Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A variety of vascular lesions can serve as cutaneous signs of systemic disease.
Telangiectasias or angiokeratomas with particular morphologies and distributions raise suspicion for an autoimmune connective tissue disease or a genetic disorder.
Vascular anomalies are divided into two major categories: tumors due to endothelial cell proliferation and malformations that result from errors in vascular morphogenesis.
Benign vascular tumors and vascular malformations may have associated widespread or regional extracutaneous findings.
Kaposi’s sarcoma and angiosarcoma represent two malignant vascular tumors with internal manifestations.
There are a number of vascular lesions that serve as cutaneous signs of systemic disease, from the mat telangiectasias of scleroderma and the papular telangiectasias of hereditary hemorrhagic telangiectasia (Osler–Weber–Rendu syndrome) to the angiokeratomas of Fabry disease. In addition, some vascular tumors and malformations may be associated with extracutaneous findings such as profound thrombocytopenia in Kasabach–Merritt syndrome or glaucoma and neurologic abnormalities in Sturge–Weber syndrome. Over the past several decades, increased appreciation of the differences between vascular tumors and malformations has led to improved classification and management of these lesions. This chapter concludes with a discussion of two malignant vascular tumors with potential internal manifestations: Kaposi’s sarcoma and angiosarcoma.
Telangiectasias are such a common cutaneous finding that they are often overlooked or disregarded. In the head and neck region, the linear variety is most commonly due to solar damage or rosacea, whereas on the lower extremities telangiectasias are usually a sign of venous hypertension ( Fig. 23-1 ; Table 23-1 ). The recurrent flushing of the face and upper trunk that occurs in patients with the carcinoid syndrome may also be accompanied by linear telangiectasias, which can result in misdiagnosis as the erythematotelangiectatic form of rosacea.

| Primary Cutaneous Disorders |
| Linear |
|
| Papular or punctate |
|
| Spider |
|
| Stellate |
|
| Poikiloderma |
|
| Systemic Diseases |
| Linear |
|
| Papular |
|
| Spider |
|
| Mat |
|
| Periungual |
|
| Poikiloderma |
|
In ataxia–telangiectasia, linear telangiectasias first appear on the bulbar conjunctivae during early childhood, followed over time by similar, but often more subtle, lesions in sites such as the periocular skin, ears, and antecubital and popliteal fossae. The telangiectasias are typically preceded by the onset of cerebellar ataxia when the patient began to walk. Additional skin findings may include granulomatous dermatitis, nevoid hyper- or hypopigmentation, and progeric changes. Affected individuals usually develop recurrent pulmonary infections and are at high risk of lymphoproliferative disorders. This autosomal recessive disorder is due to mutations in the ATM gene, but how this relates to the formation of telangiectasias is not well understood (see Chapter 34 ).
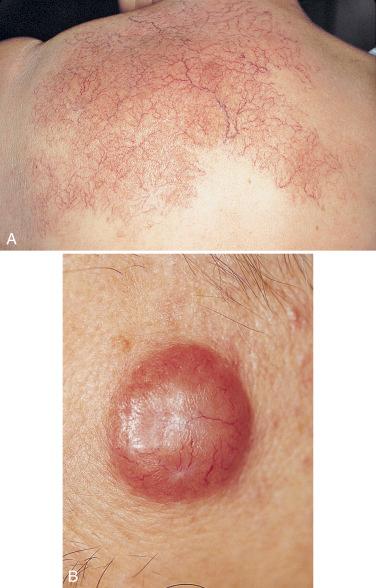
A rare variant of mastocytosis (see Chapter 36 ) referred to as telangiectasia macularis eruptiva perstans (TMEP) is characterized by multiple clusters of telangiectasias. Although somatic activating mutations in the KIT gene are found in most adults with urticaria pigmentosa, to date they have not been reported in patients with TMEP. Arborizing telangiectasias are a classic feature of basal cell carcinomas, and telangiectasias are also seen within cutaneous B-cell lymphomas ( Fig. 23-2 ).
One or two papular telangiectasias commonly occur on the face or hands of healthy individuals, especially women and children. Spider telangiectasias (also known as spider angiomas or spider nevi) represent dilations in ascending dermal arterioles and are characterized by both a punctum and radiating legs. The development of multiple spider telangiectasias can be a sign of hyperestrogenemia, such as occurs during pregnancy and in patients with hepatic cirrhosis.
The presence of multiple papular and stellate macular telangiectasias on the oral mucosa and lips ( Fig. 23-3, A ) as well as the face, fingers ( Fig. 23-3, B ), and nailfolds ( Fig. 23-3, C ) raises the possibility of hereditary hemorrhagic telangiectasia (HHT; Osler–Weber–Rendu syndrome). These vascular lesions most often become apparent around or after puberty, and a personal or family history of epistaxis, gastrointestinal bleeding, or cerebrovascular accidents increases suspicion of this autosomal dominant condition. The vascular lesions of HHT actually represent arteriovenous malformations (AVMs), which explains their propensity to bleed. By stretching the skin, an eccentric punctum with radiating branches can be visualized.

When the clinical diagnosis of HHT is made, it is important to screen individuals with a transthoracic echocardiogram bubble study (which assesses shunting) and a brain MRI with gadolinium enhancement to exclude pulmonary and cerebral AVMs, both of which are amenable to interventional vascular procedures, e.g., embolotherapy or surgical excision. Most patients with HHT have a mutation in ENG or ACVRL1 , genes that encode endoglin and activin A receptor type II-like 1, respectively. Patients with juvenile gastrointestinal polyposis in addition to HHT may have mutations in the SMAD4 gene, which encodes a protein that, like endoglin and ACVRL1, is involved in transforming growth factor-β signaling; these patients are at increased risk of early-onset colorectal carcinoma.
Poikiloderma is defined by the presence of (1) telangiectasias; (2) wrinkling due to epidermal atrophy; and (3) reticulated areas of hypo- and hyperpigmentation. This combination of skin findings is characteristically seen years after orthovoltage irradiation. Poikiloderma can be a feature of dermatomyositis ( Fig. 23-4, A ) and cutaneous T-cell lymphoma. In the latter condition, the lesions favor the axillae and groin ( Fig. 23-4, B ).

Telangiectasias, in particular mat and periungual variants, are an important cutaneous clue to the diagnosis of autoimmune connective tissue diseases (AI-CTD). Mat telangiectasias are flat, often have a polygonal shape, and favor the face, oral mucosa, and hands ( Fig. 23-5 ). They are a sign of scleroderma or an overlap syndrome that includes scleroderma. Of note, in the acronym for the more indolent, anticentromere antibody-positive CREST variant of scleroderma, the T stands for telangiectasias. Periungual telangiectasias are seen in systemic lupus erythematosus (SLE), dermatomyositis (DM), and scleroderma. In the latter two AI-CTD, individual telangiectasias appearing as swollen loops are admixed with avascular areas ( Fig. 23-6 ), whereas in lupus the telangiectasias have an appearance that has been likened to that of renal glomeruli. Nailfold telangiectasias are accompanied by erythema in SLE, and both erythema and ragged cuticles in DM.


On the basis of biologic characteristics, vascular anomalies are divided into two major categories ( Table 23-2 ): vascular tumors, which arise by cellular hyperplasia; and vascular malformations, which result from errors in vascular morphogenesis during intrauterine development and have normal cellular turnover. When vascular tumors are compared to vascular malformations, there are important differences in natural history, histologic features, associated findings ( Table 23-3 ), and treatment options. However, despite the distinct processes that govern their development, occasionally vascular tumors and malformations are associated with one another, e.g., in kindreds with autosomal dominant cosegregation of infantile hemangiomas and vascular malformations. This suggests overlap in the regulation of prenatal vascular development and postnatal endothelial cell proliferation.
| Benign vascular neoplasms and reactive proliferations |
|
| Vascular malformations |
| Low flow |
|
| High flow |
|
∗ Can be associated with Kasabach–Merritt syndrome or, for RICH, a milder thrombocytopenic coagulopathy.
† Associated with peripheral eosinophilia and enlargement of regional lymph nodes.
‡ Can be associated with systemic disorders such as monoclonal gammopathies (including type I cryoglobulinemia), antiphospholipid syndrome, bacterial endocarditis, and atherosclerosis (diffuse dermal angiomatosis variant).
| Syndrome/Association | Features of Vascular Lesion(s) | Associated Clinical Features | |
|---|---|---|---|
| Vascular tumors | Kasabach–Merritt syndrome | Kaposiform hemangioendothelioma or tufted angioma; large, rapidly growing ecchymotic mass (cutaneous or retroperitoneal) | Severe thrombocytopenia and variable consumption coagulopathy; occurs primarily in infants; possible mortality |
| Multifocal lymphangioendotheliomatosis with thrombocytopenia | Multiple (often >100) red-brown papules and plaques present at birth or appearing during infancy + gastrointestinal > pulmonary involvement | Thrombocytopenia; severe gastrointestinal bleeding; occasionally hemoptysis; possible mortality | |
| Multifocal infantile hemangiomas with extracutaneous involvement (diffuse neonatal hemangiomatosis) | Multiple (≥5) small cutaneous hemangiomas + internal hemangiomas affecting the liver and rarely other organs (e.g., gastrointestinal tract, lungs, brain) | Hepatomegaly, high-output cardiac failure, abdominal compartment syndrome, hypothyroidism (see text) | |
| Airway hemangiomas | Hemangiomas in “beard” distribution | Noisy breathing, biphasic stridor, hoarseness, respiratory failure | |
| PHACE(S) syndrome | Large (>5 cm) cervicofacial infantile hemangioma ∗ , typically in a segmental pattern correlating with a developmental unit (e.g., embryonic facial prominences; Fig. 23-16 ) | P osterior fossa malformations; H emangiomas; cervical and cerebral A rterial anomalies; C ardiac defects (especially C oarctation of the aorta); E ye anomalies; S ternal or S upraumbilical clefting | |
| LUMBAR syndrome | Midline L umbosacral or L ower body infantile hemangioma, often large and segmental ∗ | L ipoma/other skin lesions (e.g., “skin tag”): U rogenital anomalies, U lceration; M yelopathy (spinal dysraphism) † ; B ony deformities; A norectal, A rterial and R enal anomalies | |
| POEMS syndrome | Cherry angiomas, glomeruloid hemangiomas | P olyneuropathy, O rganomegaly, E ndocrinopathy, M -protein (monoclonal gammopathy), S kin changes such as diffuse hyperpigmentation, edema, sclerodermoid changes | |
| Vascular malformations § | Sturge–Weber syndrome (SWS) | Facial CM in V1 (±V2, V3) dermatomal distribution (uni- > bilateral) together with ipsilateral leptomeningeal ± choroidal CVM | Seizures, developmental delay, contralateral hemiparesis, characteristic “tram-track” cerebral gyral calcifications; ipsilateral glaucoma; facial soft tissue/bony hypertrophy over time; mosaic GNAQ mutation in affected tissues |
| Bonnet–Dechaume–Blanc (Wyburn–Mason) syndrome | (Centro)facial AVM (may mimic a CM) + metameric AVM of the ipsilateral orbit and/or brain | Ipsilateral visual impairment, various contralateral neurologic manifestations | |
| Cobb syndrome | AVM (may mimic a CM or angiokeratomas) in a dermatomal distribution + metameric AVM in the corresponding spinal cord segment | Neurologic manifestations of spinal cord compression (e.g., paraparesis) | |
| Klippel–Trenaunay syndrome (KTS) | CVM/CVLM of lower extremity > upper extremity, trunk; 85% unilateral; vascular stain with a sharply demarcated, geographic pattern is a sign of lymphatic involvement | Soft tissue/bony hypertrophy (or occasionally hypotrophy ‡ ) of affected limb(s), venous thrombosis and ulcers, lymphedema; occasionally gastrointestinal bleeding, hematuria and pulmonary embolism | |
| Parkes Weber syndrome (PKWS) | AVM ± CM/CLM of an extremity | Soft tissue/bony hypertrophy with progressive deformity over time, high-output cardiac failure | |
| Capillary malformation–arteriovenous malformation | Multifocal, small, round-to-oval pink to red-brown CM ± AVM of face, extremities, brain and/or spine | PKWS (see above); headaches, seizures, sensorimotor deficits, cerebral hemorrhage; AD inheritance of RASA1 mutations | |
| Cutaneous + cerebral capillary malformations | Hyperkeratotic cutaneous CVMs + cerebral CMs; congenital red-purple plaques and red-brown macules with peripheral telangiectatic puncta | Headaches, seizures, cerebral hemorrhage; AD inheritance, usually due to KRIT1 mutations | |
| Cutis marmorata telangiectatica congenita (CMTC) | Localized, segmental or generalized; broad, red-purple reticulated vascular network on extremities > trunk > face; telangiectasias, ± prominent veins, ± cutaneous atrophy | Often hypotrophy (rarely hypertrophy) of affected limb (girth > length); occasionally glaucoma, developmental delay; aplasia cutis + transverse limb defects ± cardiac malformation (Adams–Oliver syndrome) | |
| Megalencephaly–CM (macrocephaly–CM; formerly macrocephaly–CMTC) | Reticulated CM, persistent midfacial capillary stain | Macrocephaly, asymmetric overgrowth/hemihypertrophy, CNS abnormalities, developmental delay, syndactyly (especially of 2nd–3rd toes), joint laxity; mosaic PIK3CA mutations | |
| CLOVES syndrome | V ascular malformations (slow- or fast-flow) | C ongenital L ipomatous O vergrowth, E pidermal nevi, S keletal anomalies (e.g., scoliosis, splayed feet); mosaic PIK3CA mutations | |
| PTEN hamartoma-tumor syndrome (Bannayan–Riley–Ruvalcaba syndrome > Cowden disease) | Multifocal intramuscular arteriovenous anomalies associated with ectopic fat; ± CM, LM; intracranial developmental venous anomalies | Macrocephaly, developmental delay, lipomas, genital pigmented macules, trichilemmomas, acral keratoses, oral papillomas, neuromas, sclerotic fibromas, intestinal hamartomatous polyps, breast and thyroid adenoma/carcinoma; AD inheritance of PTEN mutations | |
| Proteus syndrome | CM/LM/CVM/CLM, most often of extremities | Progressive, disproportionate, asymmetric soft tissue/bony overgrowth, cerebriform connective tissue nevi of soles > palms, dermal hypoplasia, lipomas/regional absence of fat, epidermal nevi, CNS abnormalities, venous thrombosis/pulmonary embolism, lung cysts; mosaic AKT1 mutations | |
| Phacomatosis pigmentovascularis | CM > CMTC; ± nevus anemicus | Dermal melanocytosis and/or speckled lentiginous nevus (nevus spilus); may have extracutaneous features of SWS or KTS | |
| Blue rubber bleb nevus syndrome (Bean syndrome) | Multiple VM of skin, gastrointestinal tract > other organs | Gastrointestinal bleeding, anemia | |
| Multiple cutaneous and mucosal venous malformations | Multiple VM of skin, oral mucosa, and muscles | AD inheritance of TEK mutations | |
| Maffucci syndrome | Multiple VM/VLM, most often of distal extremities; spindle cell hemangioma | Multiple enchondromas of long bones, especially metacarpals and phalanges of the hands; chondrosarcoma (15%-30%); skeletal deformities, short stature; somatic IDH1 > 2 mutations in enchondromas and spindle cell hemangiomas | |
| Gorham syndrome | Multiple CVLM/LM of the skin, mediastinum, and bones | Massive osteolysis (“disappearing bones”), skeletal deformities, pathologic fractures, pulmonary complications | |
| Angiokeratomas || | Fabry disease | Angiokeratoma corporis diffusum—small dark red papules symmetrically in a “bathing trunk” distribution, ± mucosal involvement | Acral paresthesias, painful crises, hypohidrosis, whorl-like corneal and lenticular opacities, progressive renal and coronary artery disease, cerebrovascular accidents; X-linked recessive lysosomal storage disease due to α-galactosidase A deficiency |
| Fucosidosis | Angiokeratoma corporis diffusum (as described above) | Mental retardation, spastic paresis, seizures, recurrent sinus and pulmonary infections; AR lysosomal storage disease due to α- l -fucosidase deficiency |
∗ PHACE(S) and LUMBAR may occur in association with a “minimal growth” hemangioma with reticulated erythema, linear telangiectasias, and often small peripheral red papules.
† Midline lumbosacral capillary malformations are also occasionally associated with spinal dysraphism, usually when present together with another skin finding.
‡ Referred to as Servelle–Martorell syndrome.
§ Midfacial capillary stains have also been described in association with a variety of dysmorphic conditions, including Beckwith–Wiedemann, Roberts, and Rubinstein–Taybi syndromes.
|| Angiokeratoma corporis diffusum has also been reported in other lysosomal storage diseases such as galactosialidosis, GM1 gangliosidosis, and β-mannosidosis.
Infantile hemangiomas arise during the first few months of life and are the most common tumors of infancy, with an incidence of approximately 5% by 1 year of age and a female-to-male ratio of 3–4:1. Unlike other vascular tumors and malformations, infantile hemangiomas express the placental marker glucose transporter protein-1 (GLUT-1). These hemangiomas typically mark out their territory early on and subsequently expand in volume. The proliferative phase lasts until 3 to 9 months of age, with the most rapid growth in the first few months. This is followed by slow spontaneous regression during the involutional phase, which is complete by 3 to 10 years of age. Superficial hemangiomas are initially bright red in color and then become dull red to gray during involution, whereas deep hemangiomas are light blue in color and become softer and less warm as they involute. The term “cavernous hemangioma,” which has been used to describe both hemangiomas with a deep component and venous malformations, has led to confusion and should be avoided. Infantile hemangiomas can be complicated by ulceration, interference with the function of vital structures such as the eyes or airway, high-output cardiac failure, and problems related to associated regional structural anomalies ( Table 23-3 ; see Fig. 23-16 ). Hypothyroidism occasionally occurs in infants with large-volume proliferating hemangiomas, especially hepatic lesions, because of production of iodothyronine deiodinase within the tumors. In the past decade, use of the β-blocker propranolol has revolutionized the treatment of infantile hemangiomas that would otherwise threaten vital functions or result in disfigurement.

There are a variety of benign vascular tumors and reactive proliferations other than infantile hemangiomas ( Table 23-2 ). Congenital hemangiomas represent relatively uncommon, GLUT-1-negative vascular neoplasms that are fully formed at birth and have a natural history of either rapid involution during the first year of life or proportionate growth and failure to involute. These lesions typically present as a pink to blue-violet nodule or plaque with central coarse telangiectasias and peripheral pallor.
Cherry angiomas are small, bright-red papules representing a benign proliferation of capillaries; commonly seen on the trunk of adults, they increase in number with age. Pyogenic granulomas are rapidly developing vascular lesions that typically appear as friable papules on the face, fingers ( Fig. 23-7 ), or mucous membranes. Histologically resembling granulation tissue, pyogenic granulomas frequently occur at sites of minor trauma or on the gingiva during pregnancy.

Bacillary angiomatosis primarily affects patients with AIDS and most often presents as multiple red vascular papules and nodules; internal organ involvement, e.g., liver and bone, can also occur. The causative organisms, Bartonella quintana or B. henselae , can be seen with Warthin–Starry staining of tissue specimens. Kaposiform hemangioendotheliomas and tufted angiomas are two vascular tumors that can be complicated by Kasabach–Merritt syndrome, an acute, life-threatening consumptive coagulopathy with profound thrombocytopenia ( Table 23-3 ). Spindle cell hemangiomas are unusual tumors that typically develop within existing venous malformations and may be associated with Maffucci syndrome ( Fig. 23-8 ; Table 23-3 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here