Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Urology is the surgical specialty that focuses on the diagnosis and management of conditions and diseases of the genitourinary system in adults and children and of the reproductive system in the male. Of the surgical subspecialties, urology shares the most in common with general surgery because of our operative approaches and techniques in the abdomen, retroperitoneum, pelvis, and genitalia. Like general surgeons, urologists treat patients with open, laparoscopic, robotic, endoscopic, and microsurgical techniques. Frequently, urologists and general surgeons collaborate in the care of patients across our many interdisciplinary subspecialties. Examples of this include major trauma surgery, exenterative surgery for advanced abdominal and pelvic malignancies, and management of iatrogenic urologic and surgical injury and necrotizing infections of the genitalia and perineum.
General surgeons will encounter patients with urologic conditions as either presenting symptoms or as comorbidities to their general surgical diseases. Urology itself includes multiple subspecialties and treats a wide range of patients and diseases spanning pediatrics, stone disease, female pelvic medicine, oncology, and andrology, to name a few. The intent of this chapter is to give the practicing surgeon and trainee a broad overview of the field of urology and to impart a fundamental knowledge of our field to assist in our common goal of providing complete surgical care of the patient.
The organs of the genitourinary system span the entire retroperitoneum, pelvis, inguinal region, and genital region. Because of the close anatomic relationships of the organs in the abdomen and retroperitoneum, general surgeons must be familiar with all of the urologic organ systems to prevent iatrogenic injury and to deal with variations in normal anatomy. These challenges arise in many fields of surgery, including vascular, oncology, and colorectal surgery.
Beginning at the most superior aspect of the retroperitoneum lie the adrenal glands. These small, paired organs have two different embryologic origins and serve a primary endocrine function. The adrenal glands are composed of the cortex and medulla and are fused after development. The cortex is the outer layer of the adrenal gland and is derived from mesoderm. On cross section, the layers, from external to internal, are the zona glomerulosa, zona fasciculata, and zona reticularis. The different zones secrete various steroid-derived hormones including mineralocorticoids (glomerulosa), glucocorticoids (fasciculata), and sex steroids (reticularis). The adrenal medulla is derived from neural crest cells and is directly innervated by presynaptic sympathetic fibers. The medulla is responsible for secreting catecholamines in response to sympathetic stimulation. The adrenal glands lie within Gerota fascia and have an orange-yellow appearance and an area of usually 3 to 5 cm in transverse diameter. The arterial supply is through three sources: superior—inferior phrenic; medial—abdominal aorta; and inferior—ipsilateral renal artery. The venous drainage does not mirror the arterial supply; on the right, the single adrenal vein drains to the vena cava, whereas on the left, the adrenal vein drains into the left renal vein. Supernumerary veins can exist on either side because of anatomic variation. The adrenal glands are anatomically distinct from the kidney, although there are ventral and dorsal fascial investments that connect it to the kidney. The anatomic relations to the right adrenal gland are the vena cava on the anteromedial aspect and the liver and duodenum on the anterior aspect of portions of the adrenal gland. On the left, the pancreas and splenic vein are anterior to the cortical surface.
The kidneys are the next paired organs just inferior to the adrenal glands. These organs are completely enveloped within the perirenal fascia (Gerota fascia) and are mobile structures supported only by the perirenal fat, renal pedicle vasculature, and abdominal muscles and viscera. Although Gerota fascia separates the kidney capsule and parenchyma from these adjacent organs and reduces the risk of renal injury with local dissection, renal parenchymal injury is possible with abnormal anatomy. The kidneys are approximately the size of a closed fist, measuring 10 to 12 cm in length and 5 to 7 cm in width. The right kidney typically lies slightly more inferiorly than the left kidney because of its position beneath the liver. Despite being located in the retroperitoneum, the kidney is well protected from external injury by the surrounding muscular and skeletal structures. Posteriorly, each kidney is covered by the diaphragm on the upper third of its surface and is crossed by the twelfth rib. The inferior aspect of the kidney is adjacent to the psoas muscle medially and the quadratus lumborum and transversus abdominis laterally. The anterior surfaces of the kidneys are intimately related to several intraperitoneal structures. On the right, the liver is attached to the kidney by the hepatorenal ligament, and the anterior upper pole is adjacent to the peritoneal surface of the liver. The duodenum lies on the medial aspect of the anterior right kidney, typically on the hilar structures. The hepatic flexure of the colon crosses anterior to the inferior pole of the right kidney. On the left, the superior pole of the kidney lies posterior to the tail of the pancreas and the splenic vessels and hilum. The spleen is situated anteromedial to the kidney and is directly attached to the kidney by the lienorenal ligament. The splenic flexure of the colon is draped over the caudal aspect of the anterior left kidney.
The renal vasculature has significant variability occurring in 25% to 40% of kidneys. The typical vasculature is based on a paired artery and vein supplying the kidney as direct branches of the aorta and vena cava, respectively. The renal artery branches from the aorta inferior to the superior mesenteric artery at the level of the second lumbar vertebra. The renal artery then branches into four or five segments, each being an end artery. The renal arteries are located posterior and slightly superior to the renal veins. The artery initially branches posteriorly into the posterior segmental artery. The anterior branches are variable but include the apical, upper, middle, and lower segmental arteries. These arteries branch multiple times within the cortical kidney, creating a complex filtration mechanism at the capillary level. The venous capillary branches coalesce to mirror the parenchymal arterial system. Renal segmental veins are not end vascular structures and collateralize extensively. The renal vein on the right is short, typically 2 to 4 cm in length, and enters the posterolateral inferior vena cava. The left renal vein is longer, 6 to 10 cm, and travels anterior to the aorta and inferior to the superior mesenteric artery and enters the left lateral vena cava. The left renal vein also is the common entry point for the left adrenal vein, gonadal vein, and a lumbar vein. Renal ectopia is accompanied by markedly variable and unpredictable renal vasculature, with multiple branches arising from the iliac arteries or aortic bifurcation.
The upper collecting system begins within the renal parenchyma at the level of the papilla. The papillae coalesce to become the minor calyces, which, in turn, become the major calyces. The major calyces converge to form the renal pelvis. The ureter begins at the inferior aspect of the renal pelvis, where it narrows to become the ureteropelvic junction posterior to the renal artery. Each ureter is typically 22 to 30 cm in length, depending on height, and courses through the retroperitoneum into the pelvis, where it connects to the urinary bladder at the ureterovesical junction. At its origin, the ureter courses along the anterior psoas major muscle and is crossed by the gonadal vessels bilaterally. The ureters cross over the iliac vessels to enter the pelvis, just superior to the bifurcation of the iliac vessels into the internal and external segments. Once in the pelvis, the ureters course medially to enter the bladder. The ureters are divided into three segments, upper, middle, and lower, using this anatomic landmark as a junction point. The upper segment runs from the ureteropelvic junction to the superior margin of the sacrum. The middle segment runs over the bony pelvis. The lower segment begins at the inferior margin of the sacrum and continues into the bladder. The ureteral lumen is not uniform throughout its length and has three distinct narrowing points: the ureteropelvic junction, crossing the iliac vessels, and the ureterovesical junction. The right and left ureters have separate anatomic relationships (peritoneal and retroperitoneal structures). On the right, the ureter is posterior to the ascending colon, cecum, and appendix. The left ureter is posterior to the descending and sigmoid colon. In the male, the ureters are crossed by the vasa deferentia as they emerge from the internal ring before turning medially to join the prostate. The ureteral blood is drawn from multiple vessels throughout its course and within the adventitia; the arterial vessels create an anastomosing plexus. In general, the upper ureteral segments have a medial vascular supply (i.e., renal artery and aorta), and the lower ureteral segments have a lateral vascular supply (i.e., internal iliac and various branches). This unique collateral blood flow allows extensive mobilization of the ureter, outside of its adventitia, without loss of its blood supply.
The ureter is best identified, intraoperatively, in an area of normal anatomy and then followed to the area of concern. This is readily accomplished medial to the lower pole of the kidney or at the iliac bifurcation. After prior surgery or retroperitoneal disease processes, any of these rich collateral blood supply sources may not be contributory; thus, to minimize the risk of surgical devascularization, it is critical to avoid unnecessary extensive circumferential dissection of the ureter or dissection of the ureter in the subadventitial plane.
The bladder, the end reservoir for urine, is located within the inferior pelvis. The bladder, when empty, is located behind the pubic rami; but as the bladder becomes distended, the superior aspect of the bladder extends out of the pelvis and into the lower anterior abdomen. The bladder can be injured on entering of the abdomen through a midline incision in the retropubic space (of Retzius) if the bladder is not displaced posteriorly when the midline rectus fascial incision is extended to the pubis. Superiorly, the bladder is covered by the parietal peritoneum of the pelvis as the peritoneum reflects off the anterior and lateral abdominal walls. The anterior and lateral bladder walls do not have a peritoneal surface but reside within pelvic fat and lie along the musculature of the pelvic side wall or pubis anteriorly. Prior lower abdominal or pelvic surgery can change the anatomic relations of the bladder and cause it to be affixed abnormally within the pelvis. The bladder has a unique cross section with a urothelial lining creating a tight barrier from urine and a central muscular detrusor layer involved in the excretory function of the bladder. Branches of the internal iliac artery, the superior and inferior vesical arteries, supply blood to the bladder. Similar to the ureter, the bladder has a rich collateral vascular network, so ligation or damage to an artery is not detrimental to the bladder. The innervation of the bladder is important because of the excretory function of the bladder. The bladder has autonomic and somatic innervation with a dense neural network to the brain. The sympathetic innervation to the bladder is through the hypogastric nerve, and the parasympathetic supply is through the sacral cord and pelvic nerve. The anatomic relationships of the bladder differ between male and female patients. In the male patient, the posterior bladder wall is adjacent to the anterior sigmoid colon and rectum. Prior pelvic surgery, irradiation, or pelvic trauma can make the plane between these structures difficult to define, resulting in inadvertent injury. In the female patient, the parietal peritoneum becomes contiguous with the anterior uterus, and the superior bladder lies against the lower uterus while the bladder base sits adjacent to the anterior vaginal wall. The spherical bladder funnels caudally into the bladder neck, and this becomes the tubular urethra inferiorly.
In the male patient, the first segment of the urethra is surrounded by and integrated into the prostate. The prostate, an endocrine gland involved with male reproductive function, is located immediately inferior to the bladder and invested in the circular fibers of the bladder neck. The prostate is surrounded by the lateral pelvic fascia on its anterior surface, by endopelvic fascia on its lateral surface, and by Denonvilliers fascia posteriorly. The rectum sits immediately posterior to the prostate and is separated by a second layer of Denonvilliers fascia. This fascia also extends superiorly on the posterior prostate to encompass the seminal vesicles. The seminal vesicles are the reservoirs for seminal fluid that makes up the majority of the ejaculatory fluid. The arterial supply to both structures is through branches of the inferior vesical artery. The venous drainage mirrors the arterial supply, draining through the inferior vesical veins and subsequently into the internal iliac veins. In addition to the rectum, the other major anatomic relationship of the prostate is Santorini plexus, a network of veins derived from the dorsal venous complex of the penis.
The drainage of urine from the bladder is through the tubular urethra, which begins at the level of the bladder neck. In male patients, the urethra has five distinct segments: prostatic, membranous, penile, bulbar, and glandular (also known as the fossa navicularis). The prostatic and membranous urethra is surrounded by striated muscle, and when the urethra penetrates the genitourinary diaphragm in the perineum, the outer layer becomes spongy, vascular tissue. Within the prostate, the ejaculatory duct opens into the urethra and serves as the exit point for seminal emission. The blood supply of the extraprostatic urethra is through the common penile artery, which is a branch of the internal pudendal artery. The venous drainage of the urethra is through the circumflex penile veins and ultimately into the deep dorsal vein of the penis. The major surrounding structure in the proximal male urethra is the rectum, which sits posterior to the proximal bulbar segment. The female urethra is more regular in length and is approximately 4 cm long. The female urethra contains three distinct layers as opposed to the male urethra. The proximal urethra is surrounded by smooth and striated musculature, which forms the urinary sphincter. The arterial and venous blood supply are through the internal pudendal, vaginal, and inferior vesical veins. The only structure adjacent to the female urethra is the anterior vaginal wall.
The male external genitalia consist of the penis, scrotum, and paired testes. The penis consists of three circular erectile bodies: the two dorsal corpora cavernosa and the ventral corpus spongiosum. The corpora cavernosa are responsible for penile erection; the corpus spongiosum provides support and structure to the urethra. Blood supply of the penis is through the external and internal pudendal arteries. The external pudendal artery supplies the penile skin; the internal pudendal artery supplies the urethra and the paired erectile bodies. The venous drainage of the penis is through the superficial and deep dorsal veins and the cavernosal veins. The penis is entirely an external structure, with all three erectile bodies terminating in the perineum. The scrotum is a surprisingly complex structure consisting of a muscular sac covered with a unique epidermal layer with no fat but many sebaceous and sweat glands. The sac is divided into two halves by a midline septum of dartos muscle. The blood supply to the scrotum is through the external pudendal arteries anteriorly and branches of perineal vessels posteriorly. Within the scrotum are the right and left testicles. The testicles have both endocrine and reproductive function in men. Typically, the testes are 4 to 5 cm long and 3 cm wide. The vascular and genital ductal structures leave the testis from the mediastinum in the posterosuperior portion and travel through the scrotal neck into the inguinal canal. The spermatic cord is invested by the internal spermatic fascia, cremaster muscle, and external spermatic fascia, which are derived from the transversalis fascia, internal oblique, and external oblique, respectively. Arterial blood supply is primarily through the testicular or gonadal artery, which is a direct branch from the aorta inferior to the renal artery. Secondary blood supply to the testicle is through the cremasteric and vasal arteries. The venous drainage of the testicle initially begins as a pampiniform plexus coalescing into the gonadal or testicular veins. On the right, the vein drains directly into the vena cava; on the left, the vein drains into the left renal vein. The testicles are also responsible for spermatogenesis and for testosterone production. After production, the spermatozoa exit through a series of ductal structures that emerge into the rete testis, efferent ductules, epididymis, and ultimately the vas deferens. The epididymis is located posteriorly and slightly lateral to the testis. The spermatic artery, vein, and vas deferens are invested together in the fascial structures of the spermatic cord. The spermatic cord travels through the external inguinal ring through the inguinal canal and then into the pelvis through the internal inguinal ring. The spermatic cord is susceptible to injury during inguinal dissection for hernia repair, especially in redo cases, when it may be encased in fibrosis and injured without recognition. Significant injury to the spermatic cord may put the viability of the testis at risk, even though it is supported by three collateral arteries. The perineum is divided into an anterior and posterior triangle in the male by a line connecting the ischial tuberosities. The posterior perineal triangle contains the anus and internal and external sphincters. The anterior triangle (or urogenital triangle) contains the corpus spongiosum and proximal aspect of the paired erectile bodies, the corpora cavernosa. The layers deepening towards to the corpus spongiosum consist of the skin, subcutaneous fat, Colles fascia, and bulbospongiosus muscle (surrounding the corpus spongiosum) and ischiocavernosus muscles (surrounding the corpora cavernosa). The blood supply to this region is based on branches of the internal pudendal artery, and drainage is through the internal pudendal vein. The presence of a urethral catheter is helpful in palpating the location of the urethra, but the corpus spongiosum surrounding the bulbar urethra is still vulnerable to injury with dissection in an inflamed or obliterated anatomic plane.
Urologists were early adopters of endoscopic surgery and began evaluating the urethra and bladder with cystoscopy in the early part of the twentieth century. The first diagnostic and therapeutic endoscopic procedures were performed for treatment of urologic disease processes. Endoscopic procedures are divided based on intervention or evaluation of the lower or upper urinary tract as each has specialized procedure-specific equipment.
Cystoscopy, or cystourethroscopy as it is formally called, is used for evaluation of the urethra and the bladder. Cystoscopic procedures are typically performed to evaluate the lower urinary tract in the setting of hematuria, voiding symptoms, recurrent infections, or bladder outlet obstruction; for surveillance in the setting of malignant neoplasms; and for removal of genitourinary foreign bodies and assessment of suspected trauma. Furthermore, cystoscopy can be used to perform diagnostic evaluation of the upper urinary tract with use of ureteral catheters and instillation of contrast material, which is visualized within the collecting system by fluoroscopy. Cystoscopy can be performed with both rigid and flexible endoscopes, each with certain benefits and advantages. Endoscopes are sized with the “French” (Fr) size system, which refers to the outer circumference of the instrument in millimeters. The rigid endoscope uses optical lens systems, similar to laparoscopes, and has excellent resolution. The inflexible structure is intuitive and easy to orient. Rigid cystoscopes have a range of sizes typically from 16 Fr to 26 Fr; surgical endoscopes, or resectoscopes, have the largest size of 24 Fr to 26 Fr. Rigid endoscopes have a larger luminal diameter, which allows greater irrigation flow, improving visualization and passage of a number of working instruments. Rigid lower tract endoscopy is more difficult to perform in the awake patient, although it is much better tolerated in the female patient than in the male patient because of the short, straight urethra in the female patient. Flexible endoscopes are smaller, 15 Fr or 16 Fr, and better tolerated by patients for examination. Both male and female patients can be examined with local anesthesia, usually consisting of lidocaine jelly instilled per urethra. The flexible endoscope does not require any specific patient positioning and can be used supine and at the bedside. Finally, because of the large deflection radius, the bladder is easily evaluated without changing the lens or patient position. The optics of flexible endoscopes continue to improve by advancements in camera chip capability, with new digital platforms approaching the resolution of optical lens systems. Pediatric endoscopes are smaller, 8 Fr to 12 Fr, and are typically used in the operating room.
Upper tract evaluation is performed with either a ureteroscope or a nephroscope. The most common reason for either procedure is management of calculous disease, both ureteral and renal. Ureteroscopy can also be used to visualize and to inspect the upper collecting system, ureter, and renal pelvis; for hematuria originating from the upper urinary tract; for surveillance of urothelial carcinoma; and for treatment or biopsy of abnormal findings. Ureteroscopy is performed with both flexible and semirigid endoscopes, each with different benefits and purposes. Semirigid endoscopes are 6 Fr to 7.5 Fr at the tip and gradually enlarge to 8 Fr to 9.5 Fr. The taper at the tip allows introduction into the ureteral orifice at the trigone of the bladder. These endoscopes have larger working channels that allow greater irrigation flow and a larger field of view. Because semirigid ureteroscopes are fairly inflexible, they are used to evaluate and to treat conditions below the level of iliac vessels and mid and distal ureter. Flexible ureteroscopes are 5.3 Fr to 8.5 Fr at the tip and gradually enlarge to 8.4 Fr to 10.1 Fr. The major advantage of flexible ureteroscopes is the deflection of the tip, which ranges from 130 to 250 degrees in one direction and 160 to 275 degrees in the opposite direction, with newer endoscopes approaching 360-degree deflection. In addition, these endoscopes can be advanced through ureteral tortuosity and over external compression, such as the psoas muscle. The working channel on the flexible ureteroscope is typically smaller because of the fiberoptic system, and introduction of instruments, such as baskets or laser fibers, reduces irrigation flow. These flexible endoscopes can be used throughout the upper urinary tract but are particularly useful in the proximal ureter and renal pelvis and calyceal system.
The other method of upper tract endoscopy is through direct percutaneous access but puncture through the renal parenchyma into the renal collecting system. Percutaneous nephroscopy is most commonly used to treat large renal calculi. Management of upper tract urothelial tumors with fulguration and resection may also be performed via percutaneous nephroscopy. Nephroscopy may be performed with both rigid and flexible nephroscopes; however, most intervention is performed with the rigid system. The rigid nephroscope is placed through a percutaneous working access sheath, similar to a laparoscopic trocar, to visualize the stone or tumor. Rigid nephroscopes are usually 25 Fr to 28 Fr, and their appearance is similar to a rigid cystoscope, although they have a fixed lens system rather than an exchangeable lens. There is also growing enthusiasm for “mini-perc” approaches, which involve smaller caliber instrumentation. Newer rigid nephroscopes are built on a digital platform that allows a larger working channel with comparable optics to a standard endoscope. Various intracorporeal lithotripters are placed through the working channel to fragment large stones into manageable pieces. Flexible nephroscopes are essentially flexible cystoscopes that are dual purposed for evaluation of the kidney. Flexible endoscopy of the upper tract is advantageous because all areas of the upper collecting system (upper, mid, and lower pole calyces) can be inspected regardless of angle or direction of the internal infundibula. At times, combined use of retrograde flexible ureteroscopy and percutaneous nephroscopy, in the prone patient under anesthesia, may be necessary to address complex renal anatomy for stone-related and other indications.
Numerous working elements are used in both upper and lower tract endoscopy. Guidewires are commonly used to access the upper urinary tract collecting system or the bladder and serve as guides to pass catheters, stents, and sheaths. Most guidewires have a flexible tip and a more rigid shaft and are constructed of an inner core and an outer covering, which may be hydrophilic or neutral (polytetrafluoroethylene). Guidewires range in size from 0.018 to 0.038 inch and have various lengths. Urethral catheters and ureteral catheters may be placed over wires to assist with direct placement into the lower or upper urinary system, respectively. Ureteral stents are hollow catheters with flexible ends that form a coil on the proximal and distal ends to maintain position within the collecting systems. Stents are placed to ensure drainage of the kidney and to bypass blockages of the ureter from inflammation, stones, or tumors. Many stents are composed of thermodynamic material, which becomes softer at higher body temperatures. Stents range in size from 4.8 Fr to 10 Fr and have various lengths to accommodate variable ureteral lengths. Ureteroscopic baskets are used to remove ureteral and renal calculi and to perform extraction and biopsy of tumors. These range in size from 1.3 Fr to 3.2 Fr and are constructed of flexible material to allow placement into various calyceal locations within the kidney.
Urinary tract infections (UTIs) are a common medical problem, although patients with UTI referred to urologists for evaluation and treatment often have a complicated or unusual element to their diagnosis or management. Other infections treated by urologists include infections of the genital skin (a spectrum of disease from skin neoplasms, to cellulitis, to necrotizing fasciitis) and reproduction organs in men (i.e., orchitis, epididymitis, or prostatitis). Furthermore, these infections may require simple antibiotic therapy, multimodal treatment with surgical drainage, or debridement and management in an intensive care setting. Urinary tract obstruction with proximal infection may result in sepsis, challenging the skills of the urologist and surgical critical care specialist.
Recent literature indicates that UTIs in adult women and men accounted for 39 million office visits and 6 million emergency department visits. In adult patients, more than 50% of women and 12% of men will develop a UTI during their lifetime. Urinary infection is considered “uncomplicated” when it occurs in the immunocompetent host, without underlying anatomic or physiologic abnormalities of the urinary tract in women. UTI diagnosed in men is generally considered “complicated”. For diagnosis of a UTI, a clean catch, midstream urine specimen is preferred, and on culture, 10 5 colony-forming units must be demonstrated. In catheterized specimens, UTI can be diagnosed with as little as 10 3 colony-forming units. The typical symptoms associated with UTI are dysuria, frequency, urgency to void, and malodorous urine. Because of the inherent differences in etiology, evaluation, and treatment, uncomplicated UTIs are divided into those occurring in premenopausal and postmenopausal women. A third category of uncomplicated UTI, that occurring in pregnant patients, is beyond the scope of this overview. In general, risk factors include genetic, biologic, and behavioral; specific aspects are discussed with each group.
History and physical examination of patients in this age group presenting with symptoms of UTI are particularly important because of overlapping disease processes. In patients without vaginal discharge, the majority can be expected to have a UTI as the diagnosis. However, in sexually active women, sexually transmitted infections (STIs) must be considered, especially in the setting of a negative urine culture. Furthermore, in patients with vaginal discharge, vaginitis caused by yeast, trichomoniasis, and bacterial vaginosis are possible causes. Risk factors for UTI in this population of patients include frequent sexual intercourse, initial UTI at a young age, maternal history of UTI, and number of pregnancies and deliveries. Important aspects of the physical examination in these patients include palpation of costovertebral tenderness (assessing for ascending infection) and pelvic examination to evaluate for STI. The most common cause of infection in these patients is Escherichia coli (80%–85%), followed by Staphylococcus saprophyticus (10%–15%) and Klebsiella pneumoniae and Proteus mirabilis (4% each). Empirical therapy is acceptable, although confirmatory urine cultures are useful as the incidence of antibiotic resistance continues to rise. Prevention includes increased hydration and evaluation of hygiene practices.
As in younger patients, history and physical examination are important aspects of UTI evaluation in this group of patients. Presenting symptoms are similar in this group, although some elderly patients may simply present with altered mental status. Furthermore, an important component in diagnosis and treatment of postmenopausal women is the change in the vaginal pH levels and change or reduction in lactobacillus in the vaginal flora. The physical examination findings may differ in these patients as STIs are less likely but physical changes, such as pelvic organ prolapse and incomplete bladder emptying, become causative factors. In addition, the pathologic bacterial species are different. E. coli continues to be the predominant organism but in this age group, P. mirabilis, K. pneumoniae , and Enterobacter species become more prevalent pathogens. Again, empirical therapy is acceptable, but urine cultures are important because of increasing antibiotic resistance patterns and differing organisms. Prevention includes increased hydration and evaluation of hygiene practices.
“Complicated” UTIs require more vigilance on the part of the treating physician because of patient factors that may lead to a more rapid progression or worsening of the infection. By definition complicated UTIs occur in men and in patients with diabetes, immunosuppression, upper tract infection, resistant organisms, urinary tract anatomic abnormalities, prior surgery, calculous disease, spinal cord injury, or recent or current indwelling Foley catheter. Essentially, any abnormality of physiology or anatomy which is etiologic in a UTI or a UTI that occurs in such a setting or in the immunocompromised patient is considered “complicated.” In these patients, similar evaluation is warranted, but the evaluation should not be limited to simply history and physical examination. Empirical treatment of complicated UTI alone is not optimal, and urine cultures should be performed on all patients with suspected complicated UTI before initiation of antibiotic therapy, whenever possible. In addition, imaging is indicated in these patients because of concern for calculous disease and urinary stasis, so at a minimum, simple radiography of the kidneys, ureters, and bladder (a KUB study) and renal ultrasound, and potentially further assessment with cross-sectional radiographic imaging should be performed in patients with equivocal or concerning findings. Finally, antibiotic therapy alone may not be adequate, and these patients may require surgical drainage of obstructed urinary systems or later surgical correction of anatomic abnormalities or removal of urinary stones (once infections are treated) to prevent recurrent UTIs. Consultation with infectious disease specialists may also be indicated in patients with urologic anatomic abnormalities and recurrent UTIs with resistant organisms.
Because of the lower incidence of UTI in men, when men present with symptoms of infection, it is always considered complicated, regardless of other patient factors. As in women, younger men (younger than 50 years) and older men (older than 50 years) have different causes of their UTI and symptoms. Common presenting symptoms are urethritis, dysuria, hesitancy, frequency, and urgency of urination. A history and physical examination in these patients are important to delineate different sources of symptoms or UTI. Men can present with these symptoms and have different diagnoses, including UTI, STI, urethritis, and chronic pelvic pain. Furthermore, bacterial infections can extend to other proximal areas of the genitourinary system, such as the prostate and testicle. Men younger than 50 years are more likely to have STI as the cause rather than UTI. These men should have a thorough sexual history, genital examination, and microscopic urinalysis performed. Urethral swab or urine tests for STI should be performed as well. Men older than 50 years often have underlying lower urinary tract symptoms (LUTS), and this can be a contributing factor. Men in this age group more frequently will have UTI as a source of their symptoms, and common urinary pathogens, as in women, should be considered. Furthermore, older men should be questioned about recent surgical procedures, catheterization, or hospitalization. Elderly patients can also present with mental status or behavioral changes as their only symptom of UTI, and this diagnosis must be considered in these patients. A lower threshold for imaging and hospital admission is necessary in men with UTI as they may present with more systemic symptoms. Patients who cannot tolerate oral intake, are immunocompromised, or have medical comorbidities should be admitted with cross-sectional imaging performed. Broad-spectrum intravenous antibiotics, based on local resistance patterns, and fluid resuscitation should be initiated in these patients while the initial workup and evaluation are completed. Urinary obstruction or stone disease in these patients constitutes a urologic emergency and must be addressed rapidly.
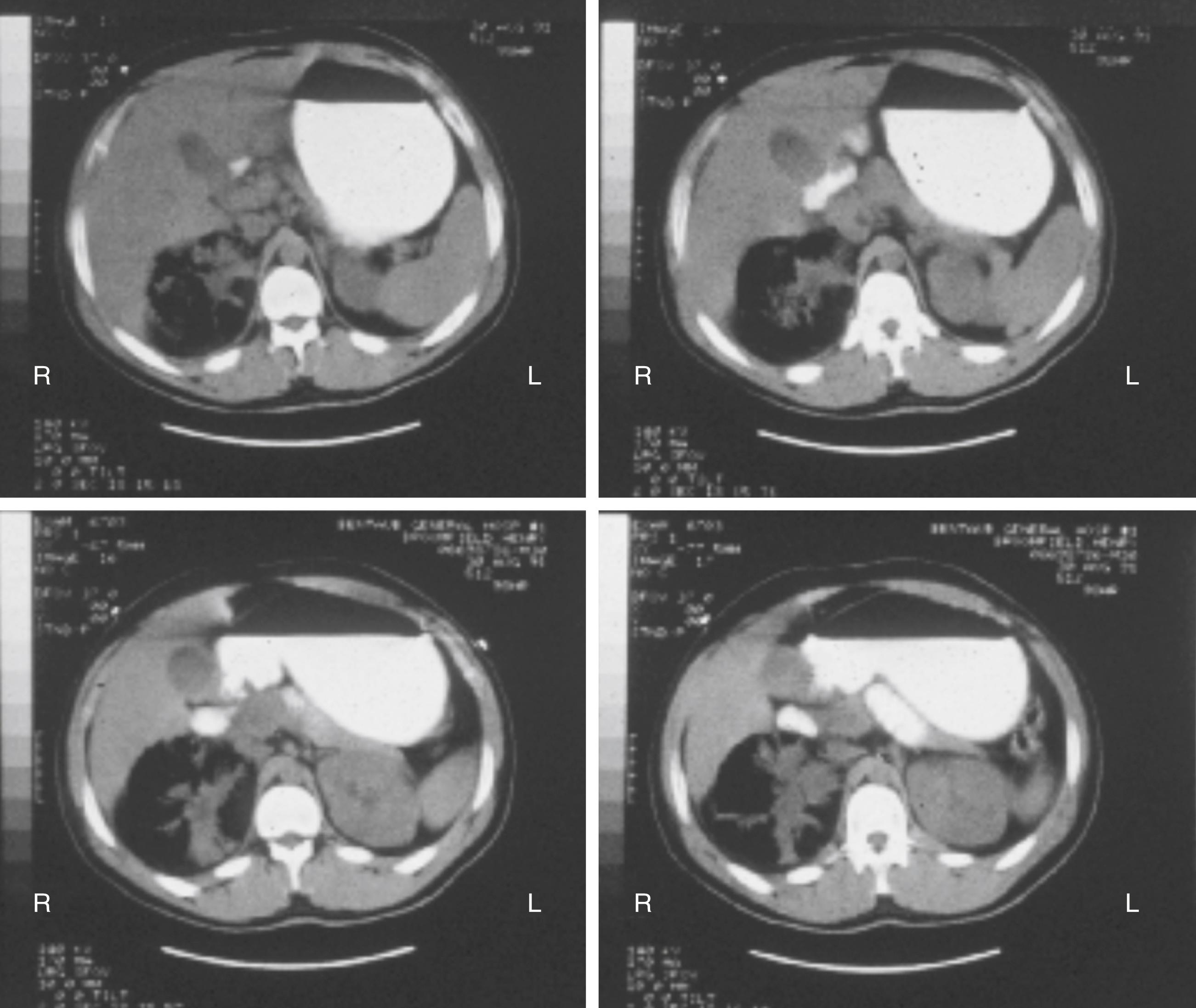
Pyelonephritis is a spectrum of infectious or inflammatory processes that involve the kidney collecting system or parenchyma. Pyelonephritis results from a UTI moving proximally upward from the lower urinary tract. In the simple form, pyelonephritis may be treated on an outpatient basis with oral antibiotics for 1 to 2 weeks. In this group of patients, urine culture is necessary to identify the causative organism. If the patient appears more acutely infected, hospitalization may be warranted for broad-spectrum intravenous antibiotic therapy, fluid resuscitation, and cross-sectional imaging. Emphysematous pyelonephritis represents an advanced form of pyelonephritis and is considered a urologic emergency. Often occurring in the diabetic patient, these uncommon infections demonstrate a significant necrotizing infection of the kidney with gas-forming organisms (typically E. coli in a facultative anaerobic metabolic state) with pockets of gas within the parenchyma apparent on imaging ( Fig. 74.1 ). The common bacterial pathogens include E. coli , P. mirabilis, and K. pneumoniae . These patients require either prompt percutaneous drainage of the infection or rapid nephrectomy. Most patients who present with this condition are diabetic or have significant medical comorbidities, and control of the metabolic abnormalities, aggressive broad-spectrum antibiotic therapy, and supportive critical care are essential. Xanthogranulomatous pyelonephritis is a chronic infectious process resulting from renal obstruction, recurrent infection, and renal calculous disease. The disease presents in three forms, focal, segmental, or diffuse, and each is treated in a different manner. The underlying histologic process involves a foamy, lipid-laden, macrophage infiltrate in the renal parenchyma with extensive inflammation, fibrosis, and loss of renal function. On imaging, there may be indications of collecting system dilation; however, drainage attempts often are unproductive because the material is often solid or too viscous to drain. Patients with focal or segmental disease may be treated with antibiotics, but those with diffuse disease frequently require nephrectomy. The risk of iatrogenic adjacent organ injury is high in these nephrectomies, and the renal hilum may be so inflamed and fibrotic that the renal vessels cannot be individually dissected. These cases may require placement of a vascular pedicle clamp with renal excision and oversewing of the pedicle.
UTIs may ascend into the genital ducts, resulting in infection of the prostate, epididymis, or testicle. Beginning in the urethra, the verumontanum is the exit point of the seminal vesicles and vas deferens into the urinary tract. Prostatitis refers to any inflammatory process affecting the prostate, but the general surgeon more commonly may encounter acute bacterial prostatitis, which results from bacterial infiltration into the prostatic parenchyma. Most infections of the prostate are secondary to gram-negative bacterial infection and typically are associated with UTI. Two important considerations in these patients are physical examination and disease extent. Although a full history and physical examination are warranted, elimination of digital rectal examination (DRE) should be considered as pressure exerted on an infected prostate may lead to hematogenous spread of the bacteria. In addition, patients who do not have reasonably rapid resolution of their symptoms should be evaluated for prostatic abscess. Prostatic abscesses typically do not respond to antibiotic therapy and require transurethral unroofing to allow adequate drainage.
Epididymitis-orchitis results when the UTI ascends through the vas deferens into the epididymis or testicle. Again, the cause is different according to the patient’s age; men younger than 35 years typically have an STI as a source, commonly Chlamydia trachomatis, whereas men older than 35 years will often have infections related to E. coli . Examination of these patients is often difficult because of significant swelling of the affected epididymis or testicle; scrotal ultrasound is useful diagnostically, especially to rule out associated abscess. When infection is advanced, the entire ipsilateral scrotal contents become involved, with overlying skin fixation and edema. It may be difficult to distinguish this entity from late torsion, incarcerated inguinal hernia, or testicular tumor with necrosis and inflammation. Patients without abscess may be managed with antibiotic therapy, rest, and scrotal elevation; however, recovery is slow, with eventual resolution of edema and discomfort. If abscess is present, surgical drainage and often orchiectomy are indicated. A subset of patients may have persistent pain or mass, and on repeated Doppler imaging, signs of testicular ischemia or persistent inflammation may be noted. These patients require exploration and possible orchiectomy to resolve the process.
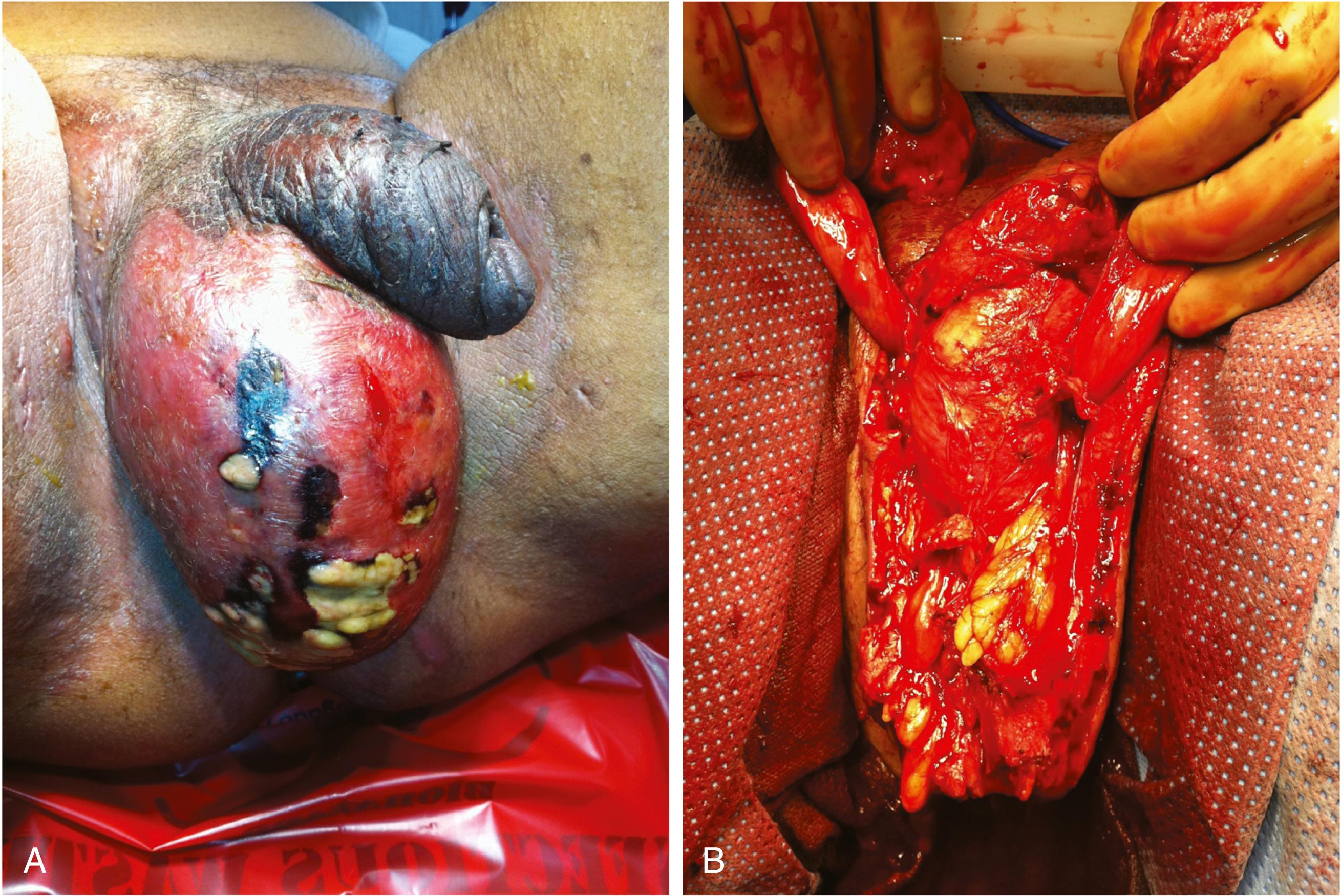
Fournier gangrene is a necrotizing infection of the male genital and perineal skin and subcutaneous tissues, similar to other progressive fasciitis and necrotizing soft tissue infections ( Fig. 74.2 ). When the genitalia are involved, patients typically present with significant pain and tenderness, scrotal and genital swelling, discoloration or frank necrosis, crepitus, and, at times, foul-smelling discharge. Fournier gangrene is usually a polymicrobial infection with microaerobes, anaerobes, and gram-positive and gram-negative organisms. Risk factors for development include peripheral vascular disease, diabetes mellitus, malnutrition, alcoholism, and other immunocompromised states. This disease represents a urologic emergency. Treatment requires urgent surgical drainage with aggressive debridement of the necrotic tissue, broad-spectrum intravenous antibiotics, and intensive monitoring with supportive care. The magnitude of the debridement depends entirely on the degree of progression of the process. It is rare for the process to involve the testicles or deep tissues of the penis deep to the tunica vaginalis and Buck fascia, respectively, so these structures should be preserved. It is uncommon for the urethra to be involved, although a defined urinary tract source may be evident, such as a urethral stricture, with perforation and local infection. Suprapubic tube diversion is generally not necessary initially; urethral catheter drainage is generally sufficient. Once the active infection is controlled, the predominant management issues become wound care and reconstruction, which may require delayed skin grafting for tissue coverage.
Fungal infections in the urinary system are most common in specific populations of patients: diabetics, immunocompromised patients, and the elderly. Fungal infections may not be symptomatic and, in an outpatient setting, may not require therapy. Most fungal infections are related to the Candida species, and it is incumbent on the treating physician to determine which infections require treatment and which represent contamination. Patients who require careful evaluation and treatment include neutropenic patients and intensive care patients, who may need evaluation for an internal source such as a fungus deposit (ball) in the bladder or kidney. Infectious disease consultation is valuable in these cases because the organisms are atypical and selection of treatment agents may not be straightforward. Renal and bladder imaging with ultrasound may demonstrate a treatable source. These patients may need antifungal bladder or kidney irrigation or occasionally endoscopic removal.
The genitourinary tract is the third most common extrapulmonary site for tuberculosis infection. This disease is spread hematogenously from the lungs and into the affected organ system. Most patients with genitourinary tuberculosis are immunocompromised, so assessment of HIV infection status is important. Patients present with various symptoms that include voiding symptoms, sterile pyuria or hematuria, and chronic kidney disease. Not all patients will have a positive purified protein derivative (PPD) test result, and diagnosis is confirmed with acid-fast bacilli smears of urine and mycobacterial culture with sterile pyuria, chest radiograph, and imaging of the genitourinary system to look for anatomic abnormalities. Tuberculosis affecting the kidney may result in segmental or global glomerular dysfunction, and progression antegrade down the urinary system may result in ureteral strictures. Tuberculosis of the epididymis may result in chronic epididymitis or mass. Antibiotic therapy consists of two months of a four-drug regimen with a subsequent seven month treatment with isoniazid and rifampin. Infectious disease consultation is mandatory in treating these patients because of public health concerns. Significant anatomic infection or functional change or loss may ultimately require surgical excision.
With the ease of global transportation and a mobile global population, parasitic infections are considerations in patients with recent travel histories. The main parasitic infections of the genitourinary system are schistosomiasis, echinococcal infection, and filariasis. Each parasite has a different point of entry, systemic spread, and organ infestation. Typically, in schistosomiasis, the parasite enters the body percutaneously and spreads through the venous and lymphatic system. Most infestations affect the bladder, resulting in chronic inflammation and granulomas. These patients present with LUTS or hematuria. Medical therapy (praziquantel) can be used to treat granulomatous disease; however, untreated infections can result in squamous cell carcinoma of the bladder. Echinococcal infections are spread through ingestion of contaminated food, and the parasite penetrates the intestinal walls and infests the liver. On occasion, renal infestation can occur, with the parasite becoming encysted in the parenchyma. Medical therapy can shrink the cysts, but surgical removal by partial or total nephrectomy is required for cure. These cysts must be removed intact as rupture or spillage of internal contents can result in severe anaphylaxis. Filariasis results from direct infection of the lymphatic system through percutaneous entry. The parasite creates noticeable symptoms when it dies, resulting in obstruction of the lymphatics. Only mild infestation can be treated with oral therapy (albendazole); advanced disease requires excision and reconstruction.
A central aspect of urology is management of bladder function and evaluation and treatment of bladder dysfunction. The bladder is a large muscular sac responsible for storing and eliminating urine. Common dysfunctions of the bladder include neurogenic problems with bladder function, storage problems, incontinence, and outflow issues related to benign prostatic hyperplasia (BPH) or enlargement. Changes in these functional areas are one of the most common reasons for urologic consultation. Although this is a broad area of urology, concentrating on these core divisions will give the general surgeon an understanding of the complex dynamics of bladder function and dysfunction.
Patients with neurogenic bladder dysfunction present with a wide spectrum of neurologic diseases or injuries that affect bladder function on the basis of the location of the injury or disease process. There is a complex interaction between the bladder and brain that primarily regulates bladder storage and bladder emptying. Bladder storage is driven by the sympathetic nervous system, specifically at the level of the adrenergic receptor. α-Adrenergic receptors are the most common adrenergic receptors in the bladder, prostate, and urethra; most are α 1 and α 2 , with three subtypes of α 1 identified: α 1a , α 1b , and α 1d . The α 1 receptor is the most common subtype in the lower urinary system. Bladder emptying is driven by the parasympathetic stimulation of cholinergic receptors, specifically the muscarinic receptors. The predominant muscarinic receptors in the bladder are M 2 and M 3 . Sensory information is carried away from the bladder by myelinated and unmyelinated afferent nerve fibers traveling through the pelvic and pudendal nerves. Any interruption in the sympathetic or parasympathetic nervous system and its communication with the bladder can result in neurogenic dysfunction. In addition, several centers within the pons, midbrain, and cerebral cortex have direct effect on the storage and emptying of the bladder. Voiding is initiated at the level of the pontine micturition center, which sends out a parasympathetic signal to the bladder to initiate voiding. The pontine micturition center is inhibited by the periaqueductal gray located in the midbrain, and this is connected to the afferent signaling pathways from the bladder. Based on this standard sensory function, specific voiding symptoms or LUTS can be predicted by the location of neurologic disease or injury.
Basic evaluation of these patients includes a through history with neurologic and urologic historical focus, physical examination (focusing on the abdomen, pelvis, and peripheral and central nervous system), and urinalysis. Additional evaluation is tailored to location of injury. Cortical brain disease and injury, such as cerebrovascular accident, are evaluated by history, physical examination, and urinalysis. These disease processes do not directly affect the bladder function, and patients are treated on the basis of symptoms alone. Spinal cord lesions are divided into suprasacral spinal lesions (spinal cord injury, infarcts) and sacral or peripheral spinal cord lesions (pelvic plexus damage from surgery, diabetic neuropathy). Patients with lesions of the suprasacral spinal cord tend to have increased bladder muscle tension, which results in abnormal elasticity of the bladder (poor bladder compliance). In addition, these patients have incoordination of the bladder and urinary sphincter, resulting in detrusor-sphincter dyssynergia. Patients with sacral or peripheral nerve lesions tend to have variable LUTS but typically do not have changes in bladder elasticity. The detrusor muscle is often partially or completely nonfunctional, and the urinary sphincter remains closed. Specialized evaluation of the patients with spinal cord lesions includes upper tract ultrasonography to monitor for evidence of hydronephrosis and urodynamic evaluation. Urodynamic evaluation involves measuring the elasticity of the bladder on filling (compliance), the pressure generated on emptying (detrusor function) by recording the abdominal pressure, and the intraluminal bladder pressure with specialized catheters. Surveillance cystoscopy is indicated in chronic patients to rule out the development of intravesical disease. Treatment for neurogenic bladder has recently been revolutionized by the introduction of onabotulinum toxin. In the past, these patients required complex regimens of antimuscarinic agents and reconstructive surgery. Now, with the use of onabotulinum toxin, most patients are treated with periodic cystoscopic injections and intermittent catheterization.
Overactive bladder (OAB) is the most common storage-related problem of the bladder. It is defined as urinary urgency with or without urgency urinary incontinence in the absence of UTI or other obvious disease. Typical symptoms of this problem include urgency, urinary frequency, nocturia, and urgency urinary incontinence. Urgency refers to the sudden, compelling desire to pass urine that is difficult to defer and replaces the normal urge. Urinary frequency is the complaint of micturition occurring more frequently than previously deemed normal and characterized by daytime and nocturnal voids. Nocturia is the complaint of interruption of sleep one or more times because of the need to urinate. Finally, urgency urinary incontinence is the involuntary loss of urine associated with urgency. A difficult aspect of this disease process is that it occurs in the spectrum of other LUTS and may be the result of long-term bladder outflow obstruction. Other conditions to consider in patients who present with OAB and LUTS are UTI, urinary calculi, diabetes, polydipsia, neurogenic bladder, and malignant disease. OAB has a worldwide prevalence of 11%, and with the aging population, this is presumed to increase over time.
All patients who present with OAB should undergo a thorough evaluation. At the basic level, this includes a thorough history to fully disclose the symptoms and to rule out other causes. Historical elements that may be contributory include caffeine intake, constipation, recurrent UTI, pelvic organ prolapse in women and prostatic enlargement in men, and excessive fluid intake. Physical examination should be directed toward evaluation of the abdomen, pelvis, and neurologic systems. Other findings may include decreased mental status or cognitive function and peripheral edema. The last absolute examination element is urinalysis, which can reveal infection, inflammation, or hematuria that may indicate more serious disease. Simple adjunctive tests that can be performed in the office include measurement of postvoid residual urine volume, noninvasive flow test, validated symptom questionnaires, and voiding diaries. Specialized tests and evaluation performed by the urologist may include cystoscopy, ultrasound, and urodynamic testing as appropriate. However, current guidelines do not require any of these specialized tests for initiation of treatment.
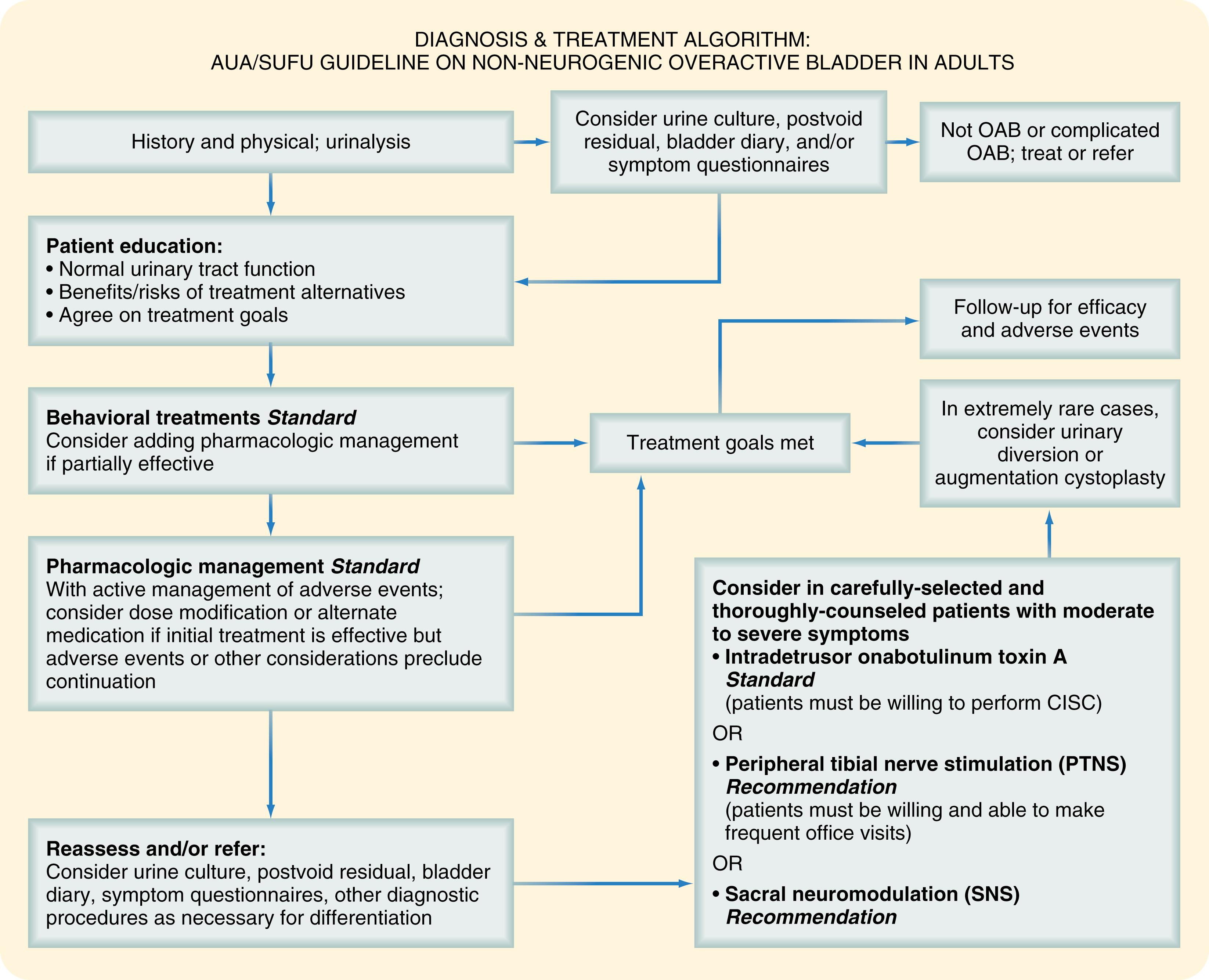
Treatment of OAB is directed toward therapy, symptoms, and motivation of the individual patient ( Fig. 74.3 ). As many patients suffering from this problem take multiple medications, pharmacologic therapy is not always offered as an initial treatment. Behavioral therapies are the first-line treatment for all patients. Behavioral therapies may include lifestyle modifications or specific physical therapies. Typically, this includes fluid intake management and modification with particular attention paid to timing of fluid intake and amounts. For example, in patients who complain of nocturia, limiting nighttime fluid intake can be beneficial. Bladder training is a noninvasive method of physical therapy whereby the patient postpones voiding to lengthen the time intervals between voids. This may be coupled with urgency suppression and timed voids to reinforce retraining of the sensory output from the bladder. Finally, voiding diaries are important to help the patient and urologist quantify the number of voids and voided amount to better target improvement goals and to tailor therapy. Pharmacologic management continues to be a mainstay of treatment and is indicated for patients as an adjunct to behavior therapies or for patients unresponsive to first-line therapy. Classic pharmacologic therapy is antimuscarinic agents that target the parasympathetic muscarinic cholinergic receptors, primarily M 2 and M 3 , and block the action of these receptors. Most of the drugs in this category are administered daily and have the common side effects of dry mouth, dry eyes, and constipation. A newer pharmacologic agent, beta agonists (β 3 ), targets receptors in the detrusor muscle to stimulate bladder relaxation. Treatment options for patients who fail to respond to these therapies fall into the specialized third-line treatments, which include neuromodulation (either peripheral or central), onabotulinum toxin, chronic indwelling catheters, and augmentation cystoplasty.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here