Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since its emergence in the late 1980s, computer-assisted surgery (CAS) has become an increasingly important adjunct to craniofacial reconstruction. The refinement of virtual surgical planning (VSP) coupled with the availability of 3-dimensional (3D) printing techniques has enabled easier and more predictable remodeling of the craniofacial skeleton. As these techniques continue to develop, they point to a future in which ever more elaborate craniofacial challenges can be tackled with more secure outcomes. In this chapter we discuss the utility of CAS techniques for primary and secondary trauma reconstruction and then consider the future of these approaches in craniofacial surgery.
The groundwork for contemporary CAS was established in the 1980s with the proliferation of CT scanning and the advent of computer-aided design and manufacturing (CAD/CAM) methods. By enabling noninvasive, 3-dimensional visualization of the craniofacial skeleton, the former enabled much more accurate preoperative diagnosis and planning than was available from plain radiographs. Utilization of CAD/CAM in turn allowed that preoperative plan to be translated into adjuncts for surgery such as patient-specific cutting guides and implants. The integration of these techniques into a unified computer-assisted craniofacial surgery was first described by Toth et al. in 1988. These authors generated patient-specific resin molds which were then used preoperatively to shape prosthetic implants and intraoperatively to guide bone shaping in a series of patients needing frontoorbital reconstruction. The subsequent revolution in digital image manipulation allowed this pioneering approach to be much more widely adopted.
Currently CAS techniques are commonly used in elective craniofacial and orthognathic surgery as well as in craniofacial trauma reconstruction. The utility of these approaches has been widely chronicled in the literature. Some of the broad categories of applications include VSP of osteotomies, segmental bone movements or reductions, virtual correction of occlusion, generation of customized cutting guides, and creation of patient-specific implants. These applications largely share a common workflow: (1) acquisition of high resolution CT images of the craniofacial skeleton; (2) conversion of these images to DICOM file format for use in digital image manipulation; (3) creation of 3D reconstructions of the craniofacial skeleton by a bioengineering company; (4) VSP teleconference between surgeons and biomedical engineers to discuss surgical plans; (5) creation of patient-specific implants, models, or cutting guides. Completion of this workflow can be accomplished in a week or less and has been shown to be cost-effective when considering its acceleration of operative times. We next illustrate the use of CAS in primary and secondary trauma reconstruction.
Utilization of CAS in primary craniofacial trauma reconstruction presents some challenges. The time required to complete CAS workflow may limit its utilization, though this process is becoming ever more expeditious. In general we advocate early treatment of facial fractures in order to achieve the most anatomic repairs and to minimize unfavorable scarring and soft tissue contraction. However, in the severely injured trauma patient, where CAS techniques are most useful, there is often time between initial stabilization of injuries to other body systems and definitive repair of craniofacial injuries. Advantages of CAS in these situations include minimization of dissection and more accurate repairs through the use of pre-bent plates and cutting guides. These benefits are particularly valuable in severe craniofacial injuries in which multilevel trauma and comminution can disrupt normal anatomic relationships that guide repair. We present an example in which CAS proved valuable in reconstruction of the mandible.
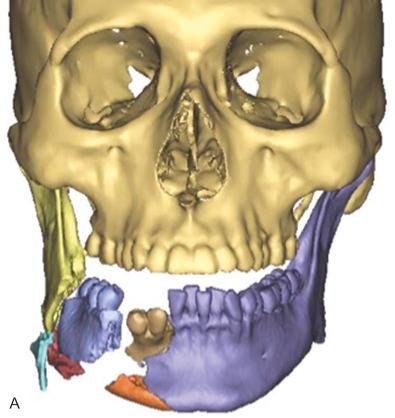
We used CAS techniques to virtually reduce a severely comminuted mandible fracture following a blast injury ( Fig. 3.14.1 ). The patient was involved in a chemical explosion at work and suffered injuries to his lower face including degloving of skin and soft tissues of the right cheek and open fractures of the right mandibular body and parasymphyseal region with significant comminution. After primary stabilization and placement of a tracheostomy at the regional burn center, the patient was transferred to our care for management of his facial injuries. The numerous fragments of mandibular bone – some of marginal viability – made accurate anatomical reduction challenging. Proper reduction and fixation was further complicated by the need to minimize additional soft tissue dissection for fear of compromising blood supply to the bone. For these reasons, we conducted a VSP planning session in which major fragments were brought into alignment virtually. Additionally, proper occlusion was established in this forum and used to guide design of a pre-bent reconstruction plate spanning the aligned fragments. This plate was milled and shipped to our center in 5 days. Intraoperatively, the patient's existing traumatic lacerations were extended and conservative debridement of clearly nonviable soft tissue and bone was performed. After simplification of smaller fracture fragments through a combination of bridle wiring and 1 mm superior border plates, the patient was placed in maxillomandibular fixation using Erich arch bars and elastics. These were secured to major fracture fragments with bone reduction forceps and digital manipulation. The custom plate was then readily adapted to the reduced mandible and secured using locking screws. The patient has gone on to heal with restoration of premorbid occlusion at his most recent 2-month follow-up.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here