Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A variety of uncommon or rare tumors develop in the lung, with incidence rates of 1 in 100,000 people or fewer. For this group of neoplasms, most published accounts take the form of case reports and small series. Given the unusual nature of these processes, it is likely that some examples will be classified as other, more common, types of neoplasms due to lack of familiarity with the entity or with its potential to develop in the lungs. This chapter will provide an overview of these tumors, recognizing that more information will undoubtedly become available with the growing availability of genetic and genomic data, which assist in tumor classification and prognostic assessment.
These entities represent a rare and distinctive group of neoplasms arising from the seromucinous glands of the trachea and bronchi. The majority of these tumors are of low malignancy, are centrally located, and share similar histologic features with their counterparts arising in the major salivary glands. The most common members of this category to occur as primary neoplasms of the lung are discussed in this chapter. Other histologic types of salivary glandlike tumors can also arise in the lung; case reports and small series of epithelial-myoepithelial carcinomas, acinic cell carcinomas, salivary duct carcinomas, hyalinizing clear cell carcinomas, myoepithelial carcinomas, and other related lesions can be found in the literature.
Mucoepidermoid carcinoma is a malignant neoplasm composed of squamoid cells, mucin-producing cells, and cells of intermediate type
Less than 1% of lung neoplasms
Bronchial obstruction by the tumor can lead to pneumonia, bronchiectasis, and atelectasis
Low-grade tumors are associated with low mortality
For high-grade tumors, survival is similar to non-small cell lung carcinomas
Occur at any age from childhood to late adulthood
Symptoms include cough, hemoptysis, shortness of breath, fever, and pneumonia
Centrally located solitary nodule
Postobstructive pneumonia or atelectasis distal to the tumor
Sleeve resection or laser therapy is used for low-grade tumors and is usually curative
Surgical resection and postoperative radiotherapy is used for high-grade tumors
Low-grade tumors rarely metastasize to the lymph nodes
High-grade tumors may metastasize to bone, liver, adrenals, and brain
Polypoid endobronchial mass usually originating in a lobar or segmental bronchus
Cystic and/or solid appearance with mucus
Infiltrative margins with necrosis and hemorrhage in high-grade tumors
Postobstructive pneumonia, bronchiectasis, and atelectasis may be seen
Mucus-filled cysts and solid areas
The columnar cells lining the cysts show round, basally located nuclei with mild atypia and apical mucin-rich cytoplasm
Solid areas are composed of squamoid and intermediate cells
The stroma may be dense or hyalinized with calcification
A solid squamoid and/or intermediate component usually predominates, with less evidence of cyst or gland formation
Marked nuclear atypia and pleomorphism and high mitotic activity are typical
Necrosis and hemorrhage can be present
Tumor cells are positive for pancytokeratins and CK7
Intermediate cells are positive for CK 34βE12, p63, and p40 (variable)
Squamoid cells express CK5/6.
CK20, TTF-1, and napsin A are negative
Fusion gene CRTC1-MAML2 in low- and high-grade carcinomas
Mucous gland adenoma
Adenosquamous carcinoma, squamous cell carcinoma, adenocarcinoma
Metastatic mucoepidermoid carcinoma from the head and neck
Mucoepidermoid carcinoma is an uncommon neoplasm representing less than 1% of lung tumors. These tumors may be observed in any age group, including children, in whom they are one of the more common bronchial tumors. Because most of these tumors occur endobronchially, symptoms are due to bronchial obstruction and include cough, hemoptysis, shortness of breath, fever, and pneumonia, but some patients are asymptomatic. There is no association with smoking.
Radiologically, mucoepidermoid carcinoma presents as a centrally located, solitary nodule, which is typically positive on a positron emission tomography (PET) scan. Parenchymal consolidation may be seen distal to the tumor.
Mucoepidermoid carcinomas form endobronchial masses covered by bronchial mucosa that can have a smooth surface or can be focally ulcerated. They generally arise in the proximal bronchi or the trachea. The cut surface of the tumor has a cystic or solid appearance with abundant mucin. High-grade tumors are usually larger, have necrotic and hemorrhagic areas, and tend to infiltrate the lung parenchyma. The pulmonary parenchyma distal to the tumor may show secondary bronchiectasis and postobstructive pneumonia.
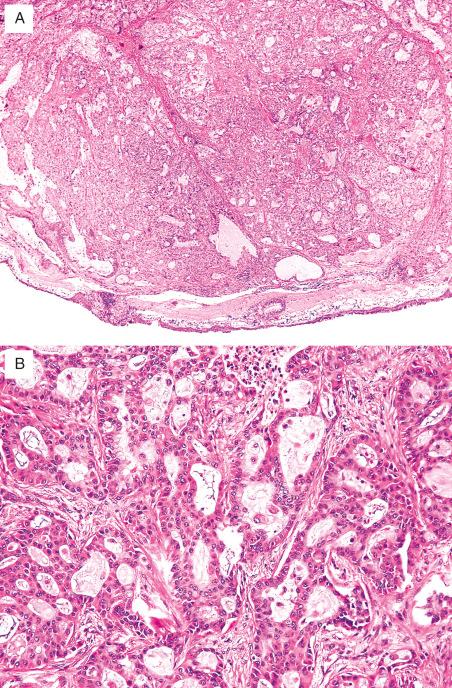
Mucoepidermoid carcinomas are divided into low and high grades based on morphologic and cytologic features. Low-grade mucoepidermoid carcinomas show solid and cystic areas filled with mucus ( Fig. 28.1 ). The cysts are lined by columnar cells with small, basally located nuclei with little cytologic atypia and abundant mucin-rich cytoplasm. Mitoses are rare. The lumina are typically filled with mucin, and occasionally mucin spills into the surrounding stroma, stimulating a granulomatous reaction, calcification, and ossification. The solid areas are composed of squamoid and intermediate cells. Squamoid cells have dense cytoplasm and well-defined cell borders. The intermediate cells are smaller than the squamoid cells, round or oval, with eosinophilic cytoplasm and sometimes with perinuclear clearing. The stroma may be myxoid or fibrotic, sometimes with dense hyalinized material and calcification. A prominent lymphoplasmacytic infiltrate may be associated with the tumor. High-grade mucoepidermoid carcinomas show a predominance of solid areas composed of intermingled squamoid and intermediate cells. In addition, they are characterized by increased nuclear pleomorphism, high mitotic counts, and areas of necrosis and hemorrhage.
These tumors stain with pancytokeratins and CK7 and are negative for CK20, thyroid transcription factor 1 (TTF-1), and napsin A. The intermediate cells are positive for cytokeratin 34βE12 and p63, and p40 is variably expressed. Cytokeratin 5/6 is positive in the squamoid component.
The fusion gene CRTC1-MAML2 is found in many low- and high-grade mucoepidermoid carcinomas and represents a diagnostic marker. It can be evaluated using a fluorescence hybridization in situ (FISH) break-apart probe. EGFR mutation has also been described in some cases.
Low-grade mucoepidermoid carcinomas differ from mucous gland adenomas by the presence of intermediate cells and squamous differentiation in the former. High-grade mucoepidermoid carcinomas must be differentiated from adenosquamous carcinomas. Features favoring high-grade mucoepidermoid carcinoma include an endobronchial growth pattern, lack of squamous cell carcinoma in situ in the surface epithelium, lack of individual cell keratinization and keratin pearl formation, and areas of low-grade mucoepidermoid carcinoma. TTF-1 and MAML2 rearrangement are also helpful for differentiating mucoepidermoid carcinoma (TTF1-negative, MAML2 rearrangement often present) from adenosquamous or adenocarcinoma of the lung (TTF-1 often positive, MAML2 rearrangement-negative). Metastasis from a mucoepidermoid carcinoma arising in the head and neck should also be excluded before classifying a mucoepidermoid carcinoma as a primary pulmonary neoplasm.
The treatment and prognosis of these tumors are related to the histologic grade. Low-grade tumors appear to have an excellent prognosis, particularly in children, and very rarely metastasize to the lymph nodes. Tumors may be treated by sleeve resection or laser therapy, but lobectomy or pneumonectomy may be required. High-grade tumors are treated with surgical resection and may receive postoperative radiotherapy. They behave more aggressively; prognosis is related to the clinical staging at the time of the diagnosis.
Malignant epithelial and myoepithelial cell tumor similar to its counterpart arising in the salivary glands, with characteristic cribriform and tubular arrangements of tumor cells
Less than 1% of malignant tumors of the lung
With advanced disease, death is often due to widespread metastases
Postobstructive pneumonia is a frequent complication
Most frequently diagnosed in the fifth decade
Symptoms are usually related to bronchial obstruction (cough, hemoptysis, wheezing)
Solitary, centrally located mass, often with an endobronchial component or a diffuse wall thickening
Prognosis depends on the clinical stage at presentation
Well-demarcated endobronchial neoplasms have a long survival, up to 15 years
Recurrences are common, and late metastasis occurs
Surgical resection is the treatment of choice
Well-circumscribed, endobronchial, polypoid masses in large airways
Less often, annular lesions with thickening of the airway walls
Uniform epithelial cells with round nuclei and pale eosinophilic cytoplasm arranged in three main patterns: cribriform, tubular, solid
In the cribriform and tubular patterns, the cells form nests, columns, or tubules around cystic spaces containing mucinous basophilic or eosinophilic PAS–positive basal lamina material
In the solid pattern, the cells form islands without cystic spaces
Low mitotic rate
Perineural invasion and infiltration of the bronchial wall are common
Luminal cells express cytokeratins, CEA, and EMA
Cells around pseudocysts stain with vimentin, S-100, actin, p63, and calponin
Extracellular material is immunoreactive for type IV collagen, laminin, heparin sulfonate proteoglycan, and entactin
Overexpression of C-kit (CD117)
Reports of loss of heterozygosity of chromosomes 3p14 and 9p and losses at 3p, 4p, and 15q and gains at 12q15 ( MDM2 site)
Adenocarcinomas of the lung
Basaloid carcinoma
Small cell carcinoma
Metastatic ACC
Adenoid cystic carcinoma (ACC) represents less than 1% of all lung tumors. They are most often diagnosed in the fifth decade of life, and there is no apparent gender predilection. The symptomatology is related to bronchial obstruction and its sequelae and consists of cough, hemoptysis, wheezing, and shortness of breath.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here