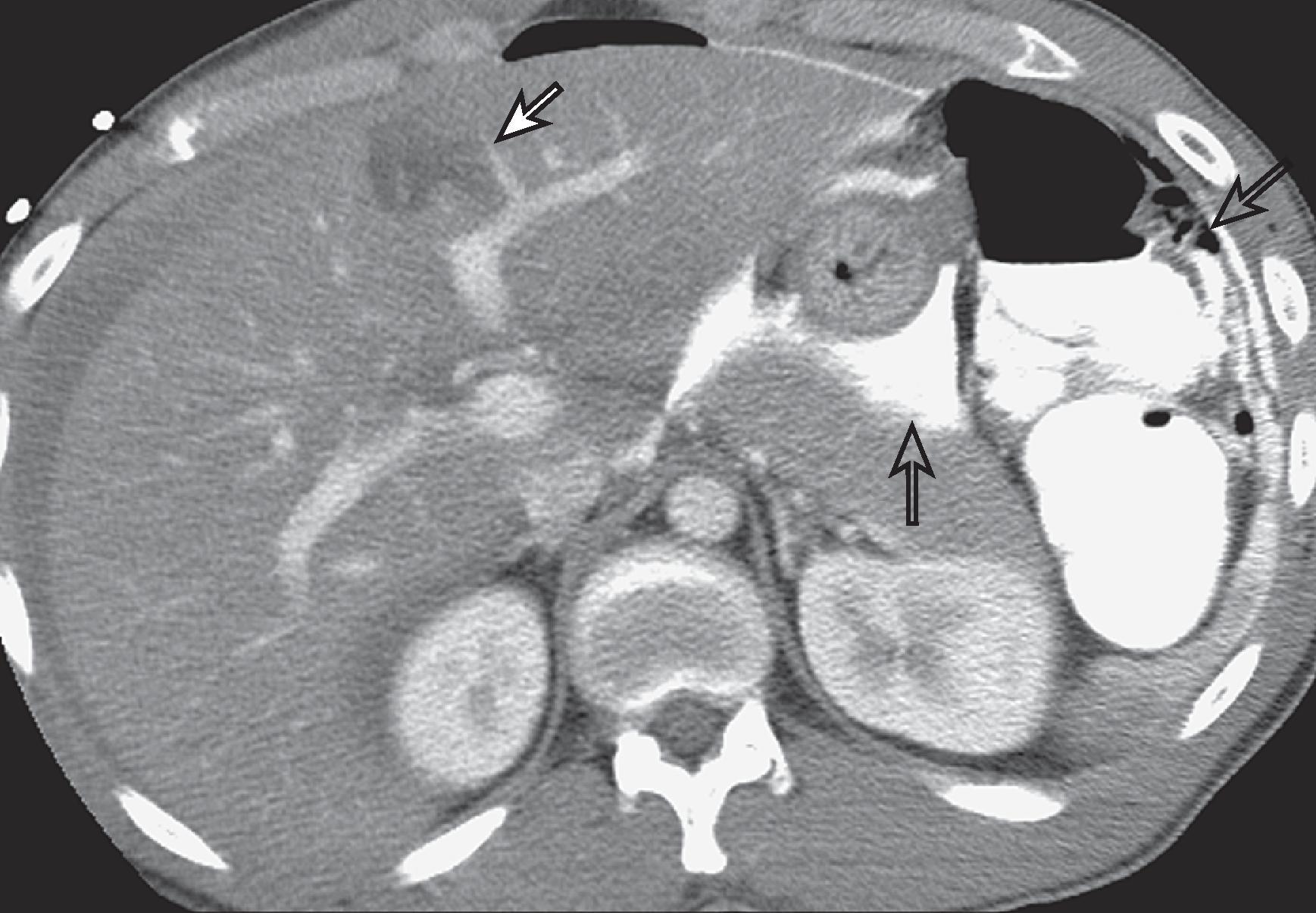
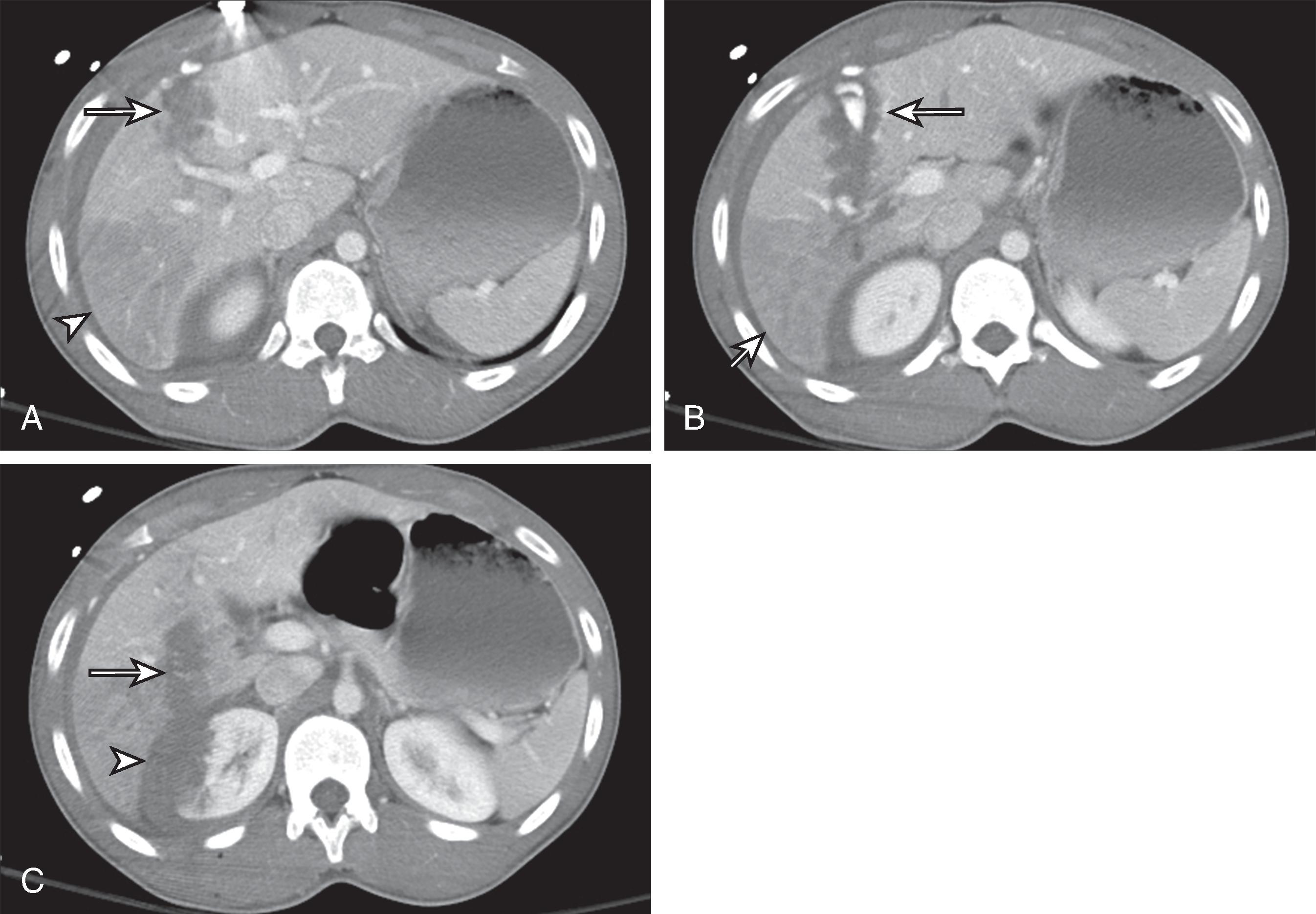
The major CT findings in blunt hepatic injuries are lacerations, subcapsular and parenchymal hematomas, active hemorrhage, and juxtahepatic venous injuries. Lacerations are the most common injury and appear as branching or linear low-attenuation areas. Lacerations can be classified into superficial (<3 cm from the liver surface) and deep (>3 cm from the surface) ( Fig. 58.4 ). Deep central parenchymal injuries seen on CT may be unrecognized at laparotomy, especially if the liver surface appears intact, and as a result, the true extent of involvement may be underestimated at surgery. It is imperative to describe any potential laceration extension to the hepatic or portal veins or to the inferior vena cava ( Fig. 58.5 ; see Fig. 58.3 ). Hematomas can also occur in hepatic trauma and may be subcapsular or parenchymal in nature. Subcapsular hematomas can be distinguished from free hemoperitoneum by mass effect on the liver surface, creating a contour deformity. Parenchymal hematomas follow the same attenuation values of blood as described before. Again, on contrast-enhanced CT, they may appear relatively lower in attenuation than enhancing liver parenchyma, but their attenuation values are often higher than simple fluid ( Fig. 58.6 ). Yet another type of hepatic injury, contusion, often appears as low-attenuation, sometimes ill-defined areas with intermixed areas of high attenuation representing blood.
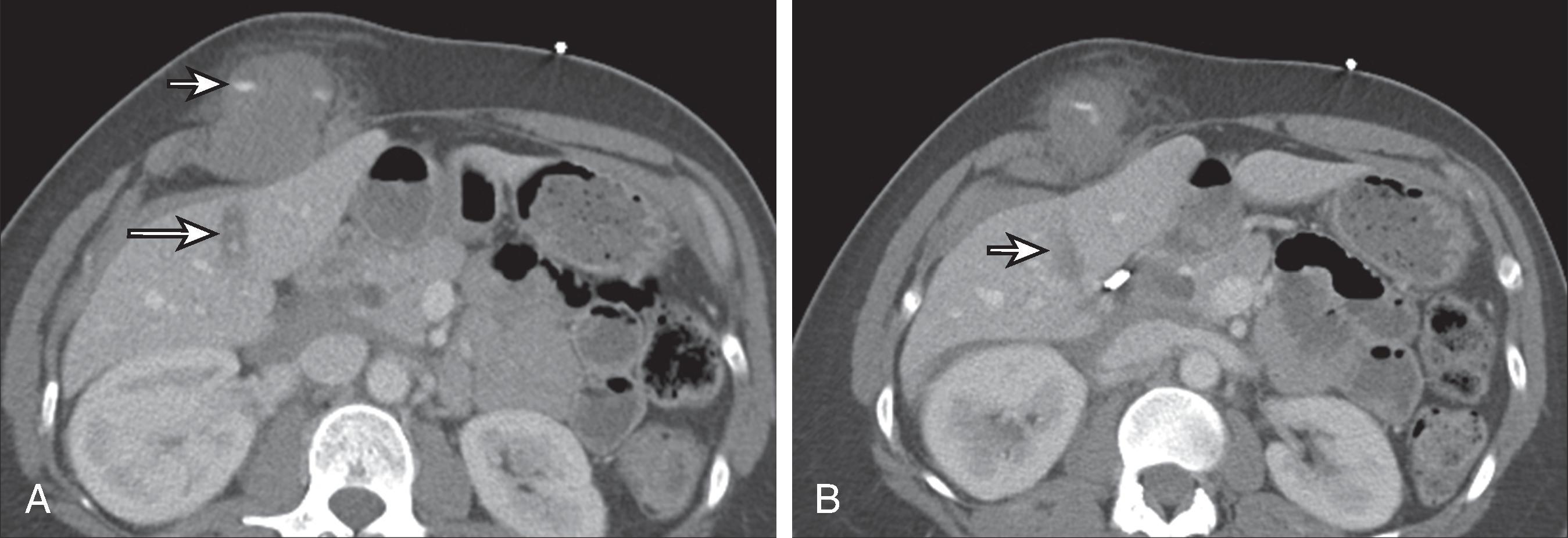
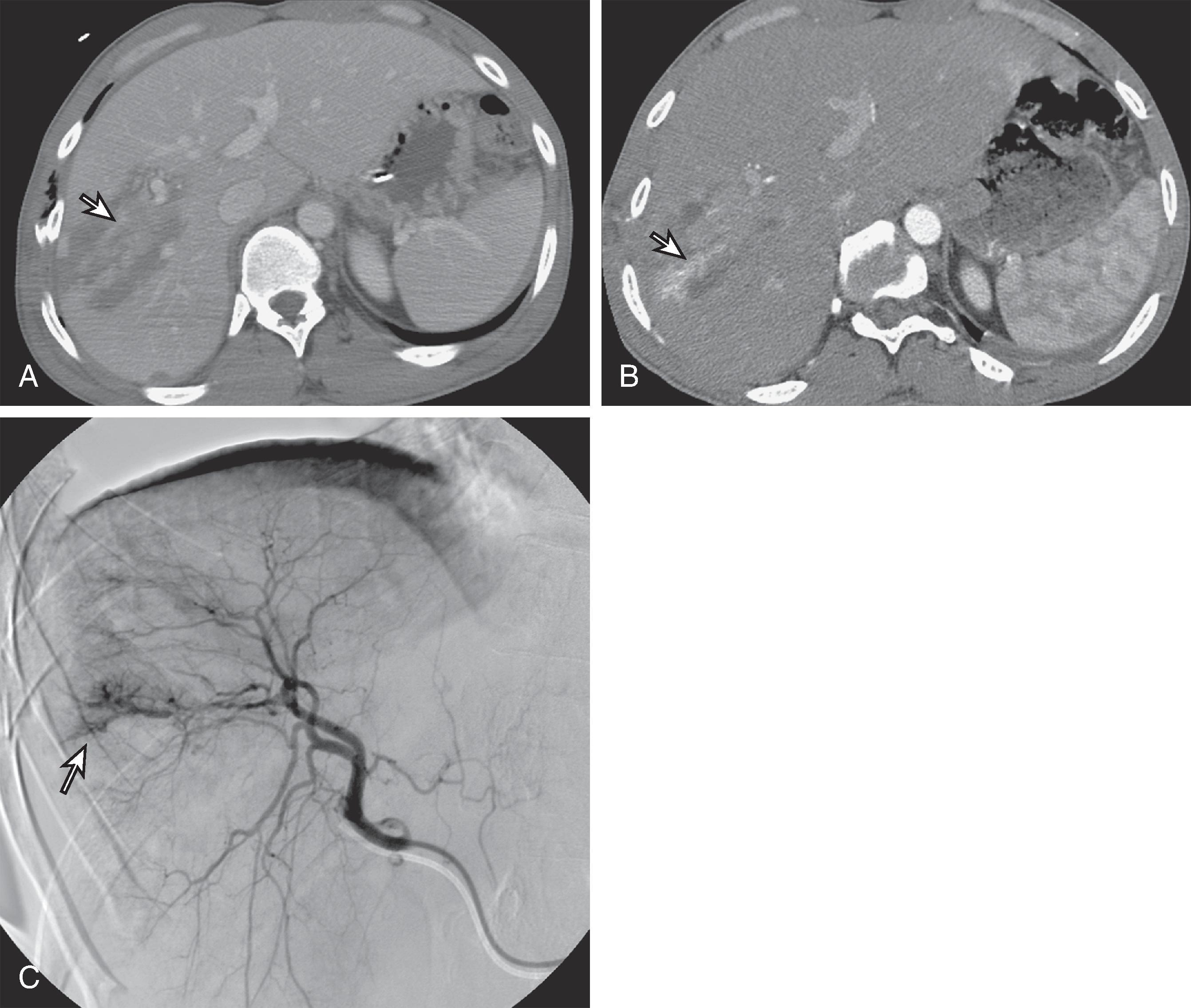
Active extravasation on contrast-enhanced CT represents one of the more severe CT features of hepatic injury and can herald life-threatening, active bleeding ( Figs. 58.7 and 58.8 ). On CT, this appears as very high attenuation approximating that of aorta (91–274 HU; mean, 155 HU) compared with the density of clotted blood (28–82 HU; mean, 54 HU). At times, active extravasation of contrast material may be difficult to distinguish from a pseudoaneurysm. Delayed contrast images are helpful in this instance, demonstrating “washout of contrast attenuation” with pseudoaneurysms (approximating the blood pool density at that time) and persistence of high density with active bleeding. Active extravasation of contrast material has been shown to be a strong predictor of potential cardiovascular collapse and failure of nonsurgical management. , Treatment of active extravasation is best performed through angiographic embolization.
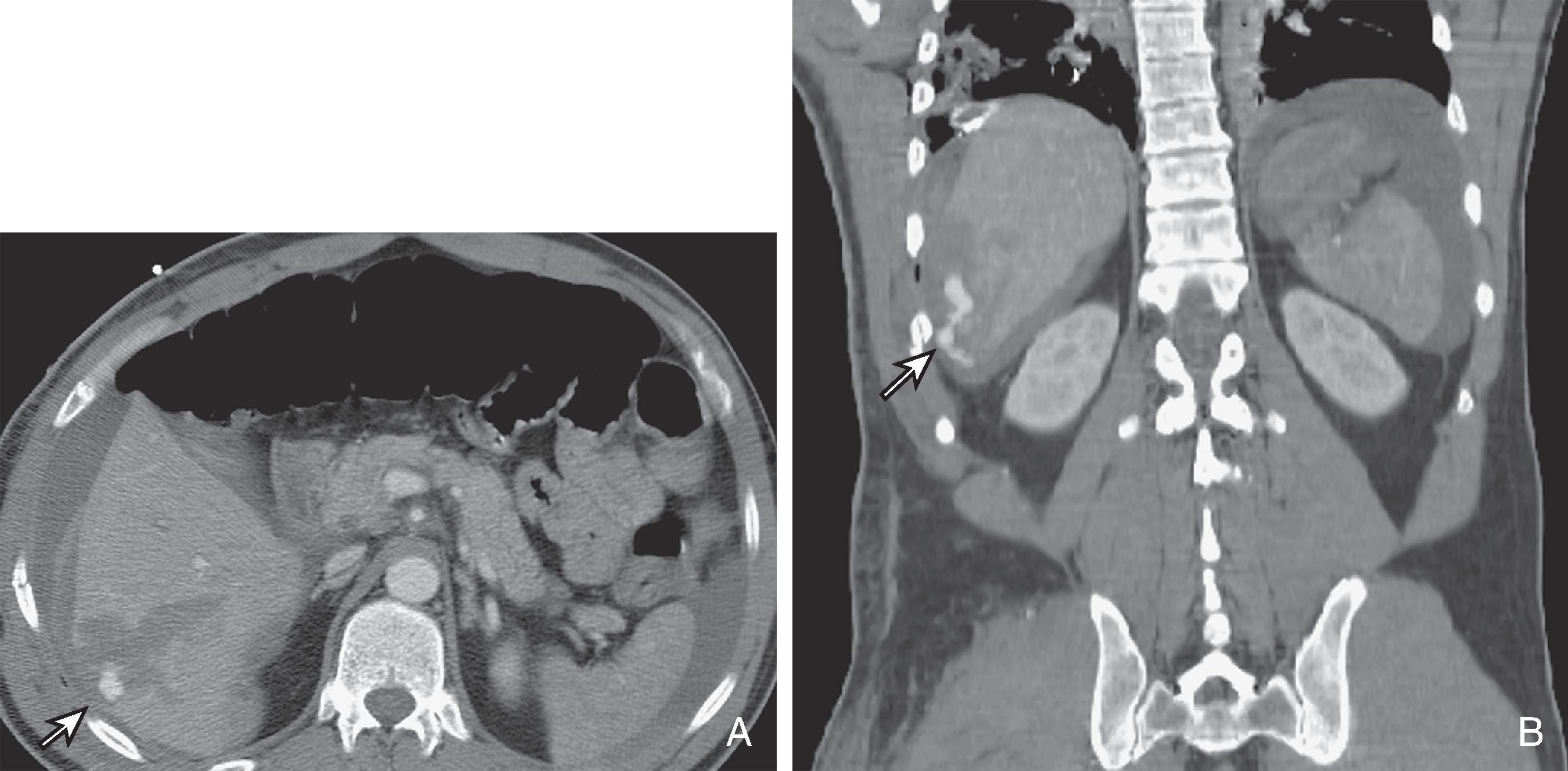
Vascular injuries of the liver, although relatively rare, can be fatal as well. When these occur, they are usually due to lacerations extending to the inferior vena cava, hepatic veins, and portal veins; thus, it is imperative to identify and to relay this extension to the clinicians (see Fig. 58.3 ). Alternatively, avulsion of the vessels can occur as well. Inferior vena cava injuries carry a particularly high mortality rate and should be suspected when there is a laceration extending to the proximal hepatic veins and inferior vena cava and when there is a large amount of retrohepatic blood. If bleeding occurs at the bare area of the liver, there may be extension of blood into the retroperitoneum as well.
Periportal zones of decreased density may be the only manifestation of hepatic trauma. These may represent linear collections of blood in the periportal regions or dilated periportal lymphatics. Periportal low density was previously thought to be an important sign of liver injury but is actually most commonly due to rapid fluid resuscitation, elevating central venous pressure, as suggested by a distended inferior vena cava ( Fig. 58.9 ). Periportal low density may also be seen in nontraumatic causes, including in patients with congestive heart failure, patients with hepatitis, liver transplant recipients, and those with AIDS. The lucency is due to a dilation of the intrahepatic lymphatics caused by obstruction of drainage. Intraparenchymal gas, in the absence of infection, has also been reported in patients with blunt abdominal trauma, but an abscess must always be excluded when extraluminal gas collections are present. ,

A CT-based classification has been formulated from these findings ( Table 58.2 ). This CT classification system grades the injuries; however, this grading system and the CT features may not correlate with the need for surgery. , It is not the grade of the injury but rather the hemodynamic parameters of the patient that often dictate conservative versus operative management decisions. Even major hepatic injuries up to and including grade IV can usually be managed conservatively if the patient is hemodynamically stable. , , CT findings associated with increased morbidity, mortality, and need for operation include deep perihilar lacerations, failure of the hemoperitoneum to be significantly resorbed within 1 week, rapid progression of hepatic injuries within hours or days of injury, and major vascular trauma (especially injury to the confluence of hepatic veins). , It has been noted that many hemodynamically stable patients can avoid operation despite significant injuries seen on CT examination. Although the CT-based injury grading system may not correlate with the need for surgery, it serves as a consistent means of describing and communicating injuries to surgeons. Radiologists should therefore be familiar with this grading system.
| Grade | Criteria |
|---|---|
| 1 | Capsular avulsion, superficial laceration(s) <1 cm deep, subcapsular hematoma <1 cm maximal thickness, periportal blood tracking only |
| 2 | Laceration(s) 1–3 cm deep, central/subcapsular hematoma(s) 1–3 cm diameter |
| 3 | Laceration(s) >3 cm deep, central/subcapsular hematoma(s) >3 cm diameter |
| 4 | Massive central/subcapsular hematoma >10 cm, lobar tissue destruction (maceration) or devascularization |
| 5 | Bilobar tissue destruction (maceration) or devascularization |
The need for follow-up CT examination to detect delayed complications is favored by some and opposed by others. , , Patients with persistent or worsening symptoms should have follow-up examinations. Patients with more severe, complex hepatic injuries may also benefit from repeated CT to evaluate injury status and possible complications. , Meredith and colleagues found that hemodynamic stability and lack of peritoneal findings were more predictive than the CT findings of which patients could undergo nonoperative management.
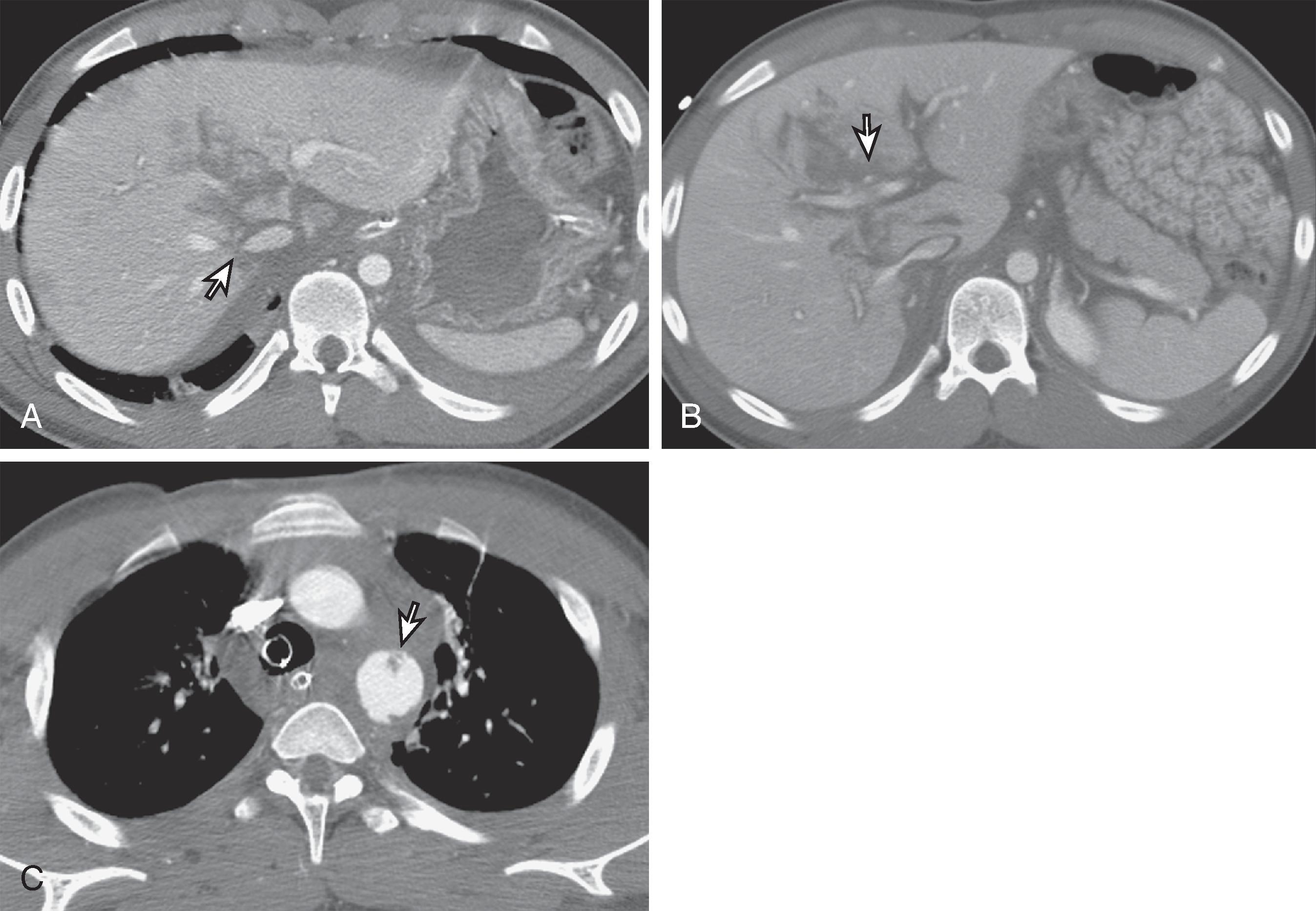
Post-traumatic complications are not uncommon after hepatic injury and are best demonstrated by CT as well. , Delayed hemorrhage can occur and can have a high mortality rate. This may be due to several causes, including an expanding injury, a biloma-induced pseudoaneurysm, a misinterpretation of contrast material extravasation on the initial CT scan, and mismanagement of the patient’s hemodynamic status ( Fig. 58.10 ). This should be suspected if there is a delayed drop in the hematocrit level. Post-traumatic pseudoaneurysms of the hepatic artery and its branches may occur weeks to months after the initial injury. These patients present with delayed hemorrhage and hemobilia (if the pseudoaneurysm decompresses into the biliary system) and should be evaluated with hepatic angiography, at which time the aneurysm can be embolized to minimize the risk of frank rupture. Bilomas ( Fig. 58.11 ) and intrahepatic and perihepatic abscesses are other major post-traumatic complications. Bilomas are seen in 0.5% to 20% of patients managed nonoperatively. , , , These fluid collections usually resolve or can be managed successfully by percutaneous drainage. Aspiration, biliary scintigraphy, or magnetic resonance imaging (MRI) may be necessary for differentiation of these fluid collections. , Endoscopic retrograde cholangiopancreatography (ERCP) can identify the bile leak and guide the insertion of a biliary endoprosthesis.
Ultrasound is being more frequently performed in the emergency department by surgeons, radiologists, and emergency department physicians. The advantages of sonography include portability, ability to rapidly detect intraperitoneal blood, and relative affordability. Problems include the operator-dependent nature of ultrasound and limitations in demonstrating the extent of injury.
The use of ultrasound was pioneered years ago in the European literature. Ultrasound can be used either to identify parenchymal injury directly or to detect intraperitoneal fluid that in the acute setting is presumed to represent hemoperitoneum. , Ultrasound is much more accurate in the detection of hemoperitoneum than in the diagnosis of specific parenchymal or hollow viscus injury. The recent interest in ultrasound is primarily in its utility as a rapid screening test for significant injury, the so-called focused abdominal sonogram for trauma (FAST). , FAST simply entails sonographic interrogation of sites in which free intraperitoneal fluid most often accumulates: Morison’s pouch, the left subphrenic and subsplenic areas, and the pouch of Douglas. It also involves evaluation for the presence of hemopericardium. According to Ma and colleagues, the suprapubic view is the single view most sensitive for hemoperitoneum (68%), but the sensitivity dramatically increases when multiple views are obtained. The best use of FAST is to triage patients. A hemodynamically stable patient with an abnormal finding on FAST should undergo CT scanning, whereas an unstable patient with an abnormal ultrasound finding should go to surgery emergently. Clinical management in cases with a normal finding on FAST is more nebulous, but at a minimum, those patients should be observed for a time.
Multiple studies have been published looking at the accuracy of ultrasound and comparing it with other modalities. In general, ultrasound is relatively sensitive for the detection of free intraperitoneal fluid, but it is far from perfect. There is a wide range of values in the literature for sensitivity (81%–94%), specificity (88%–100%), and accuracy (86%–98%) for free intraperitoneal fluid. This type of variability suggests inconsistent reproducibility of the method. In addition, for these values to be attained, some studies required repetitive sonographic scanning to detect developing fluid. Another confounding factor is that not all blunt abdominal trauma causes free fluid, with false-negative results. In some studies, 26% to 34% of patients with abdominal organ injuries did not have hemoperitoneum. Therefore, although ultrasound is very good in detecting hemoperitoneum, there are false-negative and false-positive findings. Diagnostic peritoneal lavage is a method to detect hemoperitoneum that was used commonly before the advent of ultrasound and CT. Diagnostic peritoneal lavage is known to be more sensitive than ultrasound in the detection of fluid and injury; however, positive diagnostic peritoneal lavage results led to a 30% rate of nontherapeutic, unnecessary laparotomies. , Diagnostic peritoneal lavage has been largely replaced with ultrasound and CT. In addition to the evaluation for hemoperitoneum, ultrasound can be used to detect other injuries. Ultrasound can demonstrate a number of traumatic lesions: subcapsular hematomas, parenchymal tears, contusions, and bilomas. A subcapsular hematoma appears as a lentiform or curvilinear fluid collection with echogenic properties that vary with the age of the lesion ( Fig. 58.12 ). Hematomas are initially anechoic, but as clotting proceeds, they become progressively echogenic by 24 hours. As time passes, the hematoma’s echogenicity begins to decrease again. , Internal echoes and septations develop within these collections in 1 to 4 weeks. The frequency of the transducer also determines the sonographic characteristics of the hematoma. The complexity and echogenicity of the hematoma can appear greater at higher frequencies as a result of higher spatial resolution. ,
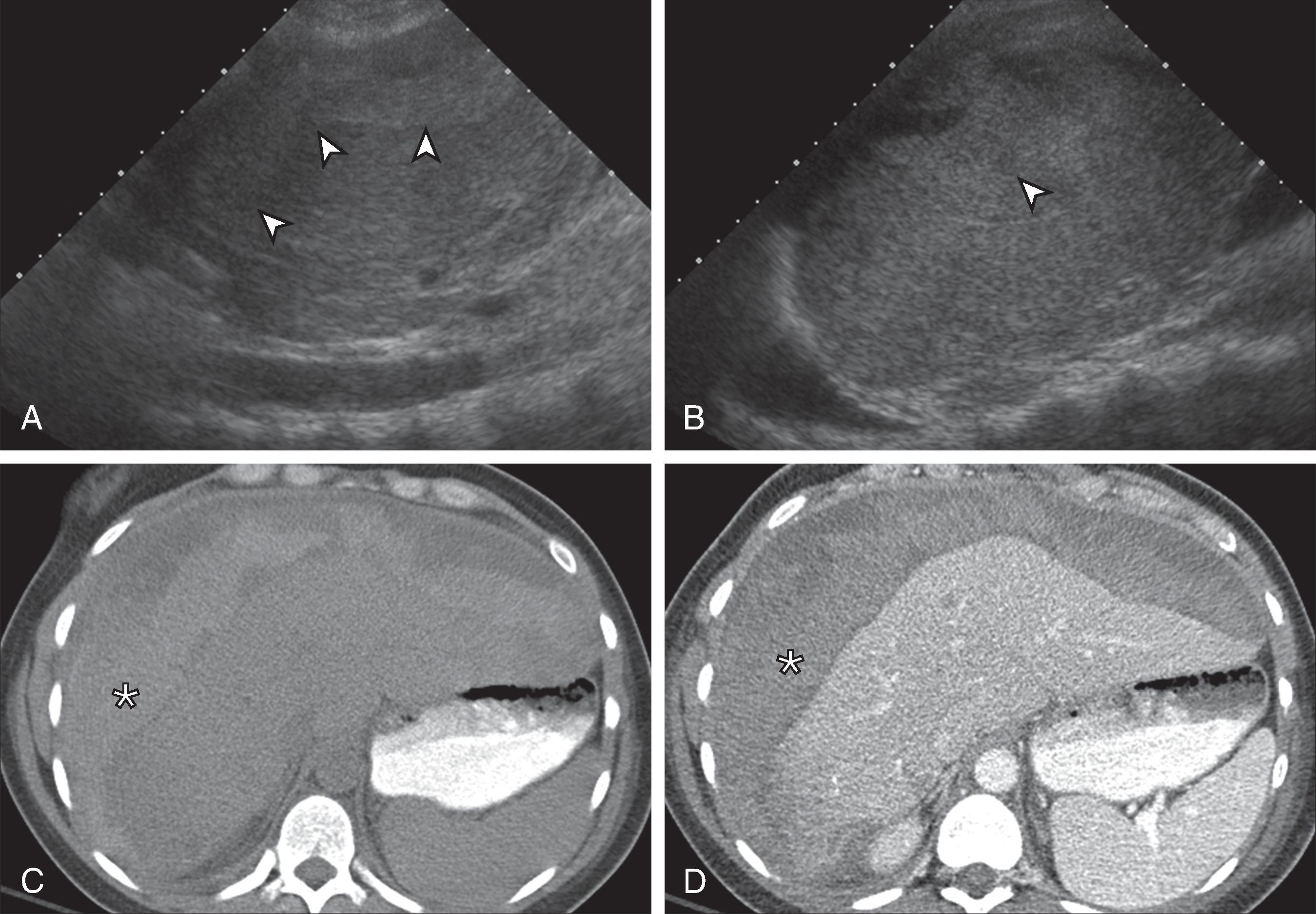
Parenchymal contusions are normally hypoechoic at initial presentation, transiently become hyperechoic, and then become hypoechoic. Lesions that occur posteriorly in the right lobe or over the spine within the left lobe are usually not sonographically demonstrable unless the patient has a slender body habitus. Parenchymal tears, with or without hematoma, are manifested as irregular defects with abnormal echotexture relative to the surrounding normal tissue. Intraparenchymal hematomas as small as 3.5 mL can be visualized as rounded, echogenic foci.
Bilomas appear as rounded or ellipsoid, anechoic, loculated structures with sharply defined margins close to the liver and bile ducts. Scintigraphy is an important adjunct in these cases to show communication of the lesions with the normal biliary tract. Fluid aspiration may be helpful to demonstrate bile. , Ultrasound is particularly helpful diagnostically when the collections no longer communicate with the biliary tract. Percutaneous drainage with CT or sonographic guidance may be helpful when fluid collections are symptomatic or infected.
Many studies have evaluated the accuracy of ultrasound for detection of parenchymal hepatic and other solid organ injuries. Sensitivity for detection of all injuries ranges from 43.6% to 93%. This wide range of numbers is due to many factors, including study design, technique, and experience. Papers with very low sensitivities often include small bowel and mesenteric injuries, which are extremely difficult to detect by ultrasound. With respect to liver parenchymal injury specifically, an article by Sato and Yoshii comparing ultrasound examination with both the clinical outcome and CT revealed a sensitivity for hepatic injury of 87.5% among experts and 46.2% among nonexpert sonographers. This suggests that detection of injuries sonographically is more difficult than simply scanning for hemoperitoneum, and can be variable. Other pitfalls of ultrasound, however, include limitations in the evaluation of retroperitoneal injuries, diaphragmatic injuries, and hollow viscus perforations.
Some authors have experimented with contrast-enhanced ultrasound in the evaluation of hepatic trauma. These contrast agents use stabilized, encapsulated microbubbles that are small enough to pass through the pulmonary circulation to reach the systemic circulation and ultimately parenchymal tissue. Contrast agents have many potential uses in the heart and vascular system as well as in the detection of focal lesions. In the trauma setting, Catalano and colleagues have demonstrated that contrast-enhanced sonography is a promising tool that better depicts hepatic lacerations and hematomas as echo-poor areas against a background of enhanced parenchyma. It also appears to demonstrate the extent of lesions better than conventional sonography. In addition, it may also have a role in detecting active extravasation of contrast material and therefore active bleeding, which cannot be done with conventional ultrasound. In their study, contrast-enhanced sonography (87%) had a higher sensitivity than routine ultrasound (65%) for hepatic injury detection. This may potentially be a powerful tool in the emergency department setting in the future.
Bile leaks are rare in blunt hepatic trauma. They more often follow cholecystectomy and partial hepatectomy. Hepatobiliary scans, the most sensitive means of detecting bile leakage, may identify the leak before the onset of clinical symptoms. With bile leakage, the tracer may appear as a subcapsular collection or may pool freely in the peritoneal cavity. Parenchymal injuries such as lacerations and hematomas are easily identified on early hepatic phase images.
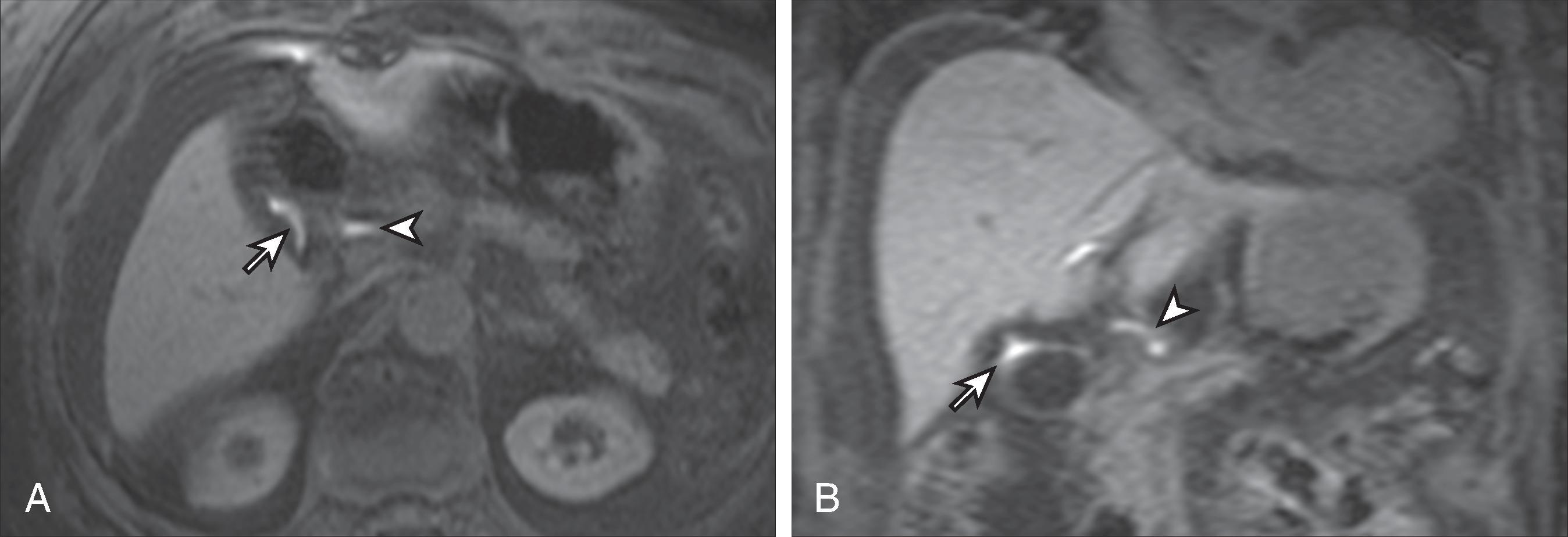
Gadolinium-enhanced MRI can depict complex hepatic injuries in patients with contraindications to iodinated contrast material. Contrast-enhanced MRI has been shown to demonstrate traumatic hepatic injuries equal to and, occasionally, better than contrast-enhanced CT. MRI, however, requires a longer imaging time as well as the need to accommodate metallic life support and monitoring equipment, which is more difficult than with CT. In addition, the MR screening process, which is necessary for the safety of the patient, is a timely process that is often not possible in a trauma setting where immediate decisions need to be made. Furthermore, images are compromised by motion to a greater extent than with CT as well as by limited evaluation of the bowel. MRI can help differentiate bilomas from subacute hematomas. , Despite these limitations, MRI may have a role in imaging of the trauma patient, although its use has not been thoroughly evaluated. With the advent of gadolinium-based hepatobiliary agents such as gadobenate dimeglumine (MulitHance; Bracco Diagnostics) and gadoxetate (Eovist; Bayer HealthCare), the biliary tree can be evaluated in a functional way. These hepatobiliary agents have dual excretion through the kidneys and liver. The contrast agent is taken up by the hepatocytes and excreted through the biliary tree. Approximately 50% of gadoxetate is excreted through the liver, whereas 5% of gadobenate has hepatobiliary excretion. This biliary excretion allows visualization of the bile ducts and any bile leaks or bilomas on T1-weighted MR sequences, on which the gadolinium portion of these agents will cause T1-weighted shortening and increased signal on T1-weighted images. Imaging for the hepatobiliary phase of biliary excretion is done in a delayed fashion after routine images. With Eovist, a delay of approximately 20 to 30 minutes is used; with MultiHance, a delay of 60 minutes is optimal. The few studies performed for the evaluation of bile duct injury have been in iatrogenic injuries after surgery. In this setting, MR has been shown to find and to characterize bilomas with a sensitivity of 80% to 96%. , Many other types of biliary abnormalities, including strictures, leaks, obstructions, and anatomic anomalies, can be depicted with these agents ( Fig. 58.13 ). Although it is still a Food and Drug Administration off-label application of these agents, functional biliary imaging with these contrast agents is extremely promising. Apart from identifying biliary injury, MRI may also have a role in follow-up of previously detected hepatic injuries. In severe hepatic injury in which follow-up imaging is warranted, the use of MRI over CT may save a significant radiation dose to often young patients, particularly if multiple follow-up examinations may be needed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here