Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Symptomatic large and massive rotator cuff tears are common with advancing age. Among those who undergo rotator cuff repair surgery, reasonable clinical outcomes have been reported in the majority of patients; however, complete tendon-to-bone healing is uncommon, with retear rates ranging from 40% to over 90%. In order to improve healing rates, various scaffolds have been investigated to augment these tears at high risk of retearing. In addition, some tears are not fully repairable, and grafts have been used to bridge the defect in the cuff tendon. In this chapter, we describe the use of human dermal allograft as both an augmented graft and an interposition graft because of its favorable biologic and mechanical properties.
A dermal allograft patch can be used either to bridge a defect greater than 1 cm in size (interposition) or to augment a complete repair (augmentation). We prefer to use an arthroscopic technique over an open technique, largely owing to improved visualization and preservation of the deltoid attachment. Sutures are passed through the graft outside the shoulder, and knots are tied on one end of the suture; the other end of the suture is shuttled into the joint through the native cuff tissue and out another cannula. These medial ends are then slowly pulled, which draws the graft into the joint. The suture ends are then tied together, firmly fixing the graft to the native tissue.
Night pain is common.
Chronic limiting activity–related shoulder pain.
Physiologically “young,” typically 50- to 70-year-old age range.
Note prior surgery, and obtain operative reports if possible.
Inspection: Note prior incisions; deformity (such as scapular winging); and muscle atrophy, including the deltoid and supraspinatus/infraspinatus fossae.
Palpation: Tenderness to palpation of the periscapular musculature, acromion, subacromial bursa, acromioclavicular (AC) joint, clavicle, and biceps tendon can identify concomitant pathology.
Range of motion (ROM): Active forward flexion is often painful, typically above 130 degrees. Passive ROM is variable but often normal. Supine internal/external rotation testing with the arm abducted 90 degrees can assist in identifying concomitant adhesive capsulitis.
Strength: Weakness during supraspinatus testing is a clinical hallmark. Testing is performed with the arm abducted in the scapular plane, internally rotated, and with the hand slightly below shoulder height. Assess external rotation strength with the elbow adducted to the side; this will identify involvement of the infraspinatus/teres minor. Belly press/lift-off/bear-hug testing can assist in identifying subscapularis pathology.
Special testing: Results of provocative impingement and biceps testing are often positive secondary to bursal inflammation and bicipital degeneration in large rotator cuff tears.
We routinely get four standard views of the shoulder for all new patients: a true anteroposterior (AP) view (Grashey), a supraspinatus outlet or “arch view,” an axillary lateral view, and an AC joint (Zanca) view.
Joint space narrowing and other signs of osteoarthritis are noted on axillary lateral and true AP views. Rotator cuff arthropathy is a contraindication to allograft repair.
We use mostly noncontrast magnetic resonance imaging (MRI). Intraarticular gadolinium contrast is useful to assess the integrity of prior rotator cuff repair but is rarely needed to assess the need for use of dermal allograft. Other pathologies, such as AC joint arthropathy, biceps tendinopathy, and subscapularis tendon tears, are assessed and planned for accordingly. The articular surface is carefully evaluated; minor articular defects are not considered a contraindication, whereas larger full-thickness defects are.
The presence of an “S-wave” is favorable for primary cuff repair. This is present when cuff tissue has a recoiled appearance on coronal MRI images ( Fig. 23.1 ).
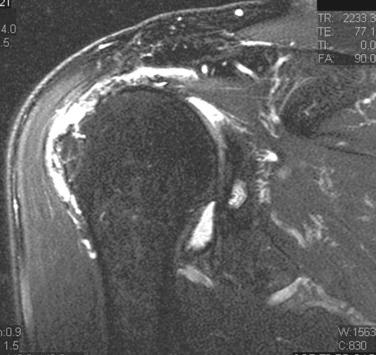
Dermal allograft augmentation should be considered when an MRI shows an “at-risk” tendon that has a thin diminutive appearance but likely can be reapproximated to bone ( Fig. 23.2 ).
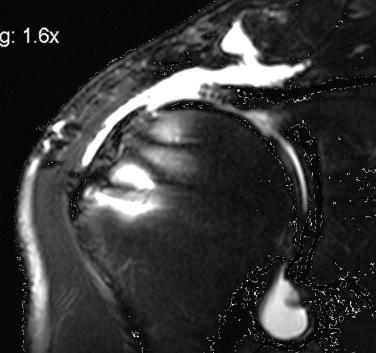
Interposition grafting is considered in cases where MRI shows a segmental tendon defect that likely will not allow reduction to the tuberosity. This is occasionally observed in Cho type II failures near the musculotendinous junction after double-row rotator cuff tendon repair ( Fig. 23.3 ).
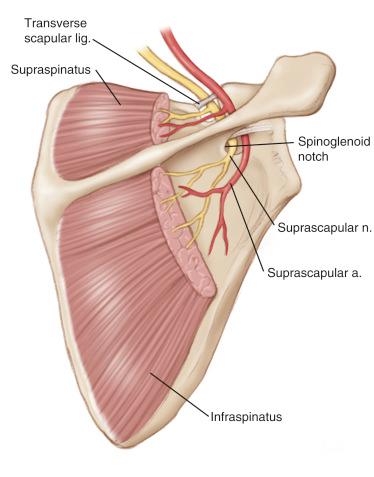
We do not routinely order electromyography with nerve conduction studies to evaluate the suprascapular nerve. Suprascapular nerve decompression at the time of surgery is controversial and of uncertain clinical benefit. Rotator cuff tendon reduction near its anatomic footprint presents the best option for “untethering” the suprascapular nerve. However, in cases where interposition grafting is used and the cuff remains in a more retracted position, decompression of the suprascapular nerve at the time of repair may have a theoretical benefit. More investigation is warranted before recommending for or against nerve decompression in these instances.
Conservative treatment: Nonoperative treatment of rotator cuff tears consists of physical therapy, nonsteroidal antiinflammatory drugs (NSAIDs), and steroid injections. An initial course of physical therapy with NSAIDs is appropriate for those with more minor rotator cuff tears and for patients apprehensive about undergoing surgery. We typically limit patients to one or two steroid injections total.
Partial rotator cuff tendon repair: There are instances where patients cannot have dermal allograft repairs despite being ideal candidates (e.g., financial, cultural). Partial repairs that address concomitant pathology will often give them some relief but with guarded expectations about shoulder function and pain alleviation.
Reverse total shoulder arthroplasty: Ideal for patients with rotator cuff arthropathy that precludes rotator cuff repair. Although repair of the tendon is often feasible, a frank discussion must address whether a cuff repair will alleviate the patient’s symptoms, because complaints related to osteoarthritis may be unchanged or become worse.
Latissimus dorsi tendon transfer: Data in the literature regarding improvement after latissimus dorsi tendon transfer have shown favorable results. No currently existing studies compare dermal allograft interposition with tendon transfer, and thus more investigation is required.
Superior capsular reconstruction: This emerging technique is currently being investigated. We have noted on rare occasions that medial rotator cuff tissue is inadequate even for dermal allograft interposition. In these cases, superior capsular reconstruction may present a viable option.
Scapular spine: Visualization of scapular spine serves as a reference for the “midpoint” of the tendon while placing medial sutures ( Fig. 23.4 ).

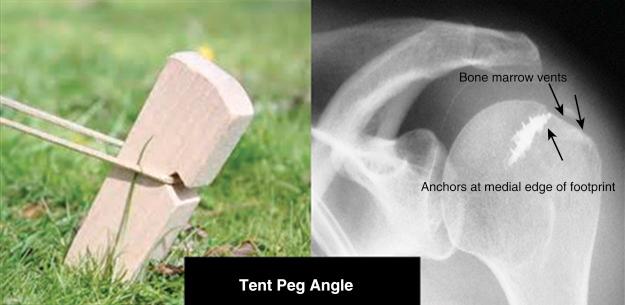
Humeral footprint anatomy: Anchors are ideally placed at the medial supraspinatus/infraspinatus footprint 5 mm from the articular cartilage at a 45-degree “tent peg” angle ( Fig. 23.5 ).
Suprascapular nerve: Overly aggressive medial debridement will place the suprascapular nerve at risk ( Fig. 23.6 ).
Tear classification: Rotator cuff tears are described by pattern (e.g., L-shaped or reverse L-shaped, stellate, “monk’s hood”) and classified using the system described by Snyder ( Table 23.1 ). When complete lesions are found, which is often the case with larger tears considered for dermal allograft, the size of the complete tear follows the “C” designation scheme:
CI: A small complete tear, such as a puncture wound, would be rated CI.
CII: A moderate tear that still encompasses only one of the rotator cuff tendons with no retraction of the torn ends would be rated as a CII lesion.
CIII: A CIII lesion involves an entire tendon with minimal retraction of the torn edge, usually 3 cm in size.
CIV: A massive rotator cuff tear (CIV) involves two or more rotator cuff tendons, frequently with associated retraction and scarring of the remaining ends of the tendon and often an L-shaped tear. When a CIV cuff tear cannot possibly undergo direct repair to the greater tuberosity, it is termed “irreparable.”
| Classification of Rotator Cuff Tears |
|---|
Location of tear
Severity of tear
|
Persistent activity-related shoulder pain and failure of other conservative measures are common indications for operative rotator cuff repair. Symptomatic full-thickness rotator cuff tears with retraction are generally treated surgically because the risk of progression to an irreparable tear is significant.
Once a patient elects to undergo rotator cuff repair, the first decision a surgeon must make is whether the rotator cuff tear is likely to be repairable using standard techniques based on clinical exam and imaging.
Ideal candidates for dermal allograft use include the following:
Failed prior repairs
Fatty infiltration
Muscle atrophy
Thin, degenerative tendon
Large tears (>2 cm)
Significant retraction (beyond humeral apex)
Chronic traumatic tears
History of failed repair on contralateral shoulder
Patients are advised that the final decision on whether to use the graft, augment, or perform an interposition procedure is made intraoperatively.
One or more of the above risk factors warrants preparation for the use of dermal allograft. There are few absolute contraindications to using a graft, but patient bias against using an allograft must be respected. Cost, additional time requirement, and surgeon’s comfort level are relative contraindications.
Note: Use of patches is approved by the U.S. Food and Drug Administration (FDA) only as an augmentation with less than 1-cm defect; therefore interposition is currently an “off-label” use, and patients should be informed of the FDA status.
We prefer the lateral decubitus position. The patient is positioned on a bean bag with pillows placed under the down leg and between the knees and ankles. A thick gel pad is placed as an “axillary roll.” Care must be taken to avoid pressure from the bean bag in the axilla of the down shoulder because this can cause brachial plexus damage.
The operative arm is placed in traction using a commercially available sleeve or well-padded arm holder. Three positions are used: standard, bursal, and midpositions. The standard position generally uses 10 pounds of balanced suspension in 70 degrees of shoulder abduction and 5 degrees of forward flexion; it is used for glenohumeral work. Switching to the “bursal” position requires moving the arm to 20 degrees of abduction while remaining in 5 degrees of forward flexion and adding 5 pounds of traction; it is used for all work in the bursal space, including rotator cuff surgery. The “midposition” can be used to improve visualization in certain cases and also allows access to the lateral aspect of the greater tuberosity for lateral anchor placement. The arm is placed in 45 degrees of abduction.
Standard shoulder arthroscopy draping is then used ( Fig. 23.7 ).

Standard arthroscopic shoulder instrument set
Electrocautery, motorized shaver
Four arthroscopic cannulas (one at least 8.5 mm for graft passage):
One 5.75- × 70-mm smooth Crystal cannula (Arthrex, Naples, FL).
Two 7- × 85-mm blue Dry-Doc cannulas (ConMed/Linvatec, Largo, FL).
One 8- × 75-mm red Dry-Doc cannula (ConMed/Linvatec, Largo, FL).
Have available a 10-mm cannula with external rubber diaphragm (Smith & Nephew, MA) to be used when graft exceeds 3.5 mm in either direction.
Two high-strength braided permanent sutures and two push-in–style suture anchors (for lateral fixation in augmentation)
Two to four triple-loaded suture anchors (ThRevo Suture Anchors as used in the figures in this chapter; ConMed/Linvatec, Largo, FL)
Six or seven No. 2 braided polyester sutures for short-tailed interference knots (STIKs) (ETHIBOND; Ethicon, Somerville, NJ)
Acellular dermal allograft (>1.8 mm thick)
Suture hook system for shuttling (Spectrum II and Super Shuttle; ConMed/Linvatec, Largo, FL)
Suture saver colored plastic suture protectors (if performing interposition) (ConMed/Linvatec, Largo, FL)
No. 0 VICRYL suture (Ethicon, Somerville, NJ) for knotted suture measuring device
Bone punch (2 mm) for creating bone marrow vents
Revo 2-mm bone punch (ConMed/Linvatec, Largo, FL)
Preparation for dermal graft includes a complete examination of the joint followed by bursoscopy and subacromial decompression. Anterior midglenoid portal (AMGP) and posterior midglenoid portal (PMGP) cannulas are placed with a larger midlateral subacromial portal (MLSAP) to allow passage of the graft. An optional posterolateral portal (PLP) can aid in speed and convenience but has the disadvantage of creating an additional incision. If individual patient physiology allows, controlled hypotensive anesthesia (goal systolic blood pressure ∼90 mm Hg) in the lateral decubitus position can minimize bleeding and improve visualization. Fluid extravasation into the soft tissues can be minimized by maintaining the deltoid fascia where practical, as well as by keeping the pump pressure as close to 35 mm Hg as possible. A debridement that allows excellent visualization with identification of the scapular spine is crucial. The scapular spine is used as a midline reference point when placing medial sutures. The final decision whether to perform an augmentation or interposition graft will ultimately depend on the ability to reduce the cuff to the medial footprint in a low-tension fashion. To a certain extent, this depends on the “feel” of cuff tension. If the cuff can be reasonably reduced to the medial footprint using a looped forceps, it is likely a good candidate for augmentation. If not, an interposition graft is more appropriate.
Draw the exterior bony anatomy (clavicle, AC joint, acromion, scapular spine, midacromial orientation line).
Create a standard PMGP and AMGP. The AMGP is most efficiently made by placing the scope in the rotator interval, placing a switching stick through the scope sheath to pierce the rotator interval, and then making a small incision to pass the switching stick “through and through” out of the skin. A Crystal cannula can then be placed over the switching stick, followed by introduction of the arthroscope.
Perform a complete 15-point arthroscopic glenohumeral evaluation, viewing from both the posterior and anterior portals. Document the condition of the cartilage surface, labrum, biceps, subscapularis, synovium, and articular portion of the rotator cuff.
Prepare the shoulder joint by debriding frayed and loose tissue.
If suture material is present within the degenerative cuff edges, it can be removed, and the cuff edges can gently be debrided. Debriding the tendon edge may aid in healing by removing proapoptotic factors detrimental to tissue regeneration.
Releases of the rotator cuff are initially performed from within the glenohumeral joint space. The shaver at this stage can be used to bluntly dissect, release adhesions, and mobilize any scar tissue that has formed.
The medial stump of the rotator cuff can be carefully released by mobilizing scar and capsule just above the glenoid.
Repair any significant subscapularis or labral pathology as needed.
Remove the arthroscope and anterior portal and perform subacromial bursoscopy.
Prior to reinsertion of the arthroscope, the arm is placed into the “bursal position” to allow better visualization of the subacromial space. Traction is generally increased to 15 pounds.
With the arm in adduction, the bursal space is entered, and a full evaluation of the anatomy is performed.
Thoroughly debride bursal tissue, viewing from the anterior and posterior portals to visualize the entire rotator cuff. Keep the deltoid fascia intact when possible to minimize fluid extravasation. Hemostasis is obtained with electrocautery.
Previously placed anchors are left in place if possible but removed if they are obstructing the bone needed for graft attachment near the articular edge of the humerus.
If there are cysts or large bony defects that will likely compromise fixation stability of the new anchors, they should be filled with a suitable bone graft material.
Create an MLSAP using a spinal needle to localize over the midpoint of the cuff tear. This will be used as a working portal and also for graft passage. The entry of the spinal needle is generally 3–4 cm distal to the lateral acromion and near the midacromial orientation line.
When the MLSAP is centered over the cuff defect, it may not be centered on the acromion in the sagittal plane.
Perform subacromial decompression, AC joint resection, or biceps procedure as necessary. Debride all soft tissues off the greater tuberosity to cortical bone. This will create a better surface for regrowth of the footprint ( Fig. 23.8 ).

Insert 7-mm Dry-Doc arthroscopic cannulas in the AMGP and PMGP. An 8.5-mm Dry-Doc cannula is placed in the MLSAP.
If the cuff defect is very large (over 3.5 cm in either dimension), a 10-mm-diameter cannula with an external rubber diaphragm is recommended to allow passage of the graft in the cannula.
A final check on visualization with debridement of soft tissues and hemostasis is quickly performed prior to starting repair procedures.
Using a ring forceps, we perform a trial reduction of the rotator cuff, which represents a key branching point in our decision process. After grasping the apex of the cuff, if it can be easily reduced to the medial footprint, we perform a standard “SCOI row” repair (so named for the Southern California Orthopedic Institute, where it was first developed) in patients without previously mentioned risk factors for failure. If a reduction is feasible but with a moderate amount of tension, we perform a repair with augmentation. If reduction requires great effort or is impossible, we perform a graft interposition.
Optional portal: A PLP can be created for visualization during suture and graft passage. This portal should be placed just posterior to the middle of the tear such that it will have complete visualization throughout the case, including the entire tear, the greater tuberosity, and the MLSAP as it enters the subacromial space. Visualization of the aperture of the MLSAP cannula is particularly important because introduction of the grasper can be directly visualized when retrieving sutures, thereby assuring that entanglement has not occurred. The disadvantage of this portal is that it creates an additional incision. The benefit is that work in the AMGP and PMGP can continue without switching the camera between them. For illustrative purposes, an accessory PLP is used in the section of this chapter describing augmentation.
The patient should have good passive and active assisted ROM of the shoulder with minimal arthritis.
Not all graft materials are alike. The rotator cuff graft must be chosen with care, avoiding materials that are weak or likely to incite inflammatory reaction, as well as those with cross-linked collagen, which are likely to retard cellular ingrowth.
The operation should be rehearsed until the steps are second nature for the surgeon, the assistant surgeon, and the operating room staff. Develop skills and comfort using the three basic subacromial portals.
Be very careful when positioning the patient for surgery. The prolonged surgical time will increase the risk of pressure points on the nerves and skin.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here