Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Normal and effective spontaneous labor is dependent upon normal uterine physiology and careful watchful waiting without overly aggressive obstetric management. Dystocia is dysfunctional labor that often has complex origins, and may develop after the normal onset of labor or after the induction of labor for indicated reasons. Metabolic dysregulation before pregnancy or during pregnancy secondary to the mother's health are thought to contribute to the cause(s) of dystocia.
The uterus is a smooth muscle organ that undergoes dramatic changes to accommodate the developing fetus. Maternal, placental, and fetal hormones play important roles in preparing the uterus to accept a growing and maturing fetus, permitting labor to begin naturally, and allowing the fetus a safe passage and a timely delivery into its new external environment.
The Friedman labor curve has been the standard used for plotting the progress of labor as defined by cervical dilation over time. More recent studies suggest that the age of women on becoming pregnant has increased and their body mass index (BMI) before pregnancy is significantly higher. These factors, along with excessive weight gain during pregnancy, contribute to abnormalities in the progress of labor during the latent and the active phases. Thus, more attention and time must be spent observing women to avoid the risk of cesarean delivery. Newer parameters for defining dystocia have been proposed as a modification of the Friedman curve.
Recent studies of the pathogenesis of dystocia have focused on conditions that affect the metabolic dysregulation of normal myometrial function, such as infection and inflammation. These conditions are more common in overweight and obese women. Currently, vitamin D deficiency is related to muscle dysfunction and a greater risk of inflammation, and this deficiency may contribute to the cause(s) of abnormal dystocia.
Oxytocin for myometrial stimulation in patients with abnormal progress of labor should be used with caution. Other risk factors such as abnormal presentation, excessive size of the fetus (macrosomia), developmental abnormalities of the fetus, and maternal pelvic abnormalities that may increase the risk of dystocia should be recognized and appropriate management initiated. Current evidence indicates that conduction anesthesia does not increase the primary cesarean delivery rate.
Although the definition of dystocia is “difficult childbirth,” the term is used interchangeably with dysfunctional labor and characterizes labor that does not progress normally. Dystocia may be caused by (1) abnormalities of the “Powers,” such as ineffective coordinated contractility and uterine expulsive forces; (2) abnormalities of the “Passenger,” such as abnormal fetal lie, fetal macrosomia, malpresentation, malposition, or fetal anatomic defects or (3) abnormalities of the “Passage,” such as maternal bony pelvic contractures, resulting in mechanical interference with the passage of the fetus through the birth canal.
The cause or causes of abnormal labor should be determined as accurately as possible so that an effective and safe management plan can be developed. The purpose of this chapter is to provide the student with specific metrics that have helped obstetricians understand normal and abnormal labor.
The pregnant uterus is a large smooth muscle organ consisting of billions of smooth muscle cells. Each smooth muscle cell becomes a contractile element when the intracellular ionic calcium concentration increases to trigger an enzymatic process that results in the formation of the actin-myosin element. Stimulation of oxytocin and/or prostaglandin receptors on the plasma membrane of cells further activates the formation of the actin-myosin element.
Contractions occur in localized areas of the uterus during gestation, but during parturition the entire uterus contracts in an organized way to allow for birth. These coordinated smooth muscle contractions occur as a result of an increase in number and action of special gap junction structures. Gap junctions are protein channels that form along the interface of two smooth muscle cell membranes and act by promoting the movement of action potentials throughout the myometrium.
During labor, two distinct segments of the uterus are formed. The upper segment actively contracts and retracts to expel the fetus, while the lower segment, along with the dilating cervix, becomes thinner and passive and is referred to as the lower uterine segment (LUS).
The pregnant cervix contains collagen, small amounts of smooth muscle, and ground substance and must be structurally altered from a firm, intact sphincter to a soft, pliable, dilated structure through which the fetus can pass at the appropriate time. The collagen fibers are helical strands of amino acids in an intracellular protein matrix of glycosaminoglycan branches (GAGs). The GAGs determine the amount of aggregation of the collagen fibers. Cervical softening involves two changes in the intracellular matrix: a reduction in the number of collagen fibers and an increase in the GAGs, and later decreasing fiber aggregation. Several hormones are known to affect cervical softening including prostaglandins (PGs) and relaxin . Prostaglandin E2 (PGE2) is considered the major hormone causing cervical softening and an increased production of PGE2 coincides with reductions in progesterone levels before parturition. The increase in PGE2 also acts to increase uterine myometrial contractions and uterine pressure and to stimulate the cervix at the onset of labor.
Labor is diagnosed by regular, painful uterine contractions that increase in frequency and intensity with progressive cervical effacement or dilation.
In early latent phase labor, the cervix softens and effaces with minimal dilation. This is followed by a more rapid active phase of dilation, which is further subdivided into the acceleration (maximum slope) and deceleration phases. The descent of the fetal presenting part usually begins during the active phase, accelerating toward the end of the active phase, and climaxing after the cervix is completely dilated. A useful method for assessing the progress of labor and detecting abnormalities in a timely manner is to plot the rate of cervical dilation and descent of the fetal presenting part ( Figure 11-1 ).
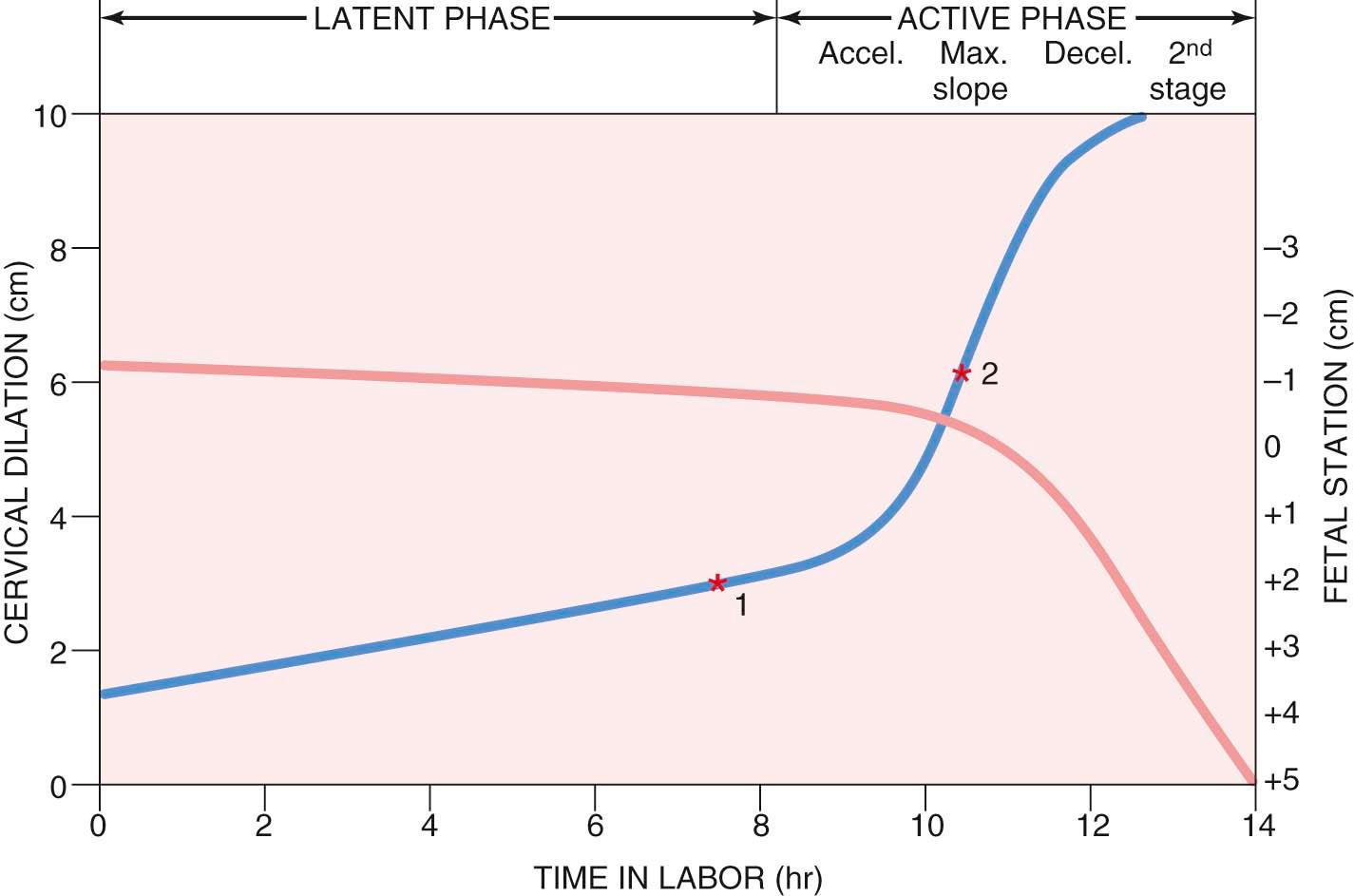
Normal cervical dilation and descent of the fetus take place in a progressive manner and occur within a well-defined time period. Dysfunctional labor occurs when rates of dilation and descent exceed these time limits. The phase of labor and the configuration of the abnormal labor curve may indicate the potential causes for the abnormal labor.
The normal limits of the latent phase of labor extend up to 18 hours for nulliparous patients and up to 10 hours for multiparous patients (see Table 8-5 ). A latent phase that exceeds these limits is considered prolonged and may be caused by dysfunctional labor, premature or excessive use of sedatives or analgesics, fetal malposition, or abnormal fetal size. A long, closed, firm cervix requires more time to efface and to undergo early dilation than does a soft, partially effaced cervix, but it is doubtful that a cervical factor alone causes a prolongation of the latent phase. Many patients who appear to be developing a prolonged latent phase are shown eventually to be in false labor or prelabor, with no progressive dilation of the cervix.
The outcome of a prolonged latent phase is generally favorable for both the mother and the fetus, provided that no other abnormalities of labor subsequently occur.
A prolonged latent phase caused by premature or excessive use of sedation or analgesia usually resolves spontaneously after the effects of the medication have worn off. Therapeutic rest with morphine sulfate or an equivalent drug has been shown to be an effective therapeutic option for women in prolonged latent phase, with about 62% being subsequently admitted in labor, particularly those at term with >50% effacement, about 29% being discharged not in labor, and about 9% being admitted for category II fetal heart rate tracings for continued assessment. Thus, women in true labor wake up in active labor, while those in prelabor stop contracting and can be discharged
If a definitive diagnosis of prolonged latent phase of labor has been made and there are medical reasons to expedite delivery, augmentation of labor by oxytocin may be performed. This is accomplished by the addition of 20 U of oxytocin to 1 L of lactated Ringer solution. A number of protocols have been suggested for the infusion of oxytocin. Oxytocin can be given as “low dose,” where the infusion is begun at a rate of 1.0 to 2.0 mU/min and is increased by 1 to 2 mU/min increments every 15 to 40 minutes until the desired frequency and intensity are obtained, or a maximum of 20 to 40 mU/min has been reached. The “high dose” infusion method is begun at a rate of 4 to 6 mU/min with incremental increases of 4 to 6 mU/min every 15 to 40 minutes until uterine contractions of the desired frequency and intensity are obtained or a maximum of 40 mU/min has been reached.
Amniotomy or artificial rupture of the membranes may be considered as part of the management of the latent phase of labor; however, recent data suggest that amniotomy is associated with an increased risk of cesarean delivery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here