Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter includes an accompanying lecture presentation that has been prepared by the authors: ![]() .
.
Our capabilities as surgeons have increased as our ability to visualize has advanced through technology and art.
The operating microscope revolutionized our field beginning in the 1950s, and intraoperative visualization continues to improve.
Art has had a huge impact on surgeons since the Renaissance, and has become more useful as artistic techniques and technologies for image manipulation have developed over hundreds of years.
We are now living in a second Renaissance related to computer technologies that are radically transforming how images are manipulated and presented in every realm of surgery.
With the introduction of the operating microscope in the 1950s, a vast improvement in visualization led to a profound transformation of neurosurgery. This disruptive technology presented surgeons with an opportunity to perform more precise operations with better outcomes, but significant advances by pioneers such as Kurze, Yaşargil, and Rhoton were required before surgeons’ abilities could match the improved surgical views. New instruments and surgical techniques were developed in order to delicately dissect the fine structures that became visible through the operating microscope, and the resulting need to better understand these structures gave rise to the field of microneurosurgical anatomy.
One of the earliest clinical motivations for the Rhoton laboratory was the need for better facial nerve preservation during acoustic neuroma surgery (personal communication). The view through the operating microscope, along with all of the developments it inspired, made such difficult feats possible. This link between visualization and ability has been crucial in the history of surgery and continues to drive our field forward today, not only in the operating room, but also in the laboratory and the lecture hall. Both art and technology have played an important role in such progress.
The quest to understand visualization has occupied many of the brightest minds since antiquity. In ancient Greece, Plato and most other prominent thinkers believed that rays emitted from the eye mediated vision. Euclid (c. 300 bce ) combined this concept with his geometric principles into a theory of optics and vision whereby a cone of rays emitted from the eye traveled in straight lines to reach the subject. These rays were thought to reach out and interact with objects analogous to the sense of touch. Aristotle (c. 300 bce ) and others such as Avicenna (c. ce 1020) argued against emission of rays from the eye. Democritus (c. 400 bce ) and Epicurus (c. 300 bce ) proposed theories in which effigies of an object were received into the eye. Nonetheless, Plato’s ideas prevailed for more than a millennium to follow, not the least because they were also adopted by the influential Roman physician Galen (c. ce 175), who also incorporated the popular physiologic theory of pneuma. He believed that this vital substance originated within the cerebral ventricles and flowed through hollow optic nerves into a spherical lens located at the center of the eye, where it produced visualization with visual rays. Alhazen ( ce 965–1040), a renowned Arab mathematician and physicist considered to be the father of modern optics, was the first to successfully overturn the emission theory. Through empirical observation he deduced that vision occurs when light is reflected from an object into the eye, which then relays it to the brain. During the renaissance, the Flemish anatomist Vesalius began to identify errors in Galen’s writings through meticulous dissections. Felix Platter later gave a more detailed account of the anatomy of the eye in which the retina, rather than the lens, was considered to be the seat of vision. Johannes Kepler then explained how light rays passing through the lens could form an image on the retina, but it was still a mystery how this led to vision. Isaac Newton extended this theory by proposing that miniature vibrations within the retina were transmitted through the optic nerves to the brain, but a detailed physiologic understanding of visual processing beyond the retina did not emerge until the 20th century with the work of David Hubel and Torsten Wiesel.
Using prisms, Newton also proved that white light could be separated into component colors, which could then be mixed as desired. In the 19th century, scientists such as Thomas Young, Hermann von Helmholtz, and James Maxwell deduced that the eye contains three types of receptors with distinct color sensitivities—loosely related to red, green, and blue—that combined in various proportions to produce all perceived colors. In 1861 Maxwell demonstrated that a full color image could be reproduced with separate black and white photographs taken through red, green, and blue filters and then projected together with the corresponding filters. Their trichromatic theory of color vision greatly simplified the capture and reproduction of color images because the required ingredients—filters, film emulsions, inks, and emitters—would only be needed for three colors. To this day, whether in print or on a digital display, full color images can be reproduced from three single-colored images, just like Maxwell’s first color photograph.
Around the time that vision scientists were learning to reproduce color perception using three colors, Charles Wheatstone realized that two images from slightly different perspectives could reproduce the effect of viewing a scene through both eyes. He invented the first stereoscope in the early 1830s, concurrent with the early development of photography. It was a simple device that used mirrors to direct images with slightly different perspectives to each eye. Leonardo da Vinci and others before him had studied the phenomenon of binocular vision but never developed a stereoscopic viewer.
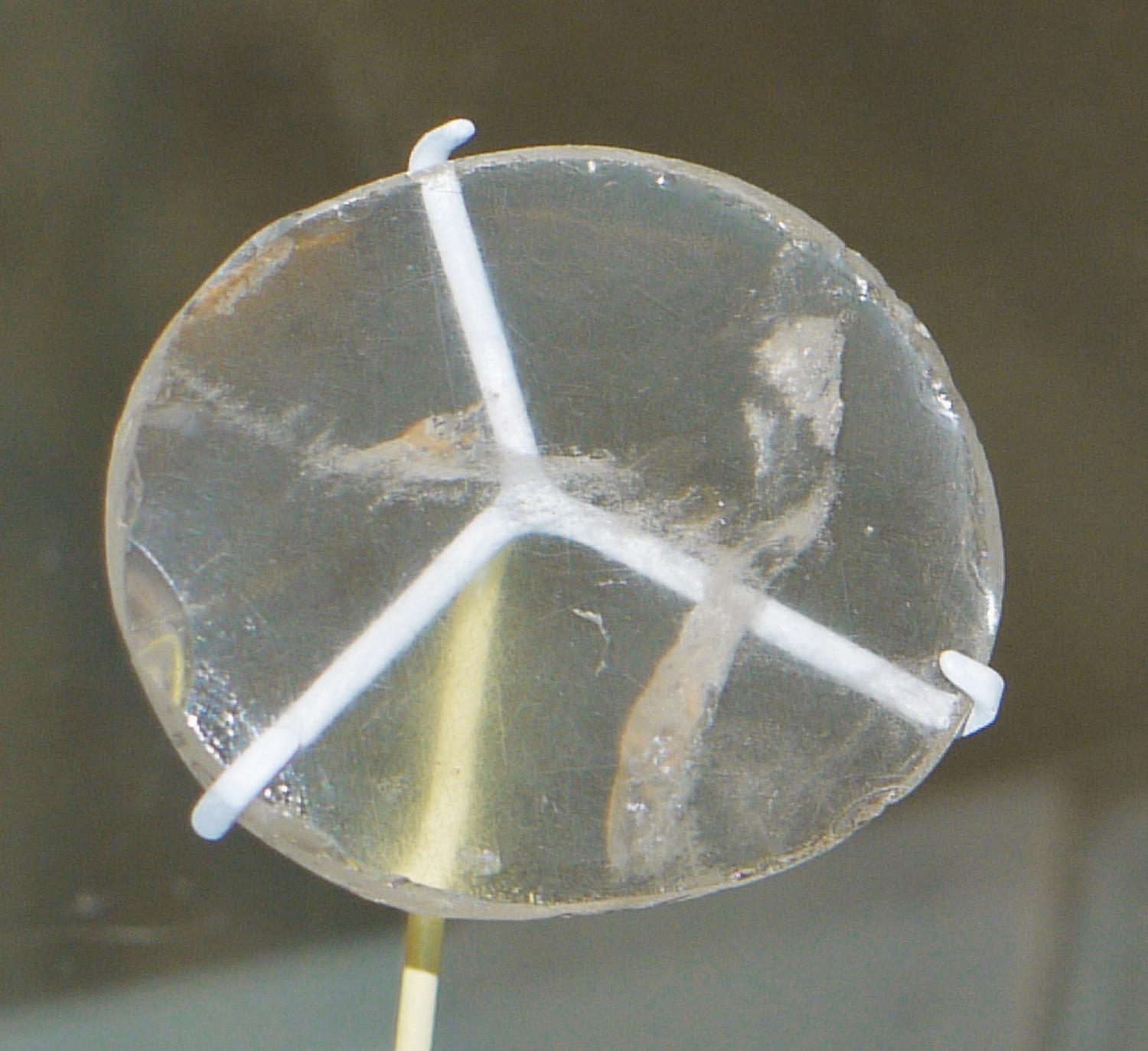
The use of lenses to magnify objects dates to antiquity. The oldest known lens, created about 750 bce , was found in the ruins of the ancient Assyrian city Nimrud, located in modern-day Iraq ( Fig. 31.1 ). Lenses found in Greek and Roman ruins are thought to have been used for both magnification and burning. In the first century, after the invention of glass, the Roman philosopher Seneca wrote, “Writing, however tiny and difficult, is seen larger and clearer through a glass sphere full of water.” Pliny wrote about cauterizing wounds with crystal balls using solar rays. If lenses were used as visual aids in the ancient world, it is a bit surprising that the invention of spectacles can only be traced as far back as 1286. Another 300 years passed before Dutch spectacle makers combined lenses in a tube to create the telescope and the compound microscope in the 1590s. The scientific utility of the microscope was recognized by Robert Hooke, who in 1665 was the first to use the term cell when describing the magnified appearance of cork in his publication “Micrographia.” Despite Hooke’s achievements, early compound microscopes still had serious technical problems in their design and manufacturing because lens making was still very much a trial-and-error process. In fact, for the remainder of the 17th century, compound microscopes were outperformed by the small single spherical lens microscopes of the self-taught Dutch biologist Anton van Leeuwenhoek, who kept his manufacturing process secret, giving him a near monopoly in the field of microbiology for the remainder of his life. He was the first to describe single-cell organisms. He also examined optic nerve tissue and failed to find the hollow conduits that Galen had described.
The first described use of a microscope within the operative theater was in 1686 by Giuseppe Campani, who used a compound microscope to examine wounds and scar tissue. Two more centuries would pass before the microscope was ready to assist with surgery. During that time, significant technical advancements were made in lens design in an attempt to overcome blurred images caused by several types of optical distortions. In 1730 the invention of the achromatic lens was the first step toward correcting chromatic aberration, which arises when the various colors of light in an image have different focal lengths because of a prism effect. This lens was composed of two layers of material with different refractive properties designed so that the chromatic aberration of the second material partially corrected that of the first. The problem was further reduced in 1868, when Ernst Abbe, a physicist hired by Carl Zeiss, developed an apochromatic lens using new materials. As the art and science of lens design and manufacturing progressed, so did the application of the microscope.
The use of magnification in surgery began in earnest in the second half of the 19th century with the development of loupe spectacles. It was not until 1921 that the microscope made it into the operating room when Carl Nylen, an otolaryngologist in Stockholm, first used a microscope during surgery for a case of chronic otitis media. His associate Gunnar Holmgren then took the initiative and developed the first binocular scope with an independent light source for use in otolaryngology. , Otolaryngologists continued to pioneer the use of the microscope in the operating room and improve on the design. As new limitations and problems became apparent, clever solutions were found. In 1938 a tripod with a counterweight system was used to further stabilize the magnified view. In addition, a prism was introduced that allowed for an observer scope to be used during the procedure.
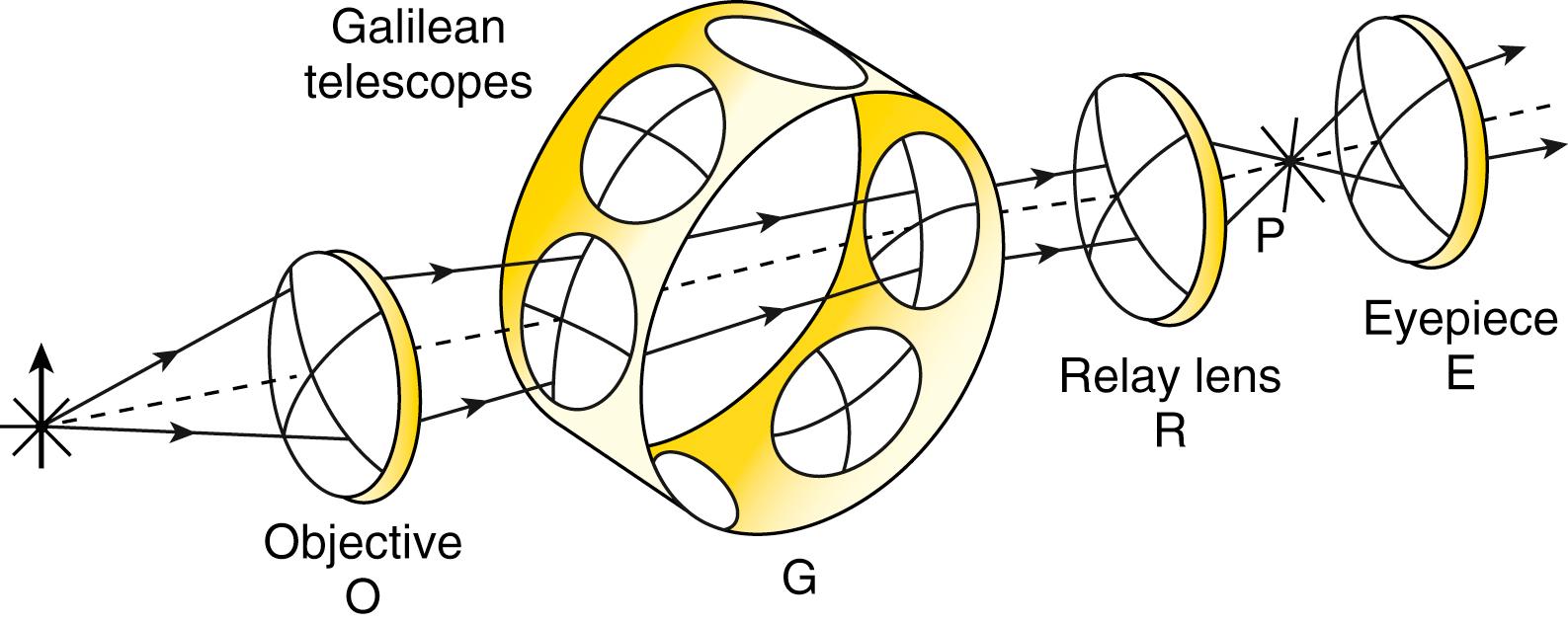
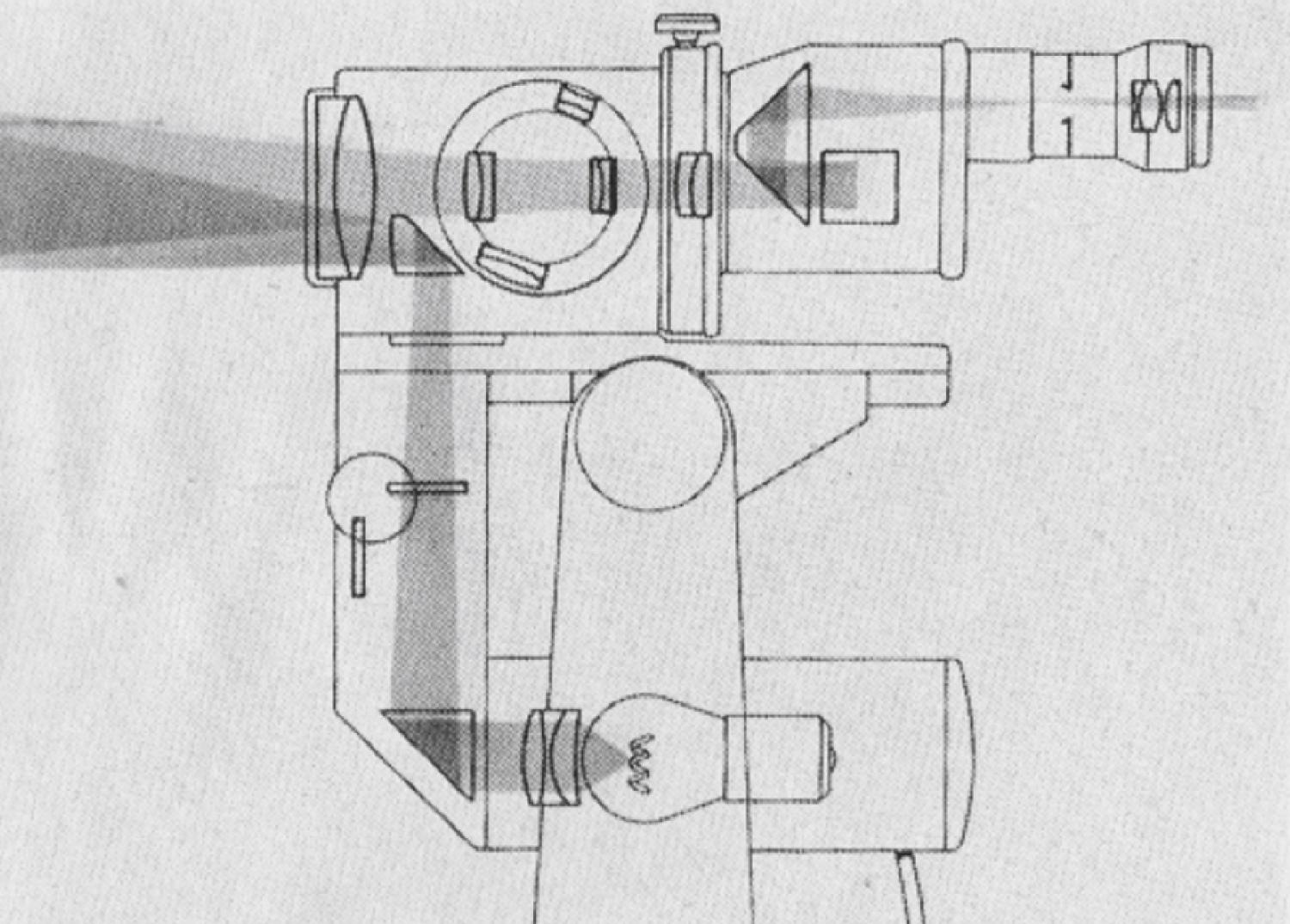
Throughout the early evolution of the operating microscope, the working distance and magnification of the image remained somewhat limited. In 1948 an ophthalmologist in Chicago used a Bausch & Lomb microscope with a 127-mm working distance and magnifications of 3, 5, 7, and 10.5, but changing settings required replacing the eyepieces used at the head of the microscope. This issue was solved through further innovation by Zeiss in 1952. Their new rotating Galilean system, developed by Hans Littman, allowed the user to change the magnification of the scope without replacing the eyepieces or changing the working distance. , The paired lenses around a rotating cylinder ( Fig. 31.2 ) allowed for a preset change in magnification. Zeiss began to market the new microscope as the OPMI 1 with rotating Galilean device, a rotating arm on a base with 100 to 405 mm of working distance, and 2.5 to 50 times magnification. The new OPMI 1 was designed for the operating room and had coaxial lighting that was superior to what had been used in previous models. Further advancements were soon made to allow for greater control and utility. , In 1956 foot and hand controls were developed for axial movement and image focus. By that time, axial lighting was widely used ( Fig. 31.3 ).
Despite the continued advancements and use of the operative microscope by otolaryngologists and ophthalmologists, neurosurgeons had yet to bring a microscope into the operating theater. This changed in 1957 when Theodor Kurze, a neurosurgeon at the University of Southern California, was inspired by the work of William House, who had been pioneering microsurgical techniques for otolaryngology. After practicing microsurgical techniques in the laboratory, Kurze performed the first microneurosurgical procedure: the excision of a seventh nerve (cranial nerve [CN] VII) neurilemmoma in a 5-year-old patient. , , At that time, sterile drapes for the operating microscope were not well developed, leaving surgeons to improvise with materials such as sterilized plastic turkey bags, which would sometimes overheat and produce smoke during the procedure. Kurze eventually performed a second procedure on his initial patient: a CN VII to CN XII nerve anastomosis. Unfortunately, the sterile drapes for the scope were not available at the start of the case, so Kurze proceeded without the microscope. On completion of the anastomosis, the drapes had become available, and he decided to evaluate his work with the microscope. He stated that the anastomosis “looked awful,” and then repaired the work with the aid of the microscope. Kurze continued using the operative microscope in his practice, even transporting the scope between facilities in the back of his personal vehicle.
Although Kurze was the first neurosurgeon to use the operative microscope, R.M.P. Donaghy quickly followed by establishing the first microsurgical research laboratory in Burlington, Vermont in 1958. Between Donaghy and his vascular surgery colleagues, the research laboratory was making important contributions by 1960, when they published the first use of the operative microscope for the anastomosis of small vessels. Before this work, vessels smaller than 7 to 8 mm could not be reliably repaired or joined. Also in 1960, Donaghy’s interest in surgical treatments for ischemic stroke led him to perform the first open middle cerebral artery embolectomy. Later in that year his vascular surgery colleagues, Jacobson and Suarez, published their findings from a collection of dog and rabbit carotid artery reanastamoses with a reported patency rate of 100%. Although this was an incredible development in microvascular technique, a prominent chairman of vascular surgery made the public critique that “[t]his is very nice work, but it is simply ridiculous to bring a microscope into the operating room.” Thus, as with most paradigm shifts, microsurgery was not universally embraced in the beginning.
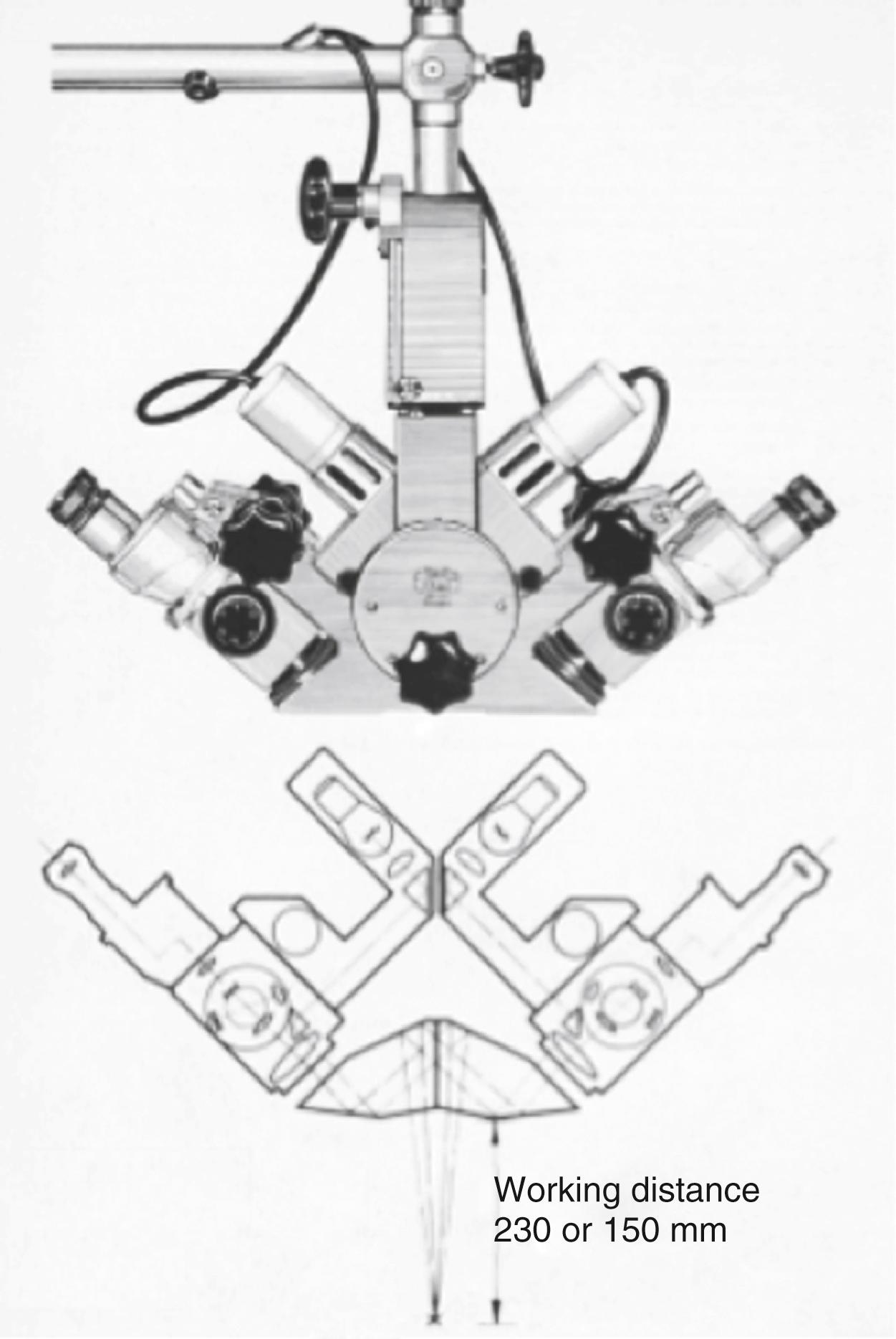
Despite the lukewarm reception, work with the microscope continued to progress. Kurze and House used the scope for more than 40 middle fossa explorations and published their experience in 1962. Kurze also used the microscope for aneurysm surgery starting in 1958, although the first to publish cases of microsurgery for aneurysms were Adams and Witt in 1964, and Pool in 1965. Also in 1965, Sais, a company from Buenos Aires, fitted a television camera on the observer head of the scope, allowing for recording and broadcasting. This was built on the advancements made by Zeiss with the 1961 release of the diploscope—a “true double microscope” for head-to-head work by two surgeons ( Fig. 31.4 ). , In the same year, Zeiss released a motorized focus and zoom feature that replaced the rotating Galilean system.
In 1966 a young Turkish neurosurgeon with an interest in vascular microsurgery arrived in Burlington. In Donaghy’s laboratory, M.G. Yaşargil developed the superficial temporal–middle cerebral artery bypass procedure. Yaşargil eventually returned to Zurich, where he was the first to perform this procedure on a human patient. Coincidentally, Donaghy repeated this feat less than 24 hours later in Vermont. Yaşargil went on to help pioneer several technical advancements, such as the ability to manually tilt the microscope head (1970) and a polyaxial counterweight system with electromagnetic braking for each joint (1972), to make the operating microscope more graceful. , These user-friendly features spurred wider adoption of the operating microscope and stimulated further industry-wide development. Modern advancements have seen improvements in optical technology, including clearer apochromatic lenses, automatic focus, increased depth of field, and more powerful motorized zoom ( Fig 31.5 ). Intraoperative angiography with indocyanine green fluorescence and the use of 5-aminolevulinic acid for high-grade glioma resection have been incorporated into several microscopes. Stereoscopic video recording and stereotactic guidance have now become widely available.
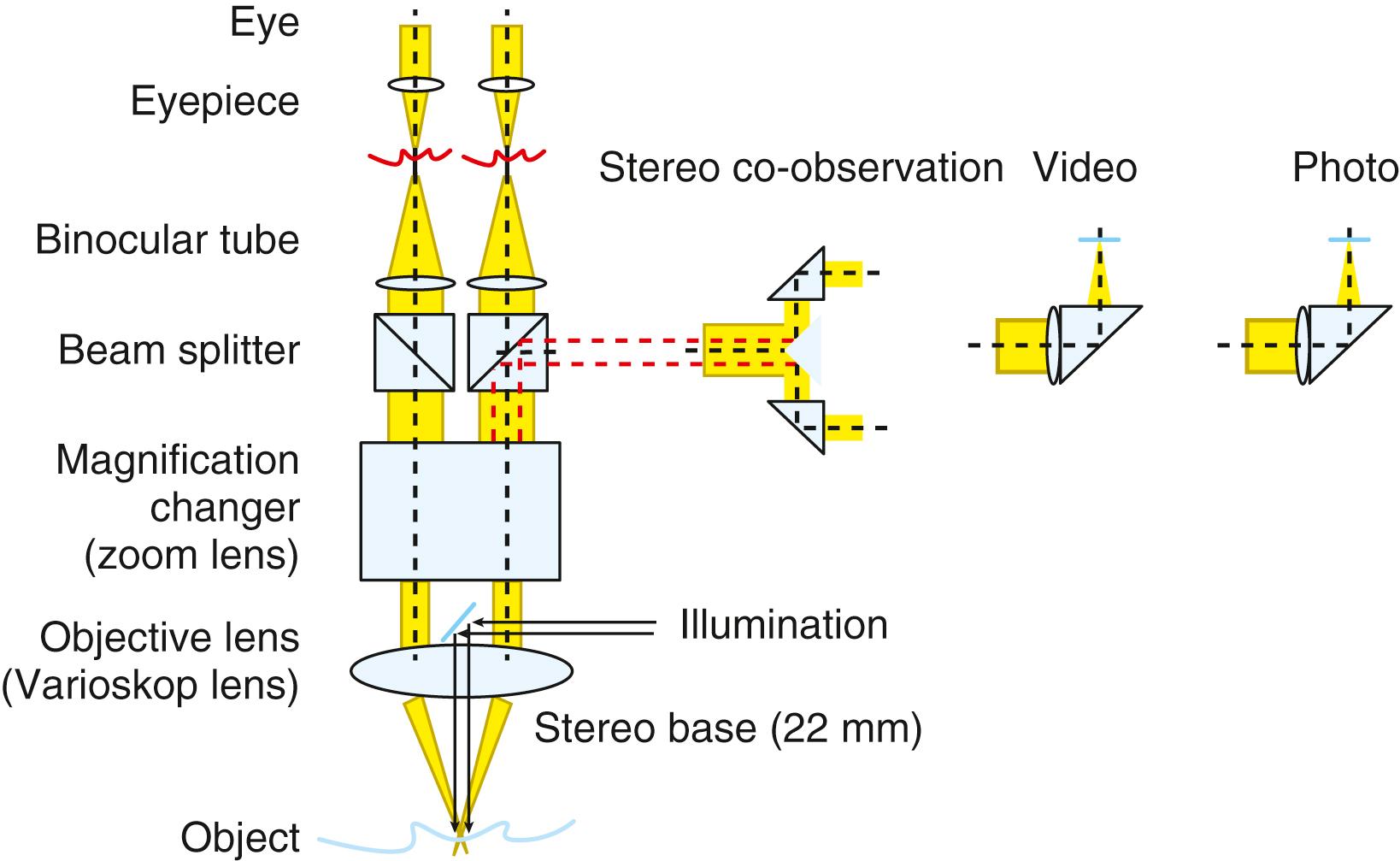
For most neurosurgical procedures, the microscope’s advantage is threefold. Magnification and focused illumination are crucial to appreciate the intricate details of the small neural and vascular structures of the nervous system. However, the enhanced stereoscopic perspective is really the major advancement the microscope has brought to surgical specialties. This helps neurosurgeons preserve binocular vision, and thus depth perception, in a deep narrow field. In fact, the microscope, through its refractory mechanisms, decreases the interpupillary distance required to maintain binocular vision in restricted depths. Such an advantage cannot be fully reproduced with simple surgical loops and a headlamp. For Yaşargil, the stereoscopic perspective of the microscope is one of the major foundations of modern micro-neurosurgery, as it facilitates navigation through the fissures of the brain and skull base corridors to reach deeper structures while minimizing unnecessary injury to the surrounding brain. Modern microsurgical approaches have thus evolved to take advantage of the operating microscope. The microscope’s mobility permits constant movement of its “visual cone” and corresponding funnel-shaped working field that is limited primarily by the surgical approach. The latter can be widened by gently retracting the brain, releasing cerebrospinal fluid, drilling the skull base, and mobilizing nerves and vessels.
Although often viewed as a modern tool, the endoscope has a longer history in the operating room than the microscope. Precursors such as the lighted speculum of Philipp Bozzini had been in use since 1806, but the field of endoscopic surgery began in 1887 with the German urologist Max Nitze, who co-invented the first operating endoscope. This device had a series of lenses within a hollow tube with a water-cooled electric lighting filament at the tip. These early endoscopes had fairly poor optics and maneuverability, so widespread adoption by gastroenterologists did not occur until the prominent British optical physicist Harold Hopkins, creator of the first viable zoom lens, developed a fiberoptic flexible endoscope in the 1950s. This allowed much more complete examinations of the gastrointestinal tract. Nonetheless, the fiberoptic scopes had resolutions that were limited by the number of fibers, which produced a pixilated image. Hopkins therefore went on to develop the rod-lens endoscope in 1959, which used a series of rod-shaped lenses with small gaps between them. This resulted in substantially better optics and smaller diameters than the previous rigid scopes used by Nitze. Karl Storz then added fiberoptic lighting to the rod-lens scopes. After urology and gastroenterology, otolaryngologists were early adopters of endoscopy. The first neurosurgical applications included coagulation of the choroid plexus for hydrocephalus, third ventriculostomy, and pituitary surgery, but neurosurgical endoscopy did not begin to blossom until the 1990s. Currently the field of skull base surgery is being redeveloped with endoscopic techniques. The endoscope provides neurosurgeons new perspectives, but like the operating microscope, it requires the development of new instruments and techniques. Because of their superior optics, rigid endoscopes still dominate in neurosurgery, but one day flexible endoscopes may allow us to work more effectively around corners, which could fundamentally alter our approaches to some neurosurgical lesions.
It is likely that the operating microscope will continue to evolve from a simple optical pathway into a hybrid optical-digital device because the laws of physics place hard limits on the quality of imaging that can be accomplished through pure optics. For instance, increased aperture size allows for better illumination but decreases the depth of field. In surgical microscopes, much emphasis has been placed on improving image magnification and illumination. When this is achieved through additional lenses, wider apertures, and brighter light sources, there can be detrimental effects, such as reduced depth of field and thermal injury to tissues. With continued improvements in computing power and charge-coupled device sensors, digital microscopes may provide alternative solutions for these challenges. New technologies will undoubtedly emerge, but a few techniques for increased dynamic range of contrast and increased depth of field that are already common in digital photography might be adapted. Digital microscopes will ultimately allow enhanced magnification, illumination, image quality, and intraoperative annotation.
Video telescopic intraoperative microscopes, or exoscopes, have been gaining popularity among neurosurgeons owing to their multifold advantages. The microscopic image is projected onto a screen outside the surgical field, allowing more extreme angles of visualization, with reduced ergonomic discomfort to the surgeon. These devices have also been showing promise for enhanced magnification, illumination, image quality, and educational value.
The high-definition three-dimensional (3D) digital image has further allowed its modern incorporation into routine spinal and cranial procedures, with surgical results similar to those with the operative microscope. , This new technology is also facilitating additional applications of robotic assistance in neurosurgical procedures. However, a key challenge remains the lack of stereoscopic vision, and thus depth perception, as provided by the traditional microscope.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here