Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Condyloma acuminatum is a benign exophytic lesion caused by infection with low-risk human papillomavirus (HPV) subtypes, principally types 6 and 11.
Condylomata are asymptomatic, usually multiple and often multifocal, presenting as papillary growths varying in size from barely visible on gross examination to several centimeters.
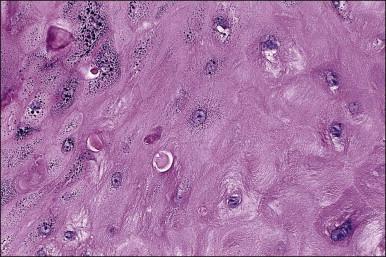
On histologic examination, the lesion consists of complex branching fibrovascular cores covered with acanthotic squamous epithelium, frequently with accompanying hyperkeratosis and parakeratosis. Pathognomonic findings include basal and parabasal hyperplasia, with koilocytic atypia, manifested by enlarged, hyperchromatic nuclei with irregular, wrinkled nuclear membranes accompanied by a region of perinuclear clearing or ‘halo,’ in the upper third of the epithelium ( Figures 4.1 and 4.2 ).
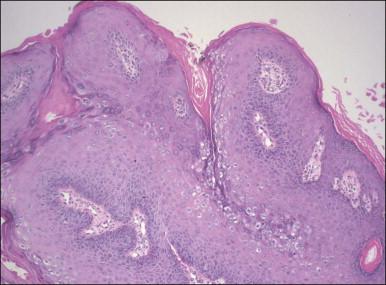
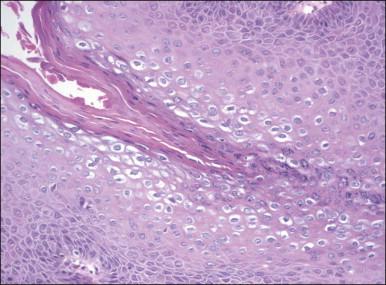
Immunohistochemical reactivity with Ki-67 in condylomata demonstrates cells active in the cell cycle at all layers of the epithelium, which is helpful to distinguish them from other benign exophytic lesions of the vulva, such as fibroepithelial polyp and seborrheic keratosis. Although warty vulvar intraepithelial neoplasm (VIN) and the warty type of squamous cell carcinoma may show marked koilocytic atypia in the superficial cells, they are distinguished from condyloma by the presence of nuclear atypia and numerous, frequently atypical, mitotic figures in deeper layers of the epithelium. Verrucous carcinoma is grossly similar to condyloma, but is distinguished by its characteristic growth pattern with a pushing invasive border.
Condylomata may regress spontaneously, but usually persist and may increase in size or number over time. They are not considered premalignant, and do not progress to high-grade VIN or carcinoma. Small lesions can be treated with topical agents or laser or electro-loop ablation. Extensive lesions may require superficial surgical excision.
Seborrheic keratosis is a benign, frequently pigmented wart-like growth common on the sun-exposed skin of the elderly and less commonly seen on the hair-bearing skin of the vulva.
The typical appearance is of an elevated, often macular–papular, flesh-toned or hyperpigmented lesion, which is well demarcated from the surrounding skin, giving the impression of being ‘stuck-on’ to the surface. Because of the superficial, exophytic nature of the lesions, they are prone to irritation and trauma, which may lead to secondary changes of inflammation, erythema, and crusting.
The epidermis is thickened by a population of cells with basaloid morphology, without significant nuclear atypia or mitotic activity, and with pronounced surface hyperkeratosis. Pigmentation of the basal and parabasal cells is usually evident. Invaginations of the surface epithelium result in the accumulation of hyperkeratotic material below the surface of the lesion, in what may appear to be cystic spaces, forming the structures known as ‘horn cysts’ ( Figure 4.3 ). Follicular plugging with this hyperkeratosis is also typical. ‘Squamous eddies,’ rounded whorls of squamous cells named for their resemblance to swirling currents in a stream, may be found ( Figure 4.4 ).
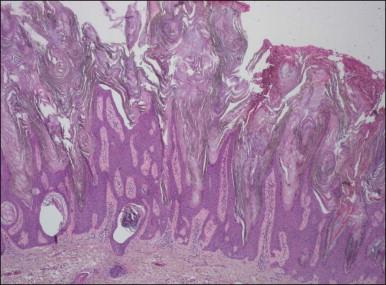
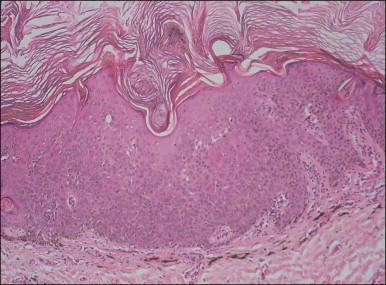
On occasion, reactive changes secondary to trauma or prominence of squamous eddies can be suggestive of squamous cell carcinoma. Key to establishing the correct diagnosis in such cases is the absence of an infiltrative growth pattern. Other entities in the differential diagnosis of seborrheic keratoses on the vulvar skin include condyloma acuminatum, VIN, and melanoma. The papillary architecture and hyperkeratosis of seborrheic keratosis can be suggestive of condyloma, particularly at low power. As seborrheic keratoses are frequently found to contain HPV DNA, some authors have maintained that these lesions are, in fact, variants of condyloma, although this remains controversial. The absence of koilocytic atypia in seborrheic keratosis and of keratin horn cysts in condylomata will usually resolve the diagnosis. The lack of significant nuclear atypia or mitotic activity is also of use to differentiate seborrheic keratosis from VIN and melanoma, with immunohistochemistry of further use in distinguishing the latter.
Treatment is identical to that of vulvar condylomata; both excisional and topical treatments are available and effective.
Keratoacanthoma is a distinctive keratinocytic neoplasm characterized by rapid growth and spontaneous regression. Although often considered a low-grade variant of squamous cell carcinoma, this view is not universally accepted, and as there have been no reported cases of malignant behavior in cases presenting on the vulva, we present it here as a benign neoplasm.
Keratoacanthoma characteristically presents as a rapidly growing pink or flesh-colored, firm, well-demarcated dome-shaped lesion with central umbilication. Although common on the sun-exposed skin of the elderly, very few cases occurring on the vulva have been reported.
The dome-shaped, umbilicated lesion observed on the skin corresponds to an endophytic proliferation of squamous cells forming a keratin-filled crater-like center rimmed by collarette, or ‘buttressing lips,’ of epidermis. The central squamous cells are well differentiated and tend to become larger toward the center of the proliferation, accumulating abundant glassy, eosinophilic cytoplasm ( Figures 4.5 and 4.6 ). In the early stages of development, mitoses may be numerous and mild to moderate nuclear atypia may be present, but these features regress as the lesion matures, and when well developed only minimal atypia is present. The lesions typically have a rounded, pushing border with a dense inflammatory infiltrate at the base of the lesion.

Focal, small, irregular nests of cells, and less commonly perineural or intravascular invasion adjacent to the pushing border of keratoacanthoma may occasionally be seen. Such seemingly infiltrative patterns can be alarming, but in the absence of other features do not warrant a malignant diagnosis.
Untreated, keratoacanthoma typically increases rapidly in size over a period of weeks to months and then may persist for months until finally undergoing spontaneous involution, usually within six months of eruption. Excision is usually curative, with rare recurrences reported.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here