Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The term vasculitis refers to inflammation of blood vessels, a finding that can be seen in association with a variety of clinical manifestations and as either a primary or secondary phenomenon. Along with vessel inflammation there is deposition of fibrinoid material in vessel walls and the presence of nuclear fragments (nuclear dust) resulting from disintegration of neutrophilic nuclei (karyorrhexis) within the vessel wall and surrounding tissues (hence the terminology leukocytoclastic vasculitis [LCV]). The presence of vasculitis may result in tissue injury as a result of vascular stenosis, occlusion, aneurysm, or rupture. The incidence of childhood vasculitis has been estimated at 20 to 50 cases per 100,000 children per year, with geographic differences noted throughout the world. ,
The vasculitic disorders are a heterogeneous group of conditions, many of which present with (or eventually result in) cutaneous manifestations. The range of clinical features is broad, from skin-limited changes to severe multiorgan involvement. Classification of the vasculitides is difficult and has most often been based on the gross and microscopic features of the disease process, primarily the vessel size involved (i.e., large, medium, or small). Large-vessel vasculitides, which will not be discussed here, include giant-cell (temporal) arteritis and Takayasu arteritis. Medium-sized vasculitides involve predominantly visceral arteries and include two of the most common forms of pediatric vasculitis syndromes, polyarteritis nodosa and Kawasaki disease (KD), both of which will be discussed. The other entities covered in this chapter all represent small-vessel disorders, which tend to involve primarily capillaries and venules; this category includes the most common form of pediatric vasculitis, Henoch–Schönlein purpura (immunoglobulin [Ig] A vasculitis), which in one retrospective study of LCV in children represented nearly 50% of all biopsy-proven cases. It should be remembered that this classification of vasculitis based on vessel size is imprecise, and overlap in the size of involved vessels is common. A summary classification of pediatric vasculitides is shown in Table 21.1 . The original patient groups used to develop vasculitis classification criteria by the American College of Rheumatology (ACR) did not include children. Subsequently the vasculitis working group of the Pediatric Rheumatology European Society (PRES), in conjunction with the European League Against Rheumatism (EULAR) and the Pediatric Rheumatology International Trials Organization (PRINTO), developed and validated criteria for some of the most common childhood vasculitides, a process that culminated in the 2008 Ankara Consensus Conference. , A summary of these criteria is shown in Table 21.2 . Notably, Kawasaki disease, another one of the most common vasculitides in childhood, was not included in this classification; criteria set forth by the American Heart Association are typically used in this clinical setting. ,
| Predominant Vessel Size | Disorder |
|---|---|
| Large | Takayasu arteritis |
| Medium | Polyarteritis nodosa Kawasaki disease |
| Small | Hypersensitivity vasculitis (cutaneous leukocytoclastic vasculitis) Henoch–Schönlein purpura (IgA vasculitis) Acute hemorrhagic edema of infancy Hypocomplementemic urticarial vasculitis Cryoglobulinemic vasculitis Erythema elevatum diutinum (primarily adults) ANCA associated:
|
| Other | Behçet syndrome Secondary vasculitides, including those related to infection, malignancy, medication, and autoimmune disorders |
| Disorder | Diagnostic Criteria |
|---|---|
| Henoch–Schönlein purpura | Purpura or petechiae (mandatory) with lower limb predominance † and at least one of following four criteria:
|
| Childhood polyarteritis nodosa | Histopathology (necrotizing vasculitis in medium- or small-sized arteries) or angiographic abnormalities ‡ (mandatory) plus one of the following five criteria:
|
| Granulomatosis with polyangiitis || | At least three of the following six criteria: |
* Also referred to as EULAR/PRINTO/PRES criteria .
† For purpura with atypical distribution, demonstration of IgA deposit in biopsy required.
‡ Angiography: aneurysm, stenosis, or occlusion of medium- or small-sized artery.
§ Livedo reticularis, nodules, infarctions.
|| Formerly known as Wegener granulomatosis.
¶ Purulent/bloody nasal discharge, recurrent epistaxis/crusts/granulomas, septal perforation or saddle nose deformity, sinusitis.
Henoch–Schönlein purpura (HSP), also known as anaphylactoid purpura and IgA vasculitis , is a form of small-vessel vasculitis that occurs primarily in children (especially boys) between 2 and 11 years of age, most commonly occurring in children younger than 5 years. It is the most common type of childhood systemic vasculitis. The classic presentation is a combination of nonthrombocytopenic palpable purpura in dependent areas, arthritis, abdominal pain, and glomerulonephritis. HSP is an inflammatory disorder that has been linked hypothetically to several potential causal agents, although the exact etiology remains unclear; these agents include group A β-hemolytic streptococci (GABHS), Helicobacter pylori, Haemophilus parainfluenza, and other bacterial, mycobacterial or viral organisms; immunizations; and medications. , There are reports of patients with coexisting HSP and acute rheumatic fever, highlighting the potential association between GABHS and HSP. Bartonella henselae has also been suggested as a potential causative infectious agent. Although the nature of the immunologic reaction in HSP is not completely clear, the common history of antecedent upper respiratory tract infection preceding the onset of symptoms suggests a hypersensitivity phenomenon resulting in localized or widespread vascular damage. A fairly consistent immunologic observation is the deposition of IgA immune complexes in affected organs (i.e., skin, kidneys) when studied by immunofluorescence. IgA complexes, however, are not a necessary requirement for the development of HSP, and their absence should not exclude the diagnosis. Around one-third of patients have elevated serum IgA levels. Several polymorphisms involving cytokines and cell-adhesion molecules that modulate inflammatory responses and endothelial cell activation have been observed and may correlate with disease susceptibility, extent of involvement, or severity of renal disease. Mutations in the MEFV gene, which is classically associated with familial Mediterranean fever with homozygous or compound heterozygous mutation, have been described in some patients with HSP and may portend more common gastrointestinal and joint involvement and edema.
The clinical picture of HSP is often, but not always, distinctive. Most patients with a rash present with an initial urticarial eruption of macules and papules ( Fig. 21.1 ) that rapidly become purpuric and are distributed primarily on the lower extremities ( Figs. 21.2 through 21.4 ) and buttocks ( Fig. 21.5 ), in dependent locations. Lesions may also occur on the upper extremities, trunk, and face, and in some instances skin lesions may develop in patterns at pressure sites. In some patients, petechiae ( Fig. 21.6 ) or ecchymoses (“bruises”) ( Fig. 21.7 ) may predominate over the typical palpable purpuric lesions. The cutaneous eruption is the presenting feature of HSP in 50% of cases. Newer purpuric lesions develop and may result in a polymorphous appearance. Other skin lesion morphologies, including vesicular or bullous lesions ( Fig. 21.8 ), erosions or ulcers, necrosis, gangrene, and even erythema multiforme–like lesions, may occur. , Marked edema of the hands, feet, scalp, or face may also be seen, especially in younger patients. , The disease often consists of a single episode that may last for several days to weeks, but in some cases recurrent attacks may occur at intervals for weeks to months.



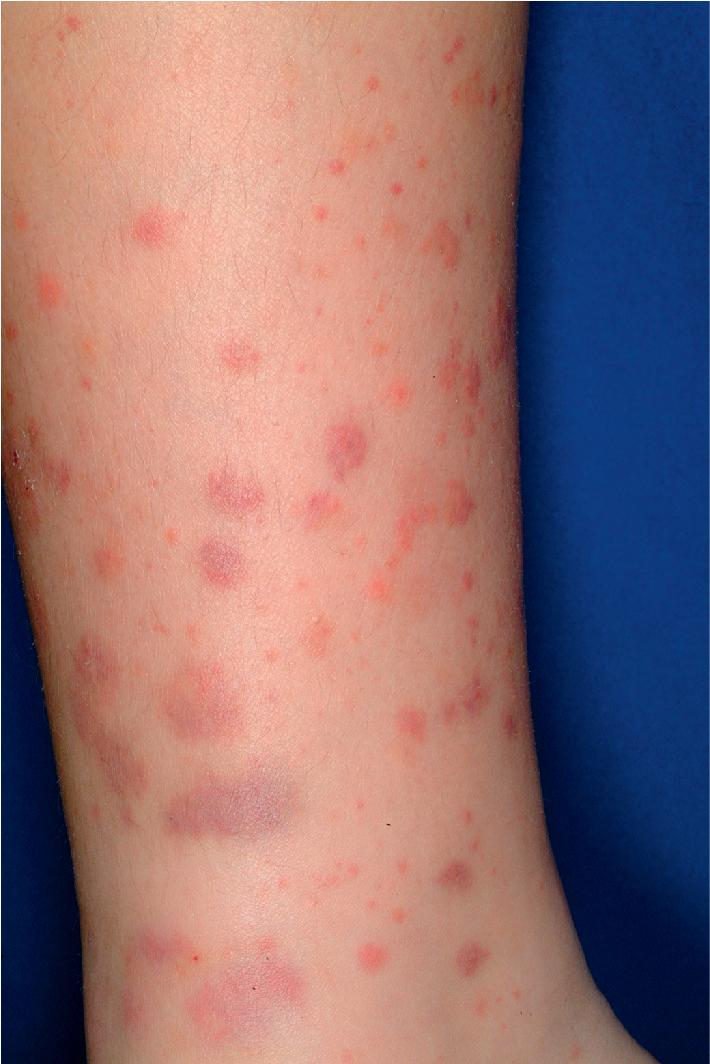




Individual lesions of HSP occur in crops, tend to fade after about 5 days, and eventually are replaced by areas of hyperpigmentation or ecchymoses. Although the differential diagnosis of the skin lesions may include drug reaction, erythema multiforme, or urticaria, the presence of palpable purpura (the hallmark of leukocytoclastic vasculitis) will usually clarify the true nature of the disorder. This characteristic finding, created by edema and extravasation of erythrocytes, gives individual lesions their diagnostic palpable and purpuric appearance as well as their nonblanching quality (i.e., individual lesions cannot be blanched when viewed through a glass slide exerting pressure over the surface, a technique called diascopy ).
Occasionally the face, mucous membranes of the mouth and nose, and anogenital regions may show petechiae. In males, vasculitis of the scrotal vessels may lead to acute scrotal swelling with or without erythema or purpura ( Fig. 21.9 ); penile swelling and purpura may also be present. Pain may be severe, and this presentation may mimic that of testicular torsion or other causes of “acute scrotum,” necessitating ultrasonography and/or radionuclide scans to help differentiate between these disorders. In one study, roughly 20% of males with HSP had scrotal involvement, and these patients were noted to have an association with headache, edema, and elevated C3 levels.

Systemic involvement in HSP, which is seen in up to 80% of cases, most commonly occurs in the kidneys, gastrointestinal tract, and joints. The degree of systemic involvement varies, with joint or gastrointestinal symptoms seen in as many as two-thirds of affected children. Renal disease occurs most often and is the most significant correlate of long-term prognosis.
The clinical expression of HSP kidney involvement varies from transient microscopic hematuria to rapidly progressive glomerulonephritis. Glomerulonephritis is seen overall in 40% to 50% of children with HSP and is usually transient and benign. The renal lesion in HSP is indistinguishable histopathologically from that of IgA nephropathy (Berger disease), although the latter tends to occur more often in older patients. The renal involvement may not become apparent for several weeks; hence the importance of long-term follow-up monitoring for development of this complication. Most often, however, if kidney involvement is going to be seen, it will be found within 3 months of disease onset. Microscopic hematuria is the most common clinical manifestation of HSP kidney involvement. Potential correlates of kidney disease in HSP include age older than 4 years, persistent purpura, severe abdominal pain, and depressed coagulation factor XIII activity of less than 80%. Initial renal insufficiency appears to be the single best predictor of the further clinical course in children with HSP nephritis.
Gastrointestinal signs and symptoms result from edema and hemorrhage of the bowel wall as a result of vasculitis. They most often include colicky abdominal pain (which may be severe and associated with vomiting), hematochezia, and hematemesis. Visceral infarction or perforation, pancreatitis, cholecystitis, esophageal involvement, colitis, protein-losing enteropathy, intussusception, hemorrhage, or shock may also be associated. Intussusception, seen in up to 2% of patients, is more common in boys. Because non-HSP–associated intussusception generally occurs in children younger than 2 years of age, when intussusception is diagnosed in older children HSP must be strongly considered. Chronic intestinal obstruction with ileal stricture has also been reported, occurring months after resolution of the acute illness. Gastrointestinal involvement with HSP is more likely when there are clinical findings of edema and cutaneous lesions above the waist.
Joint involvement in HSP is characterized by tender and painful joints with primarily periarticular swelling. True arthritis is less common. Although the ankles and knees are most often affected, the elbows, hands, and feet may also be involved. HSP joint symptoms tend to be oligoarticular. Arthritic symptoms are usually transient and rarely result in permanent deformity.
In addition to the skin, genitourinary and gastrointestinal tracts, and joints, other organ involvement is occasionally seen in HSP. Central nervous system (CNS) involvement results most commonly in headache and, occasionally, behavioral alteration, hyperactivity, intracerebral bleeds, paresis, or seizures. , Status epilepticus has been rarely reported. Respiratory involvement may range from an asymptomatic pulmonary infiltrate to recurrent episodes of pulmonary hemorrhage. Bleeding diathesis may occasionally occur.
The diagnosis of HSP is seldom difficult when patients exhibit the classic “tetrad” of organ involvement (skin, kidneys, gastrointestinal tract, and joints). However, many patients show only some of these findings, and the differential diagnosis depends on which organ-specific symptoms predominate. The differential diagnosis of palpable purpura may include hypersensitivity vasculitis (usually caused by drug reaction; see Hypersensitivity Vasculitis section), hemorrhagic diathesis (i.e., factor deficiency), or sepsis. In addition, the more “ecchymotic” lesions of HSP may be mistaken for child abuse and must be evaluated within the context of the overall clinical presentation. When the diagnosis remains in doubt, histopathologic examination of a skin biopsy specimen is useful in confirming the presence of vasculitis. Direct immunofluorescence revealing IgA immune complexes is highly suggestive of but not pathognomonic for HSP. Other laboratory investigations to be considered include serum chemistry profile, blood cell counts, coagulation studies, abdominal radiographic studies, stool guaiac testing, urinalysis, and kidney biopsy. Early diagnosis of gastrointestinal HSP may be facilitated by high-spatial-resolution ultrasound and fecal calprotectin studies, both of which have been shown to have good sensitivity and specificity for abdominal disease. ,
The overall prognosis for most patients with HSP is excellent, and full recovery without permanent residua is the norm. The disease tends to run its course over 4 to 6 weeks. In younger children, the disease is generally milder and of shorter duration with fewer renal and gastrointestinal manifestations and few recurrences. Renal disease is the most important prognostic indicator, and end-stage renal disease may occur in up to 5% of patients with nephritis. Long-term follow-up care is indicated in patients with kidney involvement. Recurrent flares of HSP may occur in up to 3% of patients and in one study had a lag period of 2 to 26 months after the initial presentation.
Supportive care is sufficient for the majority of patients, and nonsteroidal antiinflammatory agents are useful for significant joint pain. The goals of HSP therapy are to minimize symptoms, decrease short-term morbidities, and prevent chronic renal insufficiency. Systemic corticosteroids have been advocated for patients with severe gastrointestinal, joint, or scrotal involvement, as well as for renal involvement. They are generally not recommended for rash, mild joint pain, or mild abdominal discomfort alone. Various regimens have been recommended for HSP nephritis, including oral methylprednisolone or prednisone, high-dose intravenous pulse methylprednisolone, urokinase, cyclophosphamide, mycophenolate mofetil (MMF), azathioprine, plasma exchange, dipyridamole, and heparin/warfarin. , Treatment with MMF may be helpful in achieving and maintaining long-term remission from HSP nephritis. Severe gastrointestinal involvement may respond well to intravenous immunoglobulin therapy, but increasing proteinuria may be an associated limitation.
The benefits of systemic steroid therapy for HSP remain somewhat controversial. A meta-analysis revealed that corticosteroids reduced the mean resolution time of abdominal pain, reduced the odds of developing persistent kidney disease, and reduced the odds of both surgical intervention and recurrence. However, in a long-term study assessing outcomes 8 years after a randomized placebo-controlled prednisone study in a cohort of 171 HSP patients, there were no differences between prednisone and placebo groups with regard to hematuria, proteinuria, or hypertension. A retrospective cohort study of hospitalized children with HSP revealed an association between decreased hazard ratios for abdominal surgery, endoscopy and abdominal imaging, and early corticosteroid exposure. Taken together, these and other reports suggest the need for more controlled studies of the effect of corticosteroids on HSP outcomes.
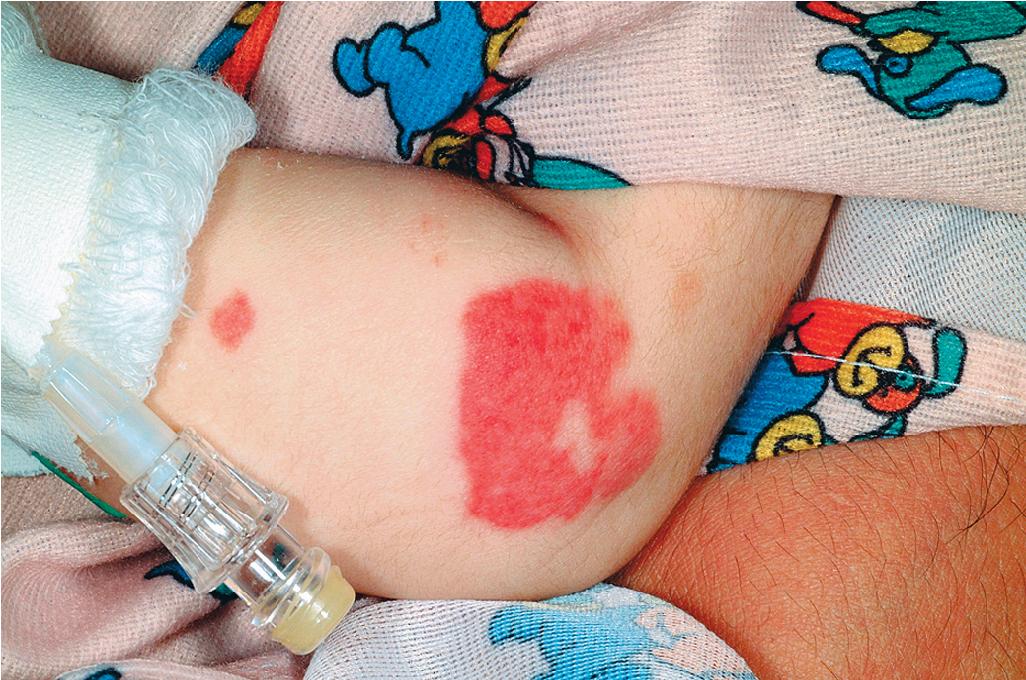
Acute hemorrhagic edema (AHE) of infancy (AHE of childhood, Finkelstein disease, Finkelstein–Seidlmayer syndrome) is a form of leukocytoclastic vasculitis characterized by fever, large purpuric skin lesions, and tender edema and reported most often in infants and children between the ages of 4 months and 3 years (and usually ≤24 months). The cutaneous lesions often have a “cockade” (medallion-like) pattern, with scalloped borders and central clearing ( Fig. 21.10 ). They begin as edematous papules with petechiae and expand centrifugally with coalescence to result in the characteristic clinical pattern ( Figs. 21.11 and 21.12 ). Facial edema is common, and edema may also involve the ears and distal extremities. Scrotal and/or penile swelling may be present. Although the cutaneous eruption may be impressive, patients are typically otherwise well, and involvement of the gastrointestinal tract, kidneys, and joints is uncommon. However, in one retrospective series of 26 patients with AHE, 50% had features of some systemic involvement, including arthralgias/arthritis, gastrointestinal hemorrhage, or microscopic hematuria. Fever, present in around 50% of patients, is usually low grade. Intussusception has been rarely observed. The cause is unclear, although an infectious trigger (i.e., upper respiratory infection, conjunctivitis, pharyngitis, otitis media, or pneumonia) is hypothesized. Associations with vaccination have also been reported. Prodromal symptoms most often are limited to those of respiratory tract illness or diarrhea.


Skin biopsy in AHE reveals leukocytoclastic vasculitis similar to HSP. Direct immunofluorescence studies, however, do not consistently reveal IgA deposition and in up to three-quarters of patients are entirely negative. , Laboratory findings may include leukocytosis and an elevated erythrocyte sedimentation rate, but hematuria, proteinuria, and hematochezia are usually absent. The course of AHE is marked by a rapid onset with a short benign course followed by complete recovery, usually over 1 to 3 weeks. No treatment is generally necessary, because AHE is typically a self-limited process (involuting in most patients within 3 weeks). Although the disorder resembles HSP, controversy exists over whether it represents an infantile form of HSP or whether it is a distinct and unrelated clinical entity. Arguments in favor of the latter include the usual lack of internal organ involvement, the absence of IgA immune deposits in most patients, and the overall benign course without a propensity toward recurrences.
Hypersensitivity vasculitis (HV) (cutaneous small-vessel vasculitis, cutaneous leukocytoclastic vasculitis, cutaneous leukocytoclastic angiitis) is a term used to denote a leukocytoclastic vasculitis involving primarily the skin and in most cases is secondary to a drug ingestion or infectious process. It is most common in adults and significantly less common in children, in whom HSP is the most common form of cutaneous vasculitis. Potential infectious causes of HV include streptococci, hepatitis B and C, human immunodeficiency virus (HIV), nontyphoidal Salmonella, and Mycobacteria (both tuberculous and nontuberculous). , Other potential disease associations include autoimmune disorders and malignancy (hematologic and solid organ).
The diagnosis of HV is one of exclusion, and other causes of primary cutaneous vasculitis (i.e., HSP, cryoglobulinemic vasculitis [CV]) or secondary cutaneous vasculitis (i.e., urticarial vasculitis, connective tissue disorders, malignancy, endocarditis, Behçet disease) must be ruled out. The lesions of HV tend to occur in “crops” (groups of lesions of similar age) because of simultaneous exposure to the inciting antigen.
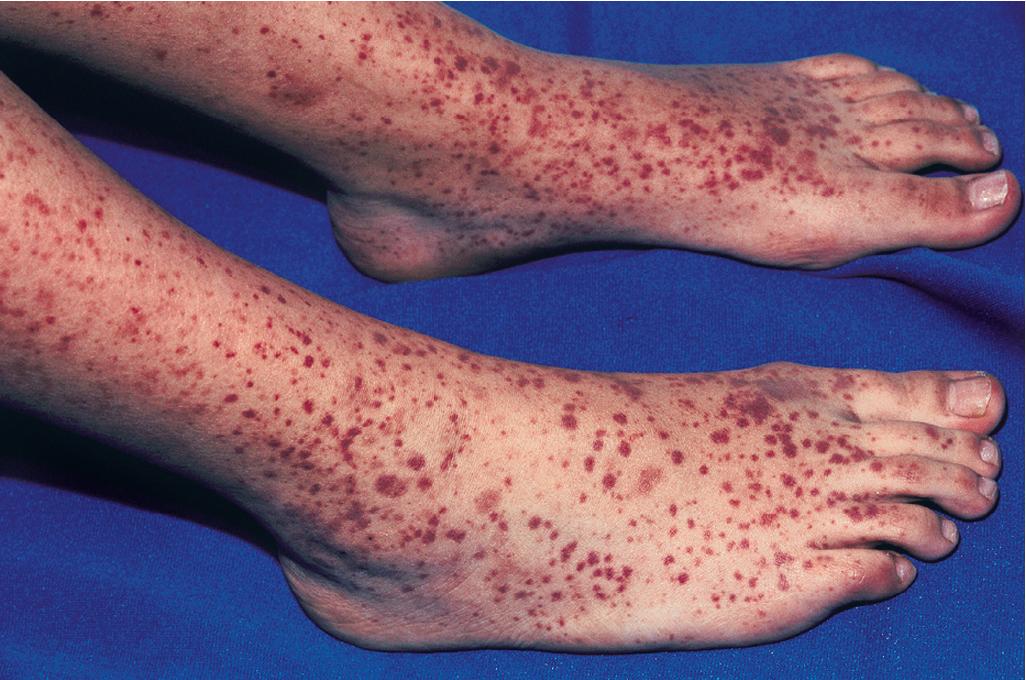
Patients with HV most often present with palpable purpura ( Fig. 21.13 ) and less often with urticaria, vesicles, pustules, superficial ulcers, or necrotic lesions. The lesions may be smaller and petechial in appearance in some patients ( Fig. 21.14 ). Skin involvement is most notable in dependent areas and in areas of trauma or tight-fitting clothing. Symptoms are usually absent, although pain or burning may be present, and systemic involvement is uncommon.

The list of potential drug causes of HV is extensive and includes multiple classes of antibiotics, nonsteroidal antiinflammatory agents, antiepileptic drugs, insulin, propylthiouracil, tumor necrosis factor-α (TNF-α) antagonists, levamisole, omeprazole, and oral contraceptives. (For a more complete listing of potential drug etiologies, see Chapter 20 .) Identification and withdrawal of the offending agent is vital in patients with HV, and in those with skin-limited disease no other specific therapy is usually necessary. For patients with either severe cutaneous or systemic involvement, therapeutic options include corticosteroids, colchicine, dapsone, hydroxychloroquine, and other immunosuppressive agents, including mycophenolate mofetil, azathioprine, methotrexate, cyclosporine, and rituximab. The lesions of HV usually resolve over weeks to months with resultant postinflammatory hyperpigmentation.
Urticarial vasculitis (UV) refers to a type of cutaneous leukocytoclastic vasculitis that presents with urticarial features and is often associated with an underlying systemic disease. In contrast to common urticaria, the lesions of UV are distinct in that they last for longer than 24 to 48 hours, often have a dusky or purpuric appearance, are associated more often with burning than pruritus, and leave postinflammatory hyperpigmentation after resolution ( Fig. 21.15 ). , Confirmation of the diagnosis of UV often requires skin biopsy given the potential overlap with other conditions, especially allergic urticaria. Deposits of immunoglobulins, complement, or fibrin may be found around blood vessels in UV in up to 80% of patients.

UV may be idiopathic or associated with other diseases including autoimmune disorders, infections, drug reactions, or paraneoplastic syndromes. Most patients can be characterized as having either normocomplementemic UV (in which case the majority represent idiopathic UV) or hypocomplementemic UV (see the following section). Patients with hypocomplementemic UV have a propensity toward more severe multiorgan involvement and systemic disease associations. , , The most commonly associated autoimmune disorders are systemic lupus erythematosus (SLE) and Sjögren syndrome (see Chapter 22 ). Serum sickness–like reactions to drugs, cryoglobulinemia, and hepatitis C virus (HCV) infection are also associated in some patients with UV, and it has been observed after some vaccinations. ,
Hypocomplementemic urticarial vasculitis syndrome (HUVS) is the term used to describe patients with UV in association with angioedema and systemic symptoms, most often obstructive pulmonary disease and ocular inflammation (conjunctivitis, iritis, episcleritis, uveitis). Glomerulonephritis, gastrointestinal involvement, and arthritis may also be present, and the condition is relatively rare in pediatric patients. Isolated microscopic hematuria may be the only sign of renal involvement, which may show features of systemic lupus erythematosus–associated kidney disease and can be progressive. Decreased serum Clq levels are seen in most patients with HUVS, and autoantibodies against this factor are detectable in the serum. , Although antibodies to Clq are also found in some patients with SLE, HUVS appears to be a unique entity.
The cutaneous lesions of UV are urticarial in nature, favor the trunk and proximal extremities, and often have a purpuric quality. The primary distinguishing features are the persistence of lesions longer than is typical for allergic urticaria (2 to 6 hours), pain or burning, and associated hyperpigmentation as the lesions resolve. If the diagnosis of UV is confirmed, a thorough physical examination and laboratory investigation to assess for associated conditions are indicated. If an underlying disease is identified, specific therapy for that disorder is indicated. There is otherwise no specific therapy for UV. Various therapeutic modalities, including prednisone, hydroxychloroquine, indomethacin, azathioprine, colchicine, methotrexate, cyclophosphamide, mycophenolate mofetil, cyclosporine, intravenous Ig, rituximab, and dapsone, have been used but with an inconsistent response. , ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here