Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Aneurysms are abnormal dilations of blood vessels and occur most commonly in arteries. Venous aneurysms are rare but have been reported throughout the veins in the body, including the extremities, head and neck, and abdomen.
When defining venous aneurysms, Gillespie et al. state: “The definition of a venous aneurysm has been controversial. A venous aneurysm is best described as a solitary area of venous dilation that communicates with a main venous structure by a single channel, and it must have no association with an arteriovenous communication or a pseudoaneurysm. Most importantly, it should not be contained within a segment of a varicose vein.” In general, venous aneurysms can be defined as an area of dilation 2 to 3 times the surrounding normal vein. , They are rare and generally asymptomatic; thus, the true incidence is unknown.
Venous aneurysms can be classified as primary (congenital) or secondary (acquired). Primary aneurysms are caused by a weakness in the venous wall secondary to inherited conditions such as Klippel–Trénaunay syndrome, neurofibromatosis 1 (NF-1), and Parkes Weber syndrome (discussed more fully in Chapter 171 , Congenital Vascular Malformations: Surgical Management). Secondary venous aneurysms arise from etiologies such as trauma, inflammation, degenerative processes, mechanical stress, and venous hypertension. Some case reports describe a correlation between pregnancy and venous aneurysm formation, but no causative factors have been elucidated. Scientific publications identify the presence of estrogen receptors in venous vascular tissue, and although it is tempting to hypothesize causality, this has not been established.
Histologically, the intima of venous aneurysms may be thickened and fibrosed. In addition, the media may be attenuated or absent and display a paucity or total lack of smooth muscle cells. Matrix metalloproteinases (MMPs) have been noted to be expressed at higher levels in venous aneurysms compared with normal venous tissue. The established relationship between MMPs and arterial aneurysms is long standing, but more research is needed to document this relationship in venous aneurysms.
Clinically, patients with venous aneurysms are usually asymptomatic; however, complications can occur and include thrombosis, embolization, rupture, local mass effects with or without edema, and localized pain or tenderness. Diagnosis may be made with physical examination in the case of superficial venous aneurysms; however, they are often misdiagnosed as soft tissue masses or even hernias. Diagnostic confirmation can be performed using duplex ultrasound (DUS), computed tomography, or magnetic resonance imaging. Venography is not indicated for primary diagnosis. A thorough history should be elicited from the patient, specifically inquiring about family history of aneurysmal or connective tissue disease and any recent or remote trauma to the region. In addition, physical examination should identify any sequela of arteriovenous fistula, with imaging studies performed if needed.
Treatment of venous aneurysms is performed on a case-by-case basis because there are few evidence-based studies to guide treatment. In general, conservative management is indicated for small and/or asymptomatic aneurysms. Surgical treatment for large aneurysms or those associated with complications consists of tangential aneurysmectomy, aneurysm resection with primary anastomosis, aneurysm resection with interposition grafting, or ligation of the affected venous segment. There is no standard endovascular treatment, but endovascular modalities have been successfully implemented in select patients.
Superficial venous aneurysms are usually visible and present as painless masses, often misdiagnosed as soft tissue masses. Depending on the location, these aneurysms can be confused with hygromas, or even inguinal or femoral hernias. Thorough physical examination may identify a superficial venous aneurysm because the mass is more resistant to compression in the dependent position compared with when the extremity is elevated. DUS can definitively make the diagnosis. Saphenous vein aneurysms have been diagnosed during operative procedures for what were thought to be varicose veins preoperatively. Venous aneurysms on the dorsum of the foot have been described and are usually asymptomatic. Interestingly, all case reports of pedal venous aneurysms involve young women.
Treatment of superficial venous aneurysms involves ligation and excision after ensuring that the deep venous system is intact. If the aneurysm is near the saphenofemoral junction, traditionally a high ligation should also be performed. Hamman et al. described their experience with endovenous thermal ablation of incompetent saphenous veins with associated aneurysms. They treated 15 limbs in 13 patients who had saphenous vein aneuryms within 20 mm of the saphenofemoral or saphenopopliteal junction. Venous segments were considered aneurysmal if they were greater than 20 mm in the greater saphenous vein and greater than 15 mm in the small saphenous vein. High ligation was concomitantly performed if the aneurysms were greater than 30 mm in greatest dimension. The authors reported no instances of endovenous heat-induced thrombosis class 2–4, deep vein thrombosis, or pulmonary embolism.
Aneurysms of perforating veins in the lower extremity have been described only rarely. This may be secondary to the lack of specific symptoms. Ultrasound is diagnostic when the size of the perforating venous aneurysms exceeds 9 mm. Although these aneurysms are located below the deep fascia, they are included in the superficial venous aneurysm section because they are often treated the same way superficial refluxing veins are treated – subfascial ligation with or without aneurysm excision. Aneurysms are excised if they are symptomatic. Labropolous et al. also noted that these aneurysms are usually fusiform and recommended treatment if perforating vein treatment was undertaken. That group found no relation between the sizes of perforating vein aneurysms and the severity of chronic venous disease.
Popliteal venous aneurysms ( Fig. 166.1 ) are the most commonly reported and best studied of all venous aneurysms. Evidence from previous studies suggests that popliteal venous aneurysms are more commonly associated with complications than aneurysms in the superficial system. These complications include thrombosis, pulmonary embolism, localized pain and swelling, more diffuse lower extremity swelling, and symptoms of chronic venous disease. In one of the largest case series, 24 cases of popliteal venous aneurysm were identified; all patients presented with thromboembolic disease. Seventy-one percent presented with pulmonary embolism. Other studies have shown that most popliteal venous aneurysms (45%–80%) are discovered incidentally during work-up after patients have suffered a pulmonary embolism. ,
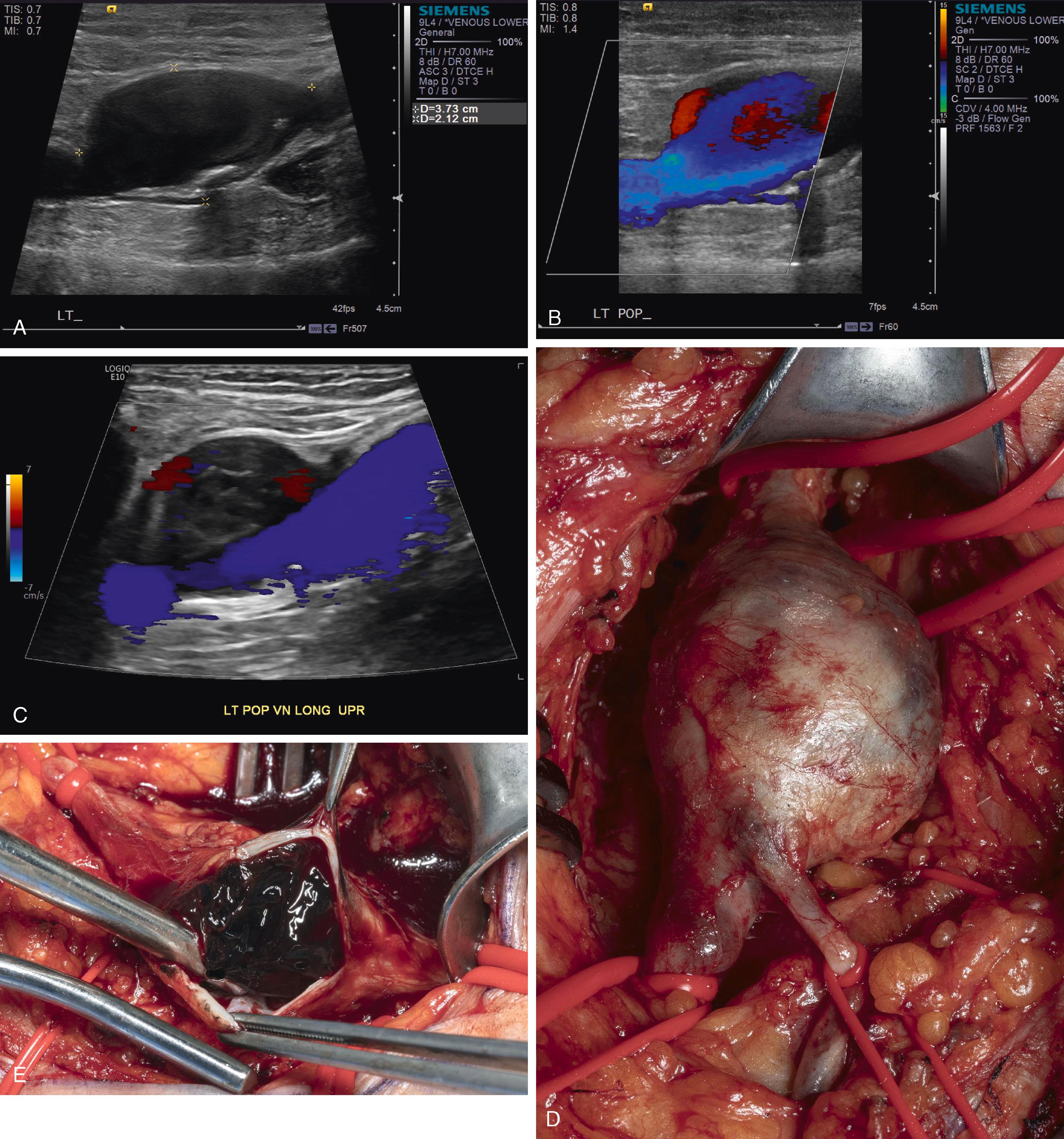
Noppeney et al. described their retrospective analysis of 39 patients treated for popliteal venous aneurysms from 1992 to 2018. Their treatment algorithm consisted of evaluation for popliteal venous aneurysm size and turbulent flow within the aneurysm sac. Generally, patients with aneurysms larger than 20 mm also had turbulent flow and thus were offered resection. There were 4 of 29 patients who did not have turbulent flow in an aneurysm greater than 20 mm. These were noted to be stable without evidence of thrombus formation during the surveillance period. Patients with aneurysms less than 20 mm were split evenly between those with turbulent flow ( n = 5) and those without turbulent flow ( n = 5). All 5 patients with turbulent flow and 1 patient without turbulent flow (patient preference) were reconstructed. The 4 patients without turbulent flow were noted to have stable aneurysm size without evidence of thrombus during the surveillance period.
Asymptomatic patients with aneurysms less than 20 mm can be serially monitored with ultrasound to evaluate for progression. Symptomatic patients, particularly those who have suffered a pulmonary embolus, should be treated regardless of aneurysm size. Anticoagulation alone is not considered sufficient treatment for popliteal venous aneurysms. Patients can develop thrombus when therapeutically anticoagulated even when no thrombus was identified on initial diagnosis. Thrombus burden localized to the popliteal venous aneurysm has been shown to predispose to pulmonary embolus even when patients are therapeutically anticoagulated. , Surgical reconstruction is preferred in these cases and consists of tangential aneurysmectomy with lateral venorrhaphy, aneurysm resection with primary anastomosis, interposition grafting with saphenous vein, or spiral saphenous vein interposition grafting. If no other option is available, a synthetic bypass can be used, but postoperative thrombosis is more common. Tangential aneurysmectomy with lateral venorrhaphy ( Fig. 166.2 ) is the preferred method of reconstruction. Inferior vena cava (IVC) filter placement and catheter-directed lysis should be considered on a case-by-case basis, taking into account patient-specific variables such as ability to tolerate anticoagulation and concomitant extent of ipsilateral deep venous thrombosis. Patients are routinely placed on anticoagulation for 3 to 6 months after all procedures.
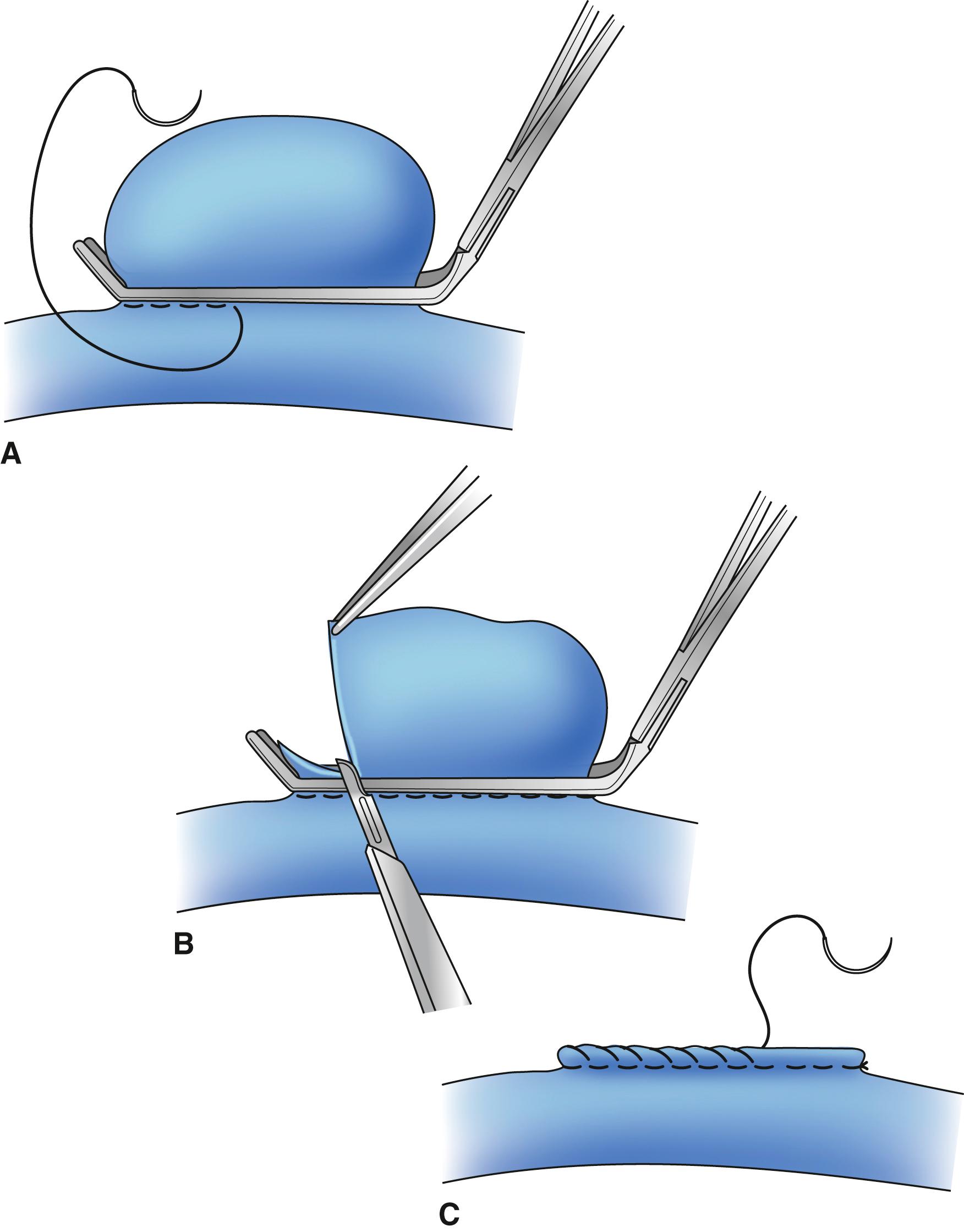
Another method for popliteal venous aneurysm repair is described by Beaulieu et al. Closed plication of the aneurysm is accomplished by tangential plication with pledgeted suture. This method was performed in nine patients with reasonable outcomes. The benefits include no routine postoperative anticoagulation and avoiding the need for proximal and distal control of the aneurysm. Limitations include contraindication in the setting of mural thrombus and the utilization of prosthetic material (pledget). The authors did not experience a deep surgical site infection in their series.
Due to their rarity, few studies exist to guide the treatment of femoral and common femoral venous aneurysms. We believe that, extrapolating from the popliteal venous aneurysm literature, symptomatic aneurysms should be treated surgically and asymptomatic venous aneurysms can be monitored for increase in size and/or development of intraluminal thrombus if they are small on discovery.
Iliac vein aneurysms are rare. Rupture was reported in one case of a large external iliac vein aneurysm. More commonly these aneurysms are asymptomatic and discovered incidentally or during evaluation for other pathology such as pulmonary embolism. Zarrintan et al. performed a review of 50 iliac vein aneurysms in the literature. Gender differences were noted in presentation with men more commonly presenting with limb swelling or pain (41.9%) and venous insufficiency (12.9%), while women were most commonly asymptomatic (35.3%). Males also tended to present with a history of trauma (12.9%) while women had a higher prevalence of associated May–Thurner syndrome. The authors also noted a higher incidence of aneurysms found on the left side and more commonly in the external iliac vein followed by the common iliac vein.
Treatment is best accomplished with tangential aneurysmectomy and lateral venorrhaphy. Ligation of the iliac vein leads to a high rate of chronic lower extremity edema and post-thrombotic syndrome and should be avoided. Aneurysms associated with arteriovenous fistula are likely best managed with covered stenting of the arterial system followed by venous aneurysm resection.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here