Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chronic venous diseases include a spectrum of clinical findings ranging from spider telangiectasias and varicose veins to debilitating venous ulceration. Varicose veins without skin changes are present in about 20% of the general population, and they are slightly more frequent in women.
References to varicose veins are found in early Egyptian and Greek writings and confirm that venous disease was recognized in ancient times. A votive tablet in the National Museum in Athens showing a man holding an enlarged leg with a varicose vein is frequently featured in many historical writings regarding venous disease.
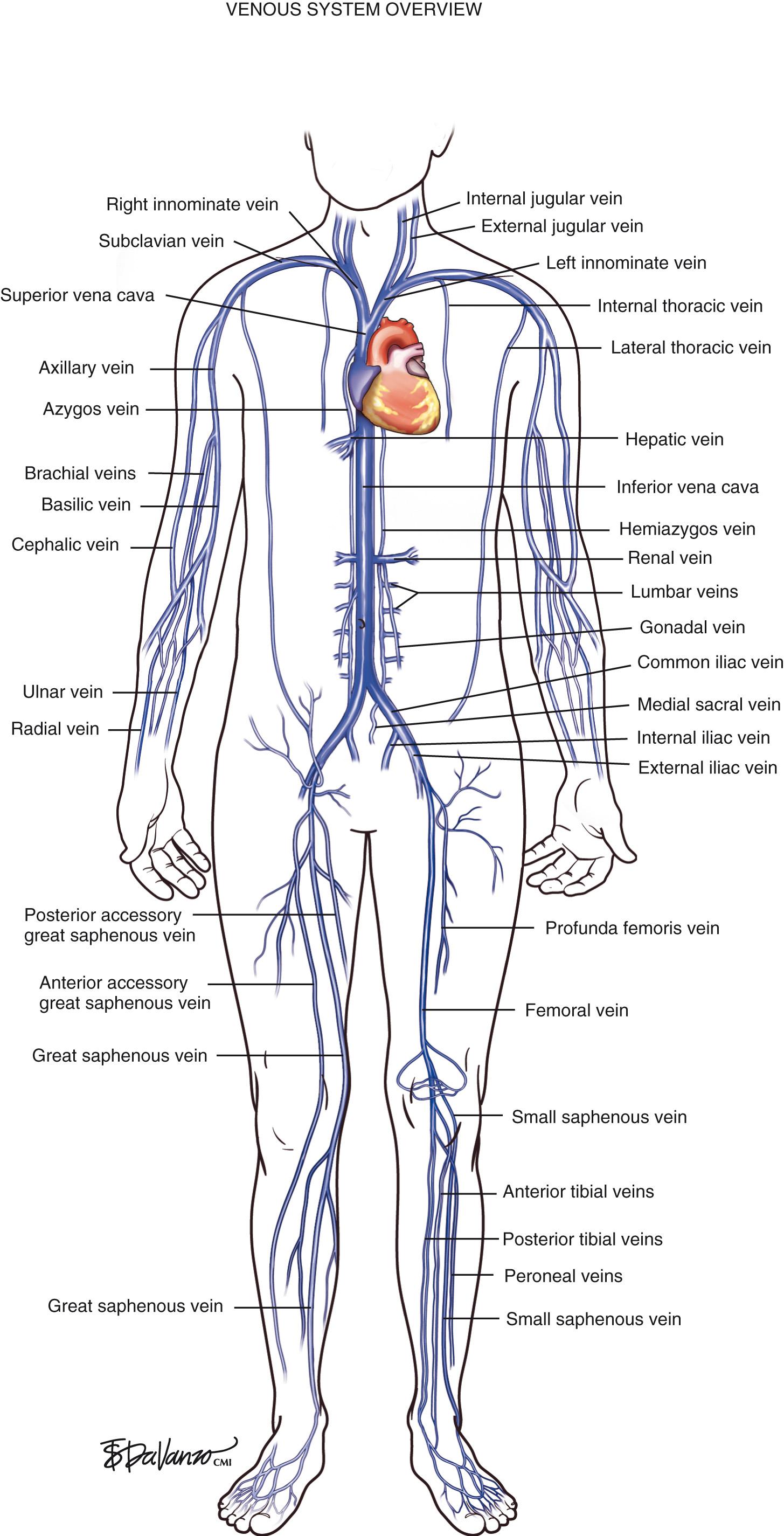
The venous system originates at the capillary level and progressively increases in size as the conduits move proximally toward the heart. The venules are the smallest structures, and the vena cava is the largest. It is critical that all endovascular venous surgeons understand the anatomic relationships between the thoracic, abdominal, and extremity venous systems, especially from the anatomic standpoint ( Fig. 1.1 ). Veins of the lower extremities are the most germane to this book and are divided into three systems: deep, superficial, and perforating. Lower extremity veins are located in two compartments: deep and superficial. The deep compartment is bounded by the muscular fascia. The superficial compartment is bounded below by the muscular fascia and above by the dermis. The term perforating veins is reserved for veins that perforate the muscular fascia and connect superficial veins with deep veins. The term communicating veins is used to describe veins that connect with other veins of the same compartment.
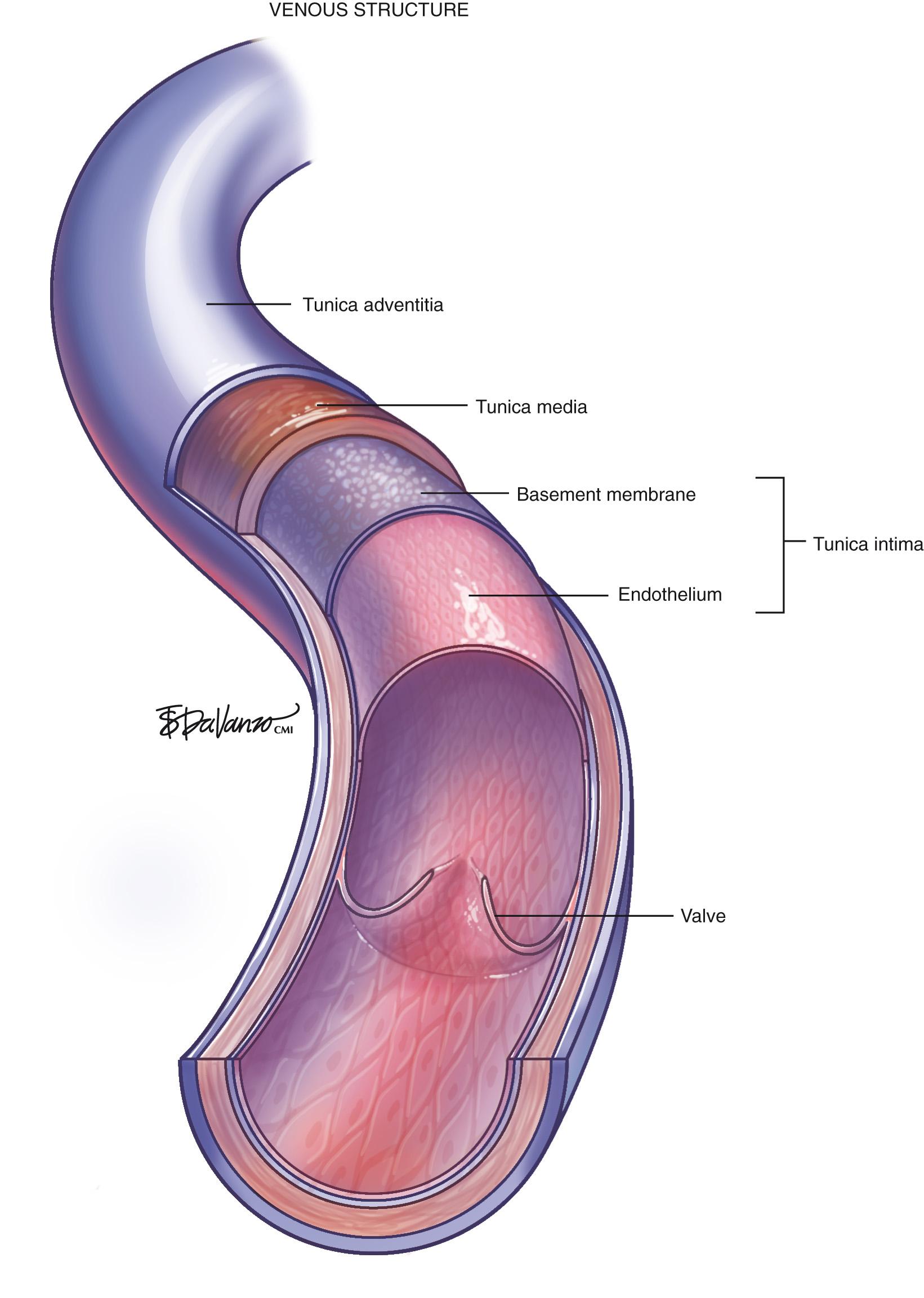
The vein wall is composed of three layers: intima, media, and adventitia. Notably, the muscular tunica media is much thinner in a vein than in a pressurized artery. Venous valves are an extension of the intimal layer, have a bicuspid structure, and support unidirectional flow ( Fig. 1.2 ).
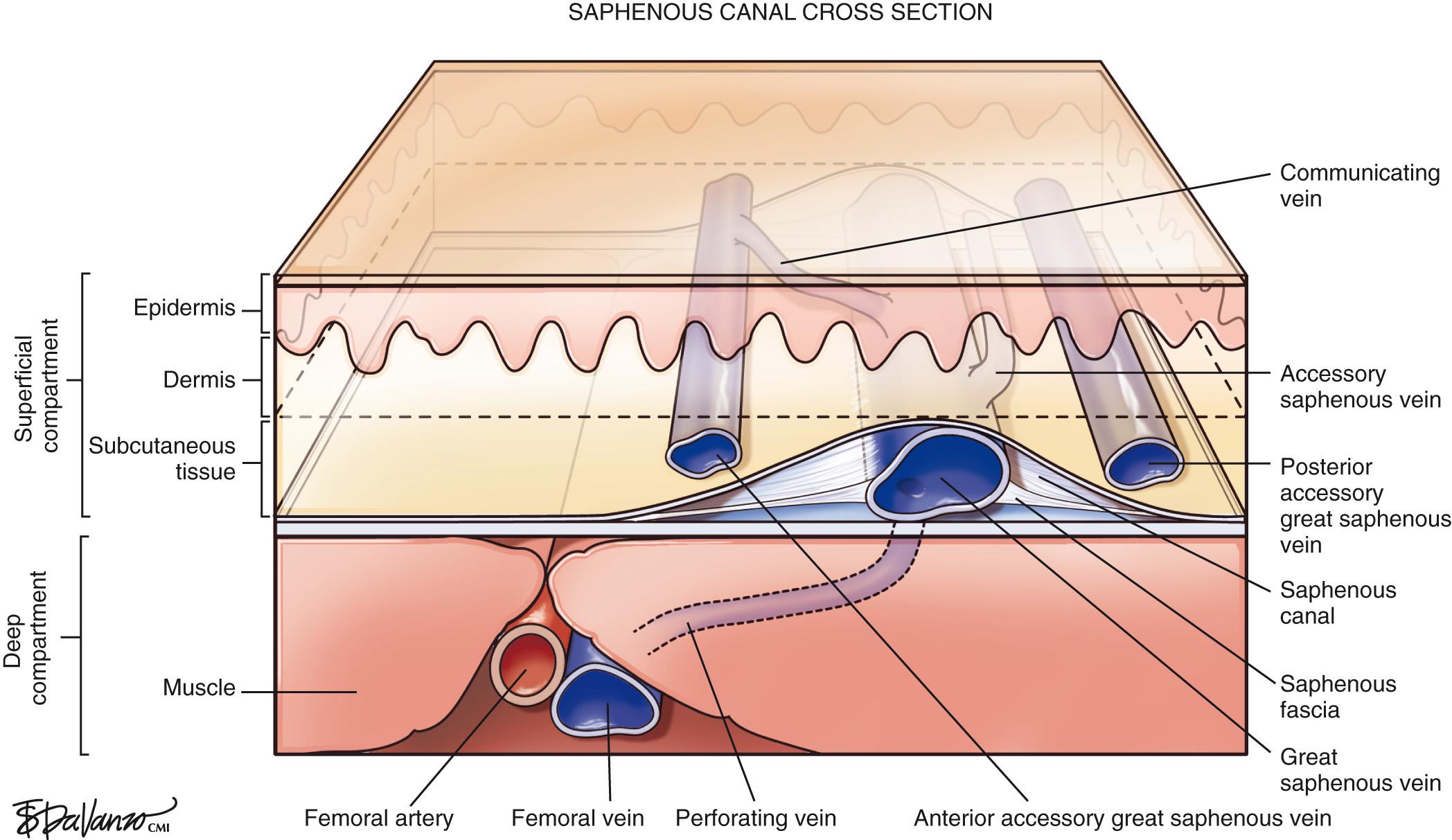
Surgeons who perform thermal or chemical ablation therapy of the great saphenous vein (GSV) and its related structures must have a good understanding of the saphenous canal. The importance of the saphenous canal in relation to B-mode ultrasound anatomy is detailed in Chapter 4 . A cross section of the saphenous canal ( Fig. 1.3 ) depicts many of the critical relationships referable to GSV treatment; the most important is how it courses atop the muscular fascia in a quasi-envelope called the saphenous fascia . The saphenous fascia is the portion of the membranous layer of the subcutaneous tissue that overlies the saphenous veins. Veins coursing parallel to the saphenous canal are termed accessory veins ; those coursing oblique to the canal are called circumflex veins . Compressible structures superficial to the muscular fascia are potential targets for treatment, but treating those structures deep to the muscular fascia may lead to a disastrous outcome. Noncompressible structures generally represent major arteries. Perforating veins must pierce the muscular fascia as they drain blood from the superficial to deep systems.
As diagnostic and therapeutic options for venous disorders expanded, the nomenclature proposed in 2002 by the International Interdisciplinary Committee required revision. The nomenclature was extended and further refined, taking into account recent improvements in ultrasound and clinical surgical anatomy. The term great saphenous vein should be used instead of terms such as long saphenous vein, greater saphenous vein, or internal saphenous vein . The LSV abbreviation, used to describe both the long saphenous vein and lesser saphenous vein , was clearly problematic. For this reason, these terms have been eliminated. Similarly, the term small saphenous vein, abbreviated as SSV, should be used instead of the terms short, external , or lesser saphenous vein .
The GSV originates at the medial foot and receives deep pedal tributaries as it courses to the medial malleolus. From the medial ankle, the GSV ascends anteromedially within the calf and continues a medial course to the knee and into the thigh. The termination point of the GSV into the common femoral vein is a confluence called the saphenofemoral junction (SFJ) ( Fig. 1.4 ).
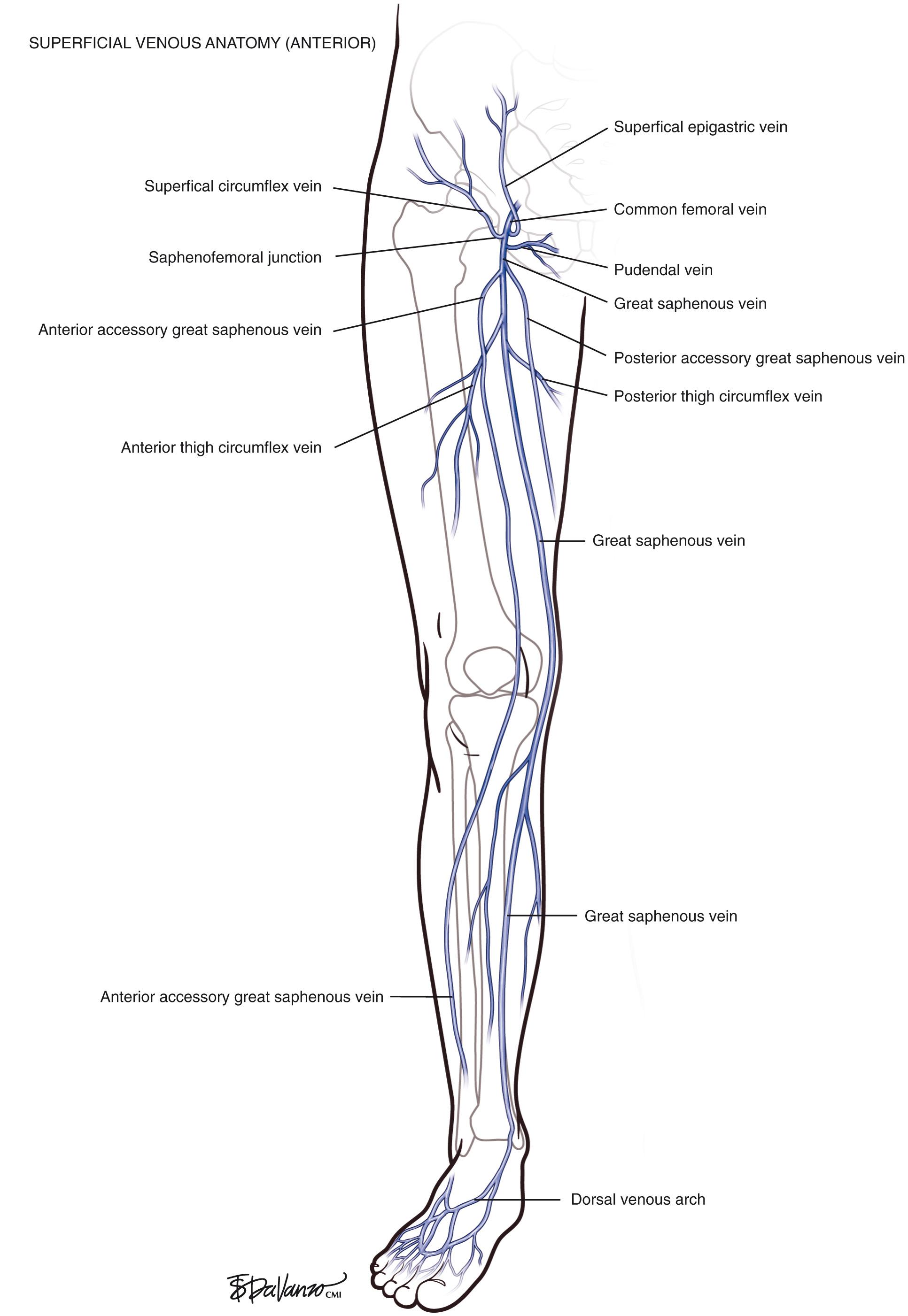
The terminal valve of the GSV is located within the junction itself. A subterminal valve can often be identified approximately 1 cm distal to the terminal valve. From the upper calf to the groin, the GSV is usually contained within the saphenous compartment. Visualization of this fascial envelope is an important landmark in identifying the GSV with duplex ultrasound. The saphenous compartment is bounded superficially by a hyperechoic saphenous fascia and deeply by the muscular fascia of the limb.
At the groin, the GSV drains blood from the external pudendal, superficial epigastric, and external circumflex iliac veins just before it enters the common femoral vein confluence. As in all human anatomy, variations are crucial to recognize, to guide the correct diagnosis and treatment. Historically, the GSV has been reported to be duplicated in the thigh in as many as 20% of subjects. However, recent examinations have demonstrated that true duplication, with two veins within one saphenous compartment, occurs in less than 1% of cases. Large extrafascial veins, which are termed accessory saphenous veins , can run parallel to the GSV and take on the characteristics of duplicated veins.
The accessory saphenous veins are venous segments that ascend in a plane parallel to the saphenous veins. They may be anterior, posterior, or superficial to the main trunk. The term anterior accessory great saphenous vein describes any venous segment ascending parallel to the GSV and located anteriorly, both in the leg and in the thigh. The term posterior accessory great saphenous vein (PAGSV) is consistent with any venous segment ascending parallel to the GSV and located posteriorly, both in the leg and in the thigh. The leg segment corresponds to the popular terms Leonardo's vein or posterior arch vein . The term superficial accessory great saphenous vein is considered to be any venous segment ascending parallel to the GSV and located just superficial to the saphenous fascia, both in the leg and in the thigh.
Circumflex veins, by definition, drain into the GSV from an oblique direction. The posterior thigh circumflex vein is present in virtually every case; however, the anterior thigh circumflex vein is less common.
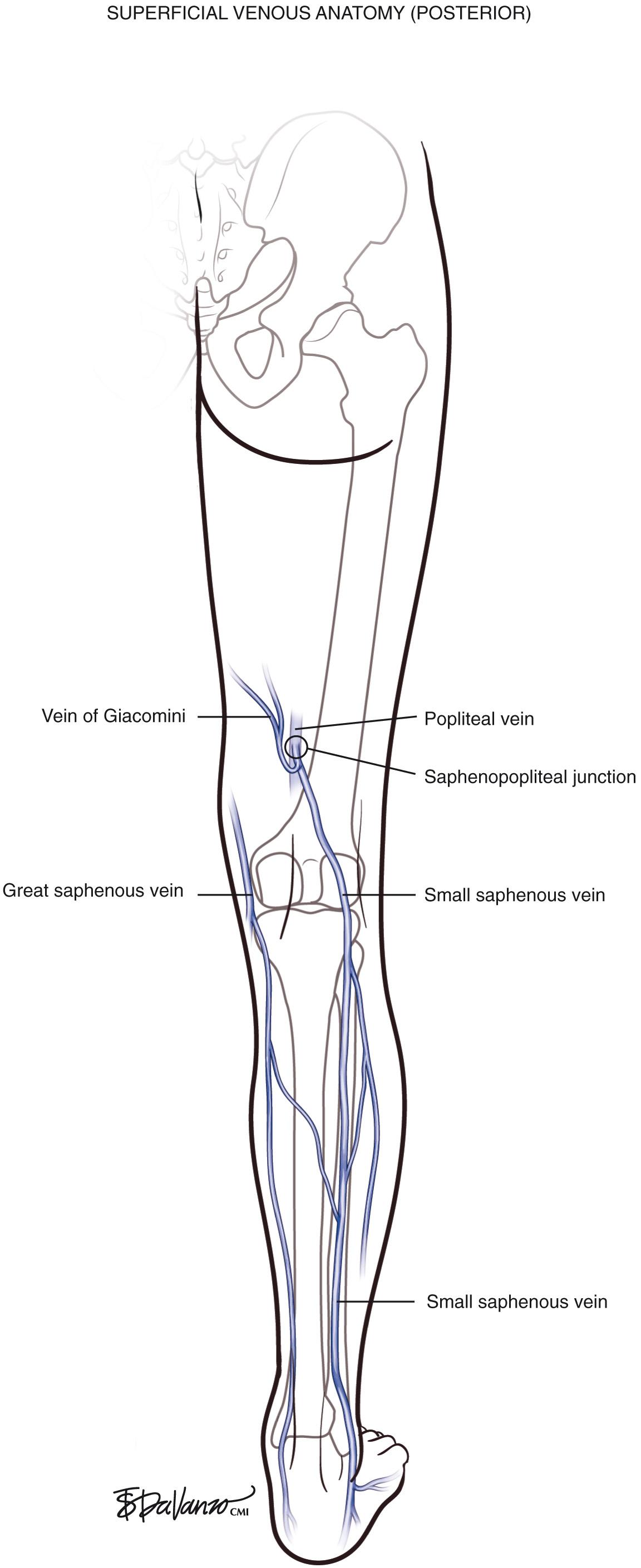
The SSV originates in the lateral foot and passes posterolaterally in the lower calf. The SSV lies above the deep fascia in the midline as it reaches the upper calf, where it pierces the two heads of the gastrocnemius muscle and courses cephalad until it enters the popliteal space. In approximately two-thirds of patients, the SSV drains entirely into the popliteal vein just above the knee at the saphenopopliteal junction (SPJ). In as many as one-third of patients, the cranial extension of the SSV drains into a posterior medial tributary of the GSV or directly into the GSV (vein of Giacomini) or into the femoral vein via a thigh perforating vein.
In variant drainage, a standard SPJ may or may not be present. The SSV is truly duplicated in 4% of cases; most often, this is segmental and primarily involves the midportion of the vein ( Fig. 1.5 ).
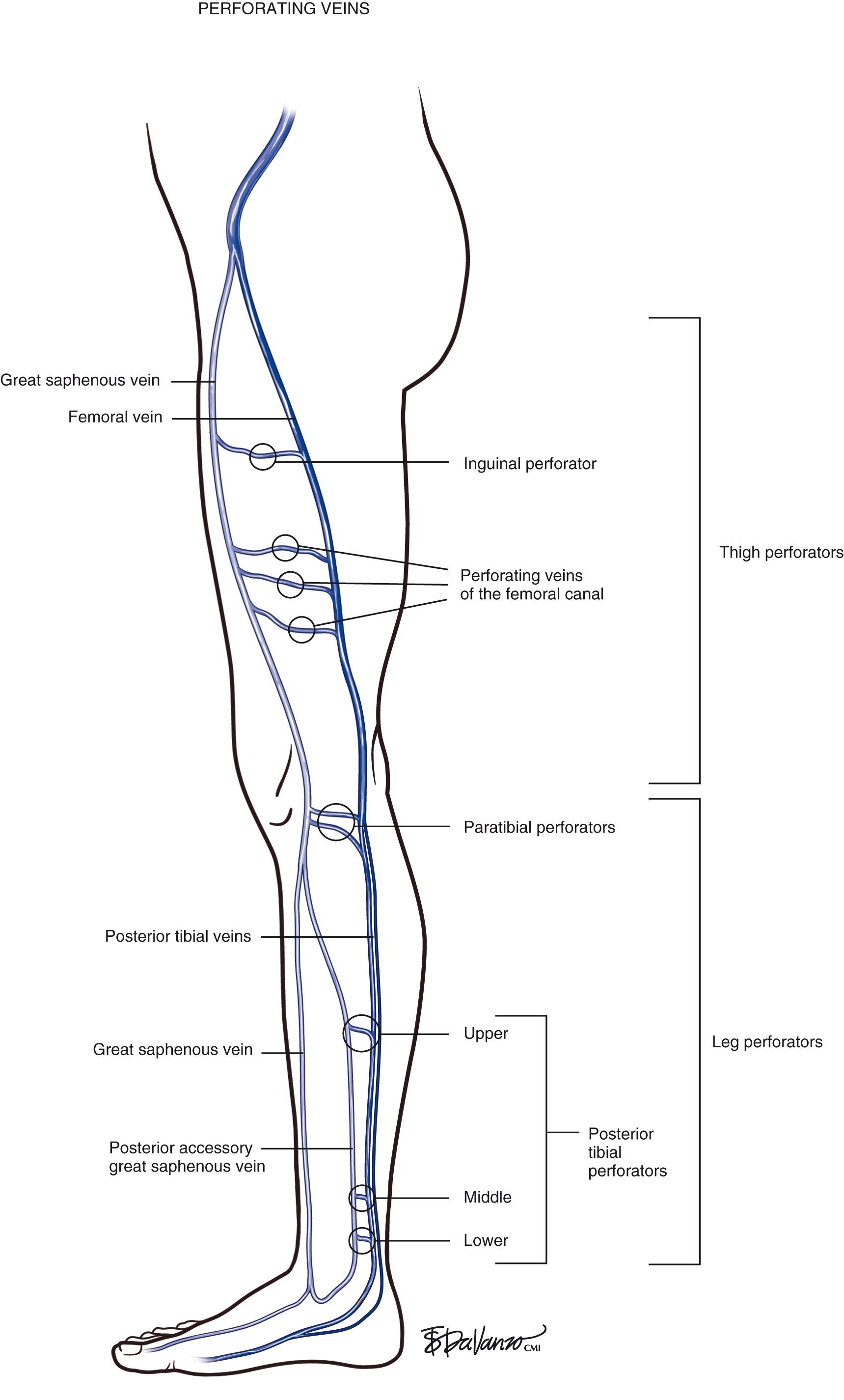
Identifying perforating veins based on the original descriptions of investigators (i.e., Cockett, Sherman, Dodd) is falling into disfavor. Descriptive terms based on topography, which designate the anatomic location, have become the contemporary approach. Perforating veins pass through defects in the deep fascia to connect deep and superficial veins of the calf or thigh. Venous valves prevent reflux of blood from the deep veins into the superficial system. Perforating veins may connect the GSV to the deep system at the femoral, posterior tibial, gastrocnemius, and soleal vein levels. Located between the ankle and the knee are perforating veins, formerly known as Cockett perforators, that connect the posterior tibial venous system with the PAGSV of the calf (also known as the posterior arch vein) ( Fig. 1.6 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here