Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Ultrasound is a key method of guidance for biopsy and fluid drainage because of its real-time needle visualization and the ability to image and intervene in multiple anatomic locations and planes.
Effective periprocedural antithrombotic management requires an understanding of specific antithrombotic agents as well as the balance of the potential risk of hemorrhage from a given procedure versus the risk of a thrombotic event if a blood thinner is discontinued.
Ultrasound typically offers excellent guidance for superficial biopsies, paracentesis, thoracentesis, and most solid organ biopsies in the abdomen including liver, kidney, and spleen. CT guidance is often utilized for adrenal, retroperitoneal, and certain deep pelvic biopsies or deep drain placement.
Familiarity with both trocar and Seldinger techniques is useful for ultrasound-guided drain placement.
Percutaneous biopsy and fluid drainage are invaluable diagnostic and therapeutic procedures for the management of patients. Ultrasound is a central method of guidance for these interventional techniques because it allows real-time needle visualization and the ability to image and intervene in multiple anatomic locations and planes. An approach to this topic requires knowledge of the current fundamental methods and applications of these procedures in general and in terms of specific anatomic locations.
Because of its relatively low cost and wide availability, ultrasound-guided biopsy has become one of the most important methods of tissue diagnosis in radiology practices worldwide. Ultrasound-guided biopsy is a safe and accurate technique for confirmation of suspected malignant masses and characterization of benign lesions in locations throughout the body. In addition, minimally invasive tissue confirmation decreases patient costs by obviating the need for a surgical diagnosis and decreasing duration of hospital stay and number of ancillary diagnostic tests. In addition, lack of ionizing radiation and real-time imaging during the procedure make the procedure safer.
In most cases a biopsy is performed in the setting of possible malignancy, for either initial diagnosis of cancer, confirmation of metastatic disease, or to obtain tissue for molecular profiling and targeted treatment planning. In other patients, biopsy is performed to gauge the presence of parenchymal disease in a native organ or rejection in a transplanted organ. Occasionally, biopsy is indicated simply to determine the nature of an incidentally discovered mass.
Relative contraindications to percutaneous needle biopsy include severe uncorrectable coagulopathy, lack of a safe biopsy route, and an uncooperative patient. To assess for inherent coagulopathy, the most valuable information comes from the patient history, including bleeding tendency or need for transfusion or a family history of bleeding diathesis. Patient medications should also be reviewed for recent use of antithrombotic agents.
The second relative contraindication is the lack of a safe biopsy route. A biopsy path extending through large vessels such as the splenic or extrahepatic portal vein increases the risk of hemorrhage. A biopsy path free of overlying stomach or bowel is also a preferable route, although such biopsies have been safely performed using smaller (21-gauge) needles. Biopsies performed through ascites have also proved to be safe, although drainage of ascites prior to biopsy may increase target accessibility.
The third relative contraindication to needle biopsy is an uncooperative patient in whom uncontrolled motion during needle placement increases the risk of unanticipated injury and hemorrhage. This is a particularly common problem in pediatric patients, and deeper sedation may be required.
An effective approach to the management of periprocedural antithrombotics depends on an understanding of the balance of hemorrhagic and thrombotic complications. That is, the potential risk of hemorrhage from biopsy or drainage in a patient on an antithrombotic agent versus the risk in that same patient of a thrombotic event if a blood thinner is discontinued. Significant thromboembolic events, including myocardial infarction and ischemic stroke, have been shown to occur in 1% to 4% of select patients in whom aspirin or warfarin is withheld without bridging therapy. Although decisions on periprocedural antithrombotic management are best made in collaboration with the referring clinician, the performing radiologist typically makes the ultimate judgment of whether and when to perform a procedure for a patient on an antithrombotic agent. It is therefore important for the radiologist to have a general knowledge of common anticoagulants and antiplatelet agents as well as the bleeding risks associated with certain procedures. However, any withdrawal of a therapeutic agent should be deferred to the ordering clinical provider, often following a discussion with the radiologist regarding procedure-specific bleeding risk.
Although helpful institutional and society guidelines have been put forth on the topic of periprocedural antithrombotic management, true consensus and uniformity in practice remain elusive. This is due to the expanding pharmacy of antiplatelet agents and anticoagulation as well as to evolving literature showing lower bleeding risks for some procedures than previously thought. In general, our own practice has leaned toward liberalizing guidelines; that is, foregoing preprocedural labs in certain patients for lower-risk procedures (superficial biopsies such as thyroid and superficial lymph nodes as well as thoracentesis, paracentesis, and superficial abscess drainage) and performing certain lower-risk procedures, especially if urgent, without discontinuing antithrombotic agents.
The most commonly encountered antithrombotics in both inpatient and outpatient populations are the antiplatelet agents aspirin and clopidogrel (Plavix), the vitamin K antagonist warfarin, and the clotting factor inhibitor heparin (unfractionated or low-molecular-weight). Anticoagulants using other mechanisms such as direct thrombin inhibitors (e.g., dabigatran), direct factor Xa inhibitors (e.g., fondaparinux), and glycoprotein IIb/IIIa inhibitors (e.g., abciximab) are being increasingly utilized and may also be encountered in practice. General familiarity with mechanisms and metabolism of these agents is important for decision making. For example, the direct thrombin inhibitor dabigatran has a half-life of 12 to 14 hours but is excreted by the kidneys; therefore the period of preprocedural discontinuation, if pursued for a nonurgent deep biopsy, should be extended in a patient with renal impairment (6-7 days vs. 4-5 days if normal renal function in our practice).
For low-risk procedures, such as thoracentesis and paracentesis, we have found little impact on bleeding risk from therapeutic anticoagulation or aspirin use. Bleeding complication rates in coagulopathic and thrombocytopenic patients (international normalized ratio [INR] > 1.6 and/or platelets < 50 × 10 9 /L) after thoracentesis or paracentesis are very low (up to 1%). Patients often benefit greatly from these procedures. Accordingly, we have eliminated routine complete blood count prior to these procedures for most patients and request warfarin be held only if patient is at low risk for thromboembolic event. If patients will be taking warfarin at the time of the procedure, an INR should be obtained within 24 hours prior to procedure to ensure they are not supratherapeutic. Additional labs may be requested by the radiologist at their discretion, but we have found this is rarely needed. Aspirin may also be continued in our practice for thoracentesis or paracentesis. A similar approach is used for superficial biopsies and superficial drain placement.
Higher-risk procedures include liver and kidney biopsy as well as mesenteric, retroperitoneal, or deep pelvic lymph node biopsy, and deep abscess drainage. Although called “higher risk” this is relative to other procedures, and the true risk of postprocedural bleeding, even for these procedures, is low.
Native renal parenchymal biopsies have the highest risk of postbiopsy bleeding with reported rates of significant bleeding of 0.3% to 6.6%. Liver and renal transplant biopsy bleeding rates are generally lower and at our own institution are 0.5% and 0.2%, respectively. If a higher-risk biopsy is nonurgent or elective, aspirin can be held for 5 days beforehand if the risk of thromboembolic event is acceptably low and then restarted at 24 hours after biopsy. However, our clinical experience has shown little if any association of recent aspirin use on significant postprocedural bleeding. In a study of 15,181 percutaneous core biopsies, the incidence of bleeding in patients taking aspirin within 10 days before biopsy was 0.6% and that of patients not taking aspirin was 0.4% ( p = .34). This study included 585 liver biopsies performed in patients with recent aspirin use with a 0.3% risk of major hemorrhage (not significantly different to the 0.5% in those not taking aspirin). Consequently, we continue to perform many solid organ biopsies in patients on aspirin and rarely postpone or cancel a biopsy because of aspirin usage. Exceptions to this practice include elective biopsies, especially in a local patient who will be able to easily reschedule the procedure, and in some cases native kidney biopsies that already confer an increased risk of bleeding. The incidence of major hemorrhage after native or transplant renal biopsy in patients taking aspirin was slightly higher when compared to those not taking aspirin (1.0% vs. 0.6%) although this difference was not statistically significant ( p = .08). For warfarin and heparin, we recommend holding prior to a higher-risk biopsy if possible—5 days for warfarin (to INR ≤ 1.5), 4 hours for therapeutic dose intravenous (IV) unfractionated heparin, 24 hours for therapeutic dose low-molecular-weight heparin, and 12 to 24 hours for prophylactic dose unfractionated or low-molecular-weight heparin.
If the history suggests a bleeding disorder but the patient is not on an antithrombotic agent, prothrombin time (PT), activated partial thromboplastin time (aPTT), and platelet count should be obtained if a higher-risk procedure is planned. The role of bleeding time measurement is of uncertain value in determining bleeding risk; in most cases, no good evidence supports the value of the bleeding time to predict bleeding. For core biopsies or drains, platelets greater than 50 × 10 9 /L and an INR of 1.6 or less are the suggested thresholds but biopsy may be pursued even if patients fall outside these parameters at the discretion of the performing radiologist and the referring clinician after weighing the risks and benefits. Data have shown that a platelet count of 50 × 10 9 /L or less is a statistically significant risk factor for major bleeding after liver biopsy (2.2% vs. 0.5% rate of significant bleeding, p = .04). Interestingly, in the same study group, no patients with an INR of 1.6 or greater ( n = 43, range 1.6-1.9) had a significant postbiopsy hemorrhage.
Some coagulopathies can be corrected with the transfusion of appropriate blood products although there is unpredictable impact of this on postprocedural bleeding rates for certain procedures such as thoracentesis. For higher-risk biopsies, however, we continue to believe that there is benefit to transfusing to reach previously mentioned thresholds of platelets greater than 50 × 10 9 /L and INR of 1.6 or less in thrombocytopenic and coagulopathic patients if possible. Desmopressin (DDAVP) can be given to a uremic patient to improve functioning platelet activity. Postbiopsy embolization of the needle track has been reported to control hemorrhage in patients at high risk for bleeding and in whom the need for biopsy outweighs any risk, but it is not routinely performed in our practice.
Both ultrasound and computed tomography (CT) can be used to guide percutaneous needle intervention. The choice of method depends on multiple factors, including lesion size and location, relative lesion conspicuity on the two modalities, equipment availability, and personal preference.
Ultrasound has several strengths as a means of guiding percutaneous intervention. It is readily available, relatively inexpensive, and portable. Ultrasound uses no ionizing radiation and can provide guidance in almost any anatomic plane. The greatest advantage, however, is that sonography allows the real-time visualization of the needle tip as it passes through tissue into the target. This allows precise and confident needle placement and avoidance of important intervening structures. In addition, color Doppler flow imaging (CDFI) may help prevent complications of needle placement by identifying the vascular nature of a mass and by allowing the clinician to avoid vascular structures lying within the needle path.
Ultrasound guidance can be used for the biopsy of many organs and regions of the body. The technique is optimal for lesions located superficially or at moderate depth in a thin to average-sized person such as the omentum (Video 17.1 ), as well as for lesions within organs prone to respiratory motion (e.g., liver, kidney) (Video 17.2 ). In the latter scenario, the advantage of real-time ultrasound-guidance allows continuous visualization of the target during the biopsy. Lesions located within or behind bone or gas-filled bowel cannot be visualized because of near-complete reflection of sound from the bone or air interface.
Theoretically, any mass that is well visualized with ultrasound is amenable to ultrasound-guided needle biopsy. In our practice, most liver and kidney biopsies are performed with ultrasound guidance, as are biopsies of the thyroid and parathyroid glands. Superficial lymph nodes are also particularly well suited to real-time ultrasound-guided biopsy. Occasionally, the pancreas (particularly pancreas transplants) and other sites in the abdomen and pelvis undergo biopsy with ultrasound guidance if lesion visualization is adequate.
Compared with CT, ultrasound-guided procedures require less time to perform and can be more cost-effective. Ultrasound-guided biopsy has been shown to be more accurate than CT, with a lower false-negative rate.
CT is well established as an accurate guidance method for percutaneous biopsy of most regions in the body. It provides excellent spatial resolution of structures between the skin surface and targeted lesion, and it provides an accurate image of the needle tip. In addition, lesions located deep in the abdomen or within bone are better seen with CT than with ultrasound. In our practice, many pelvic, adrenal, pancreatic, retroperitoneal, and bone biopsies are performed with CT guidance because these structures are often best seen with this imaging method.
Historically, CT was limited by its lack of continuous visualization of the needle during insertion and biopsy. In the past decade, CT fluoroscopy has allowed real-time visualization of needle positioning. This has reduced the time required for interventional procedures at the cost of increased radiation dosage.
A variety of needles with a spectrum of calibers, lengths, and tip designs are commercially available for use in percutaneous biopsy. Needle caliber is based on outer diameter, with larger-caliber needles having a lower gauge number. Conceptually, needles can be grouped into small-caliber (20 gauge or smaller) or large-caliber (19 gauge or larger) sizes. Small-caliber needles are traditionally used to obtain cells for cytologic analysis by using a procedure commonly referred to as fine-needle aspiration (FNA). However, small pieces of tissue may be obtained for histologic examination as well. With these small-caliber needles, masses behind loops of bowel can be punctured with minimal likelihood of infection. The smaller samples yielded by small-caliber needles are appropriate to confirm tumor recurrence or metastasis in a patient known to have a previous primary malignancy. Even if the sample is small, the pathologist is usually able to make an accurate diagnosis by comparing the biopsy specimen with the original tissue.
Large-caliber needles can be used to obtain greater amounts of tissue for more thorough histologic and cytologic analysis. Larger needles may be necessary to obtain sufficient tissue to diagnose and subtype some types of malignancies (e.g., lymphoma), many benign lesions, and most chronic diffuse parenchymal diseases (e.g., hepatic cirrhosis, renal glomerulonephritis, renal allograft rejection). The large-caliber tissue sample can also be used to generate an additional “touch prep” specimen, whereby the tissue is manually swiped across a glass pathology slide, leaving a cellular sample on the slide for cytologic analysis.
The preference and level of expertise of the pathologist involved in the interpretation of biopsy specimens are considerations in the selection of needle size and type. Cytopathologists specialize in the interpretation of cellular samples, rendering a diagnosis based on the cells provided. Unfortunately, some clinical facilities do not offer cytopathologic interpretation. Histopathologists, in contrast, often prefer a large biopsy specimen for interpretation. For example, a large biopsy specimen from a metastatic lesion often allows a more reliable prediction of the primary site of the malignancy than a tiny sample or a cytologic aspirate. Determination of the primary site allows the oncologist to tailor subsequent treatment.
Before any invasive procedure is performed, the procedure, risks, alternatives, and benefits should be explained in terms that the patient can understand so that informed consent can be obtained. The performing physician must address patient apprehension about potential pain during the procedure and possible complications of the biopsy. After discussing the procedure, any patient questions should be answered fully.
Biopsies are frequently performed on an outpatient basis. Discomfort during the procedure is rarely severe and is usually controlled by appropriate administration of local anesthetic after the skin is cleaned and draped. An IV access may be established before the biopsy in the event that fluid or medications are necessary during the procedure. Premedication is usually not necessary. Sedatives and analgesics such as midazolam or fentanyl can be administered intravenously after consent has been obtained. In patients with an increased risk of bleeding, a larger or second IV access site may be prudent.
There are two options to sterilize the transducer. The transducer may be covered with a sterile plastic sheath, although this may degrade image quality and make the transducer more difficult to handle. Alternatively, the transducer itself may be directly sterilized and placed directly on the skin. Sterile gel is used as an acoustic coupling agent. After the biopsy, the transducer is soaked for 10 minutes in a bactericidal dialdehyde solution.
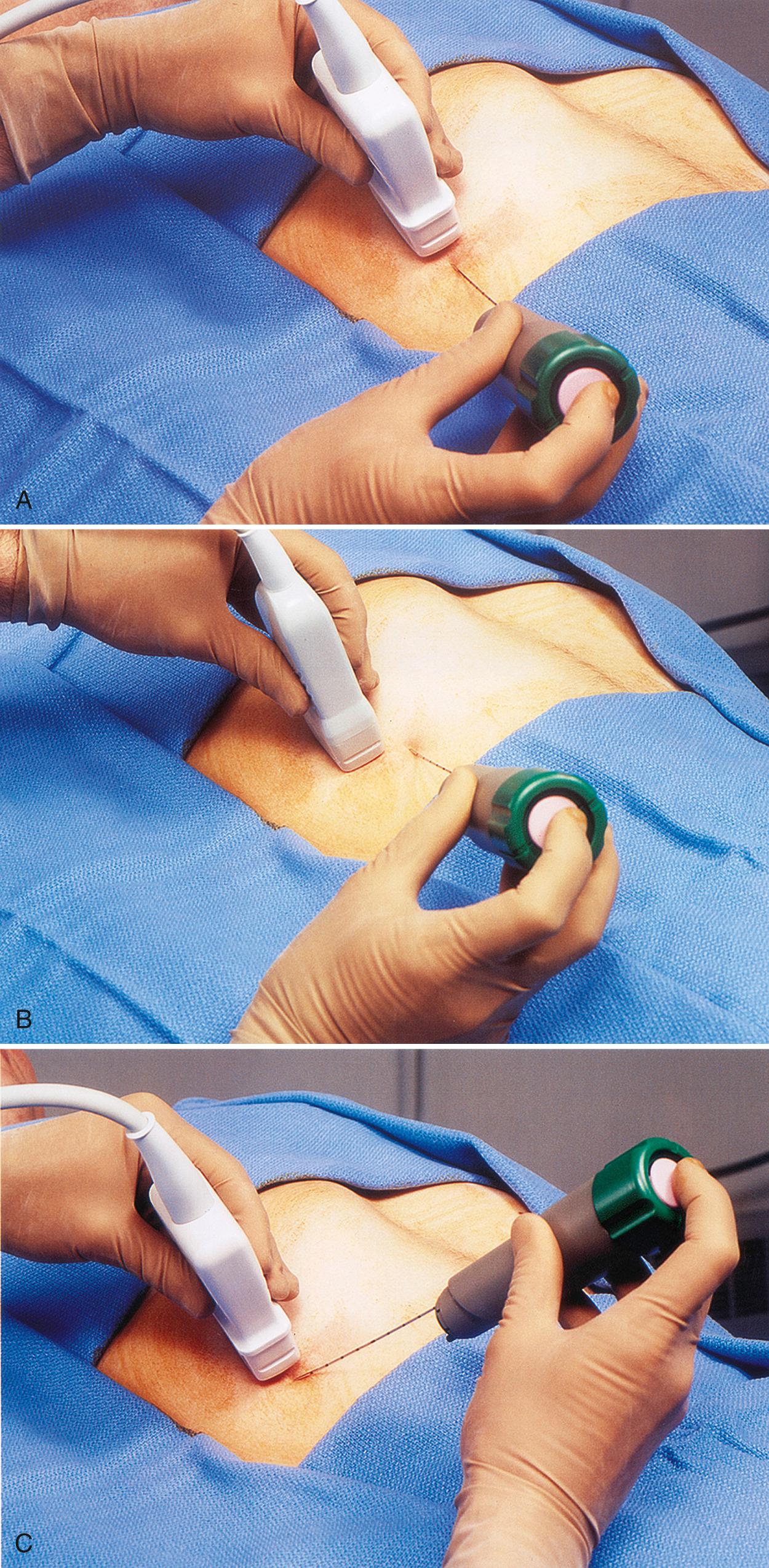
Most ultrasound-guided biopsies are performed under continuous real-time visualization. Needle guidance systems designed to facilitate proper needle placement are commercially available. These guides attach to the transducer and direct the needle to various depths from the transducer surface, depending on the preselected angle of the guide relative to the transducer ( Fig. 17.1A,B ). Many radiologists prefer the “freehand” technique in which the needle is inserted through the skin directly into the view of the transducer without the use of a guide ( Fig. 17.1C ). The needle is then independently directed to the target lesion by the operator under real-time ultrasound visualization ( and 17.4 ).
In contrasting these two biopsy techniques, one can appreciate the technical ease provided by the needle guidance method. This can decrease the time to perform a biopsy, particularly in the hands of a novice operator. However, the freehand technique allows greater flexibility to the operator in performing subtle adjustments to the needle path in the event of patient movement, particularly with respiration.
FNA biopsies are performed by placing the tip of the needle into the target lesion and rapidly “bobbing” the needle within the mass, collecting cellular samples within the lumen of the small needle. Some biopsy devices include a syringe on the end to provide negative pressure within the lumen, increasing the cellular yield.
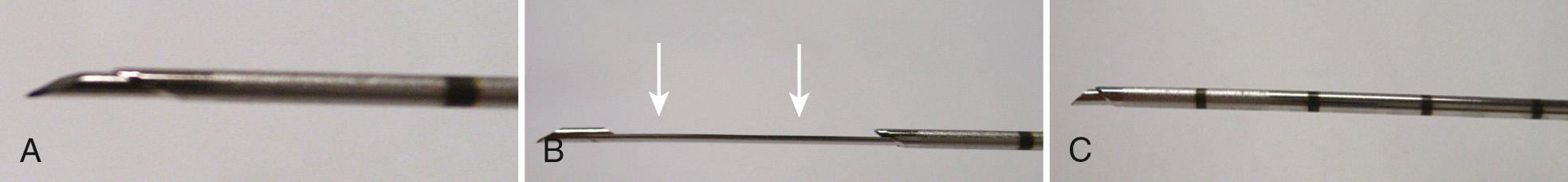
Large-caliber needles are used to obtain cores of tissue. With the typical spring-loaded core biopsy device (biopsy “gun”), the needle tip is advanced to the margin of the target lesion. Careful attention is made to the anticipated excursion of the device to prevent injury to deeper structures. Some biopsy devices allow initial manual advancement of the stylet through the target lesion to the desired depth. When the spring-loaded cutting sheath is activated, the sheath advances over the stylet, but there is no additional forward motion of the needle ( Fig. 17.2 ).
Most biopsies are performed by making one or more passes into a mass with a single needle. Occasionally, two needles are used in a coaxial manner, whereby a larger introducer needle is first placed into the mass. The inner stylet of this needle is then removed, and a longer, smaller-caliber needle is placed through its lumen. Multiple samples can then be obtained with the smaller needle without the need to reposition the larger introducer needle. This technique allows a large amount of tissue to be obtained with only one puncture of the organ capsule, although gas introduced during the procedure may interfere with ultrasound imaging. Although intuitively this should decrease bleeding complications, this has not been conclusively demonstrated in real practice. This may be related to the large caliber of the introducer needle or the extended time during which the introducer needle lies within the organ, potentially tearing the capsule.
After the biopsy is performed, the patient is typically observed in the radiology department for a period commensurate with procedure risk. Longer observation may be appropriate if there is clinical concern about a potential complication. In many medical centers, initial cytologic results are available within this time. If the results of the initial cytologic analysis are not conclusive, a repeat biopsy may be performed while the patient is in the department. When core biopsy tissue samples are obtained, frozen-section analysis may be performed for diagnosis if the touch-prep cytology specimen is inconclusive. In this case, additional samples may be necessary if permanent fixation or special staining is required.
Continuous real-time visualization of needle tip advancement is one of ultrasound's greatest strengths as a biopsy guidance method. Unfortunately, this is frequently the most technically difficult aspect of ultrasound-guided biopsy for many radiologists. Beginners may choose to practice on a homemade ultrasound biopsy phantom to develop the coordination necessary for ultrasound-guided procedures.
The most common reason for nonvisualization of the needle tip is improper alignment of the needle tip and transducer. To visualize the entire needle, the needle and central ultrasound beam of the transducer must be in the same plane. This allows the entire shaft of the needle to be visualized. Although malalignment rarely occurs with the use of a mechanical needle guide, such parallel placement can be challenging using the freehand technique, particularly when the radiologist is focused on the ultrasound image. In many cases the radiologist can simply look at the alignment of the needle with the transducer to allow gross correction of path deviation ( Fig. 17.3 ), and then fine-tune the needle alignment with ultrasound imaging.
A bobbing or in-and-out jiggling movement of the biopsy needle during insertion improves needle visualization. This bobbing motion causes deflection of the soft tissues adjacent to the needle and makes the trajectory of the needle much more discernible within the otherwise stationary field. Alternatively, if using a coaxial system, the inner, smaller needle can be “pumped” or moved in and out within the larger cannula.
Needle visualization can also be improved by increasing the reflectivity of the biopsy needle. Large-caliber needles are more readily visualized than small-caliber needles. Keeping the bevel of the needle directed toward the transducer may also increase the conspicuity of the needle tip. Some authors have found CDFI helpful to visualize needle motion, although we have not routinely incorporated Doppler ultrasound into our practice. Modifications in needle tip design to enhance needle visualization include scoring the needle tip and using a screw stylet. Extrareflective needles specifically designed for ultrasound guidance are commercially available. Most needles, however, are sufficiently visible sonographically as long as the needle and transducer are aligned.
The echogenicity of the parenchyma of the organ undergoing biopsy also affects the visibility of the biopsy needle. If the parenchyma is relatively hypoechoic, such as liver, kidney, or spleen, the echogenic needle can usually be identified easily. Conversely, if the organ or soft tissues are relatively hyperechoic, it is usually difficult to visualize the echogenic needle tip in this background. This is particularly relevant in the biopsy of masses in obese patients or masses surrounded by complex fat, as in the retroperitoneum.
Linear or curved array transducers are frequently used for guiding procedures because of their good near-field resolution, which allows visualization of the needle after relatively little tissue penetration. The focal zone of the ultrasound beam should also be placed in the near field for better needle visualization. Sector transducers are often used if there is a small acoustic window or if there is a deep lesion where a steep needle approach will be needed.
Clear visualization of the biopsy needle is an important element in the success of ultrasound-guided needle biopsies. The various techniques described here can be used to enhance needle visualization. However, considerable real-time scanning experience remains the key factor to the successful performance of ultrasound-guided biopsies.
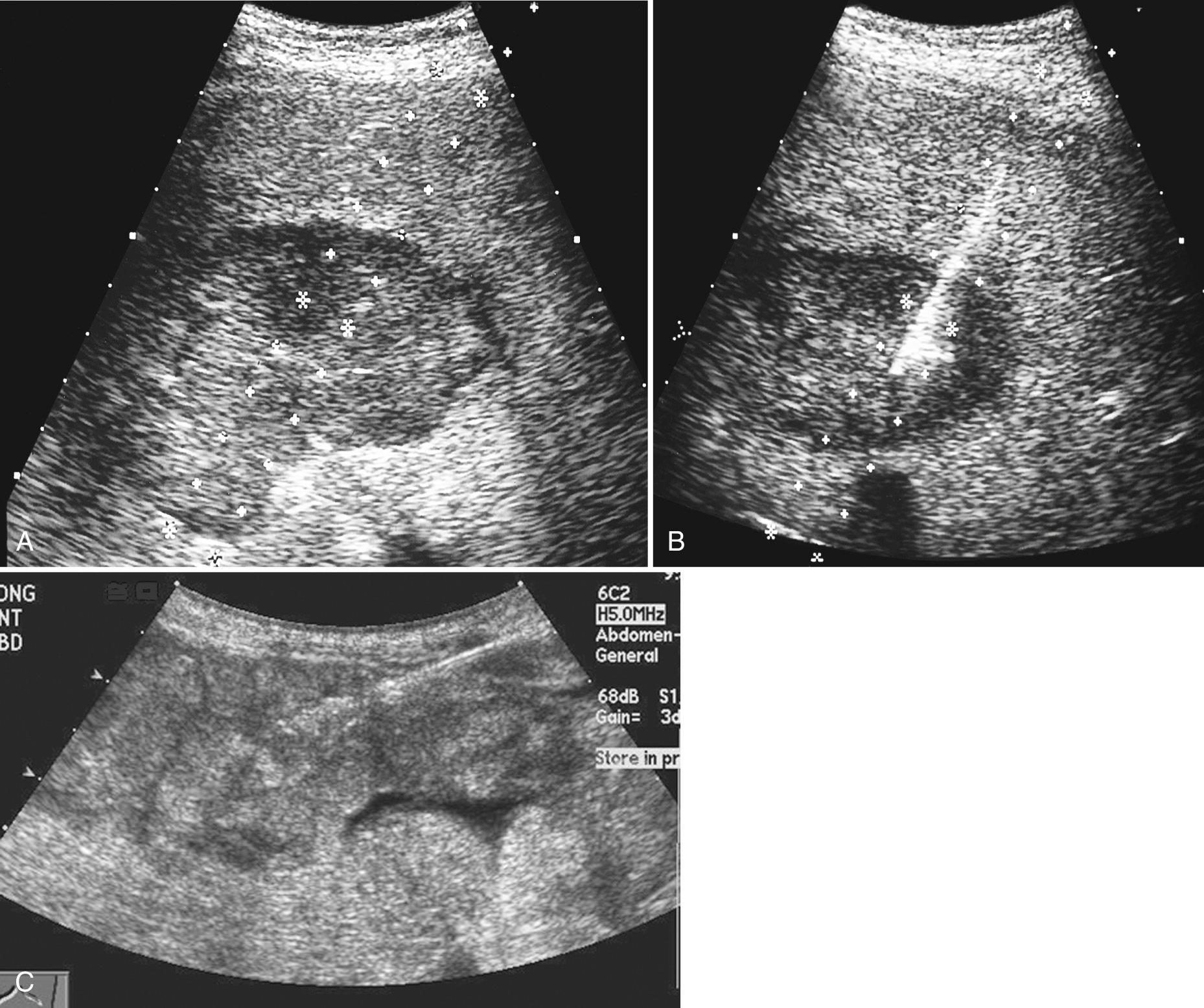
The liver is the abdominal organ in which percutaneous biopsy is most frequently performed. Common indications for biopsy include nonsurgical confirmation of metastatic disease, characterization of focal liver mass(es) with inconclusive imaging, and diagnosis of parenchymal disease, although random parenchymal biopsies have decreased at our own institution as a result of increasing utilization of elastography for liver fibrosis evaluation. Biopsy of large or superficial lesions is most easily done. With experience, deep lesions and lesions smaller than 1 cm can undergo accurate biopsy ( Fig. 17.4 ).
In our practice, liver biopsy is almost universally performed under ultrasound guidance because of the real-time visualization of the needle. This advantage becomes particularly obvious when there is significant movement of the liver caused by respiration and diaphragm excursion.
Lesions in the left lobe of the liver and in the inferior portion of the right lobe can usually undergo biopsy through a subcostal approach. Lesions located superiorly in the dome of the liver present a technical challenge for traditional CT-guided biopsy, but real-time, off-axial imaging with ultrasound allows for accurate needle targeting of such tumors, often through an intercostal approach. Although the intercostal approach may violate the pleural space, aerated lung is rarely punctured because it is well visualized sonographically and can be avoided. We usually place the patient in a left posterior oblique rather than supine position when an intercostal approach is used to improve visibility of the liver. If working along the right side of the patient, such a position also prevents the patient from watching needle manipulation. As feasible, orienting the transducer along the longitudinal axis of the patient is preferable. Such orientation minimizes the interference of respiration, because the tumor and needle remain in the field of view throughout the procedure.
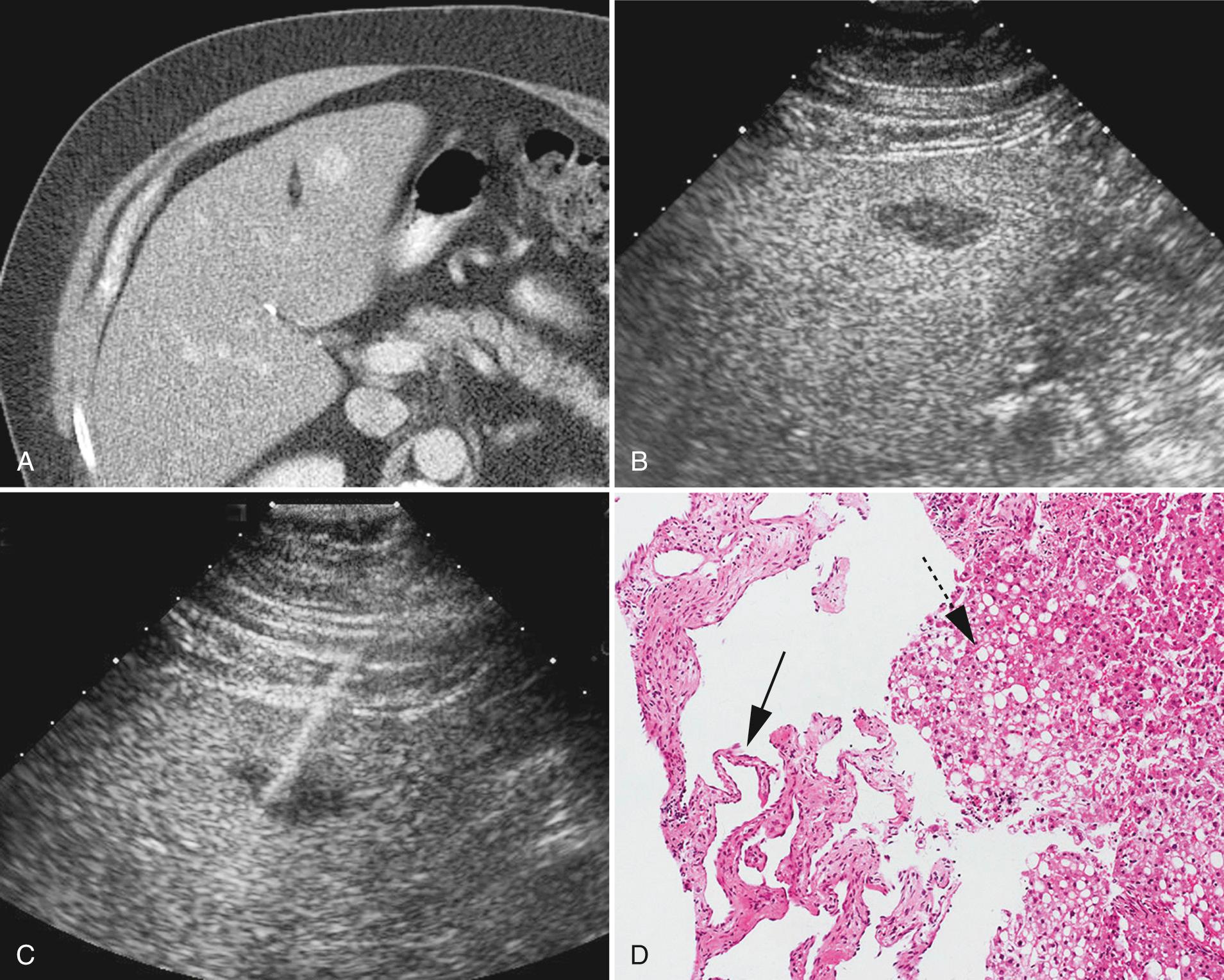
Benign hepatic lesions such as focal fatty infiltration, focal areas of normal liver within a fatty infiltrated liver, cavernous hemangiomas, focal nodular hyperplasia, and even atypical hemangiomas can usually be confidently characterized as benign by magnetic resonance imaging (MRI) of the liver. However, they occasionally mimic the appearance of malignancy on imaging studies. Biopsy of these processes can be done with ultrasound guidance to exclude malignancy and to confirm their benign nature if MRI findings are equivocal and especially if the patient has a known primary malignancy ( Fig. 17.5 ). Although cavernous hemangiomas are vascular lesions, these masses have undergone successful percutaneous biopsy without significant complications. Particular care must be taken to avoid direct puncture of cavernous hemangiomas without intervening liver parenchyma because this may result in significant bleeding. Normal overlying liver may tamponade potential bleeding from the hemangioma in these cases. Significant bleeding after direct puncture of hypovascular liver masses is less of a concern.
There has been increasing interest in biopsy of suspected hepatic adenomas as a result of evolving classification schemes and subtyping. Different subtypes carry different potential for bleeding and malignant transformation and this has implications for patient management. Although biopsy of hepatic adenoma is safe, there remains a small risk of discordant pathology results between initial biopsy and either subsequent biopsy or surgical resection specimen based on pitfalls in pathologic interpretation and occasional overlap in histologic features between adenoma, focal nodular hyperplasia, and hepatocellular carcinoma. In a series that included biopsy of 60 suspected hepatic adenomas, 6 (10%) showed discordant at time of follow-up pathology, including 4 later diagnosed as focal nodular hyperplasia and two later diagnosed as hepatocellular carcinoma.
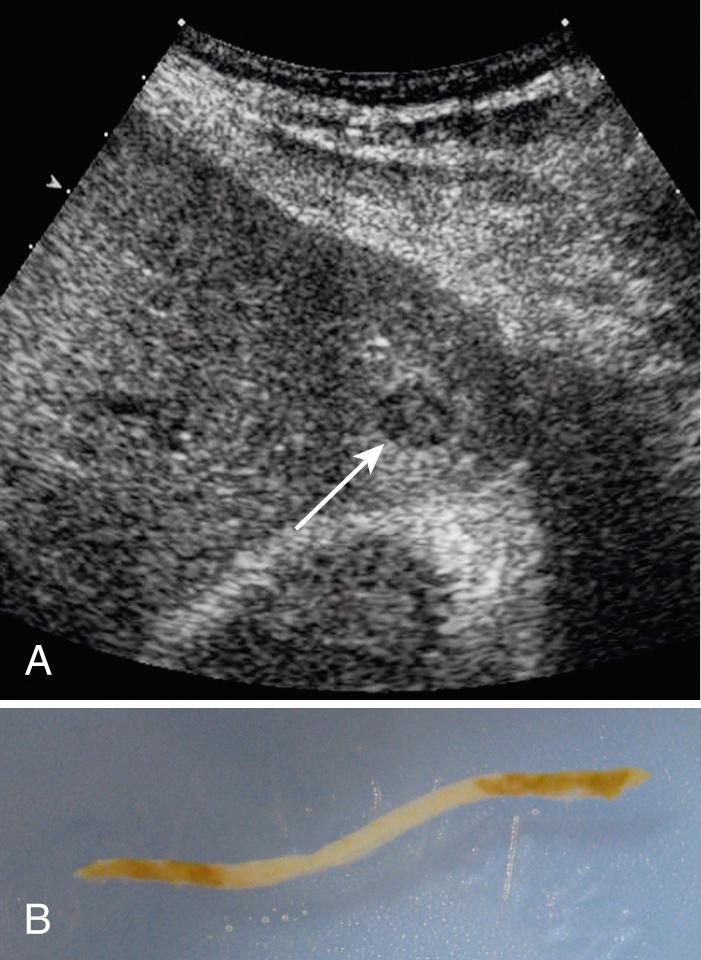
Percutaneous ultrasound-guided biopsy of portal vein thrombus has proved to be a safe and accurate diagnostic procedure for staging of hepatocellular carcinoma, although also performed less frequently in the context of advanced MRI techniques.
Liver biopsies are relatively safe, with an overall significant complication rate of less than 1%. Hemorrhage is most common. Such significant bleeding complications are more likely to occur in the biopsy of patients with malignancy and those with acute liver failure, chronic active hepatitis, or cirrhosis. Most complications occur soon after the biopsy procedure, with about 60% occurring within 2 hours and 80% within 10 hours. Several large series report mortality of percutaneous liver biopsy as 0.1% or less.
Despite the growing use of endoscopic ultrasound (EUS) and EUS-guided FNA, percutaneous biopsy of pancreatic tumors remains necessary in some cases when the tumor is in the tail of the pancreas or when EUS is unavailable. Biopsy is occasionally required to document malignancy or differentiate malignancy from a benign condition, such as focal pancreatitis.
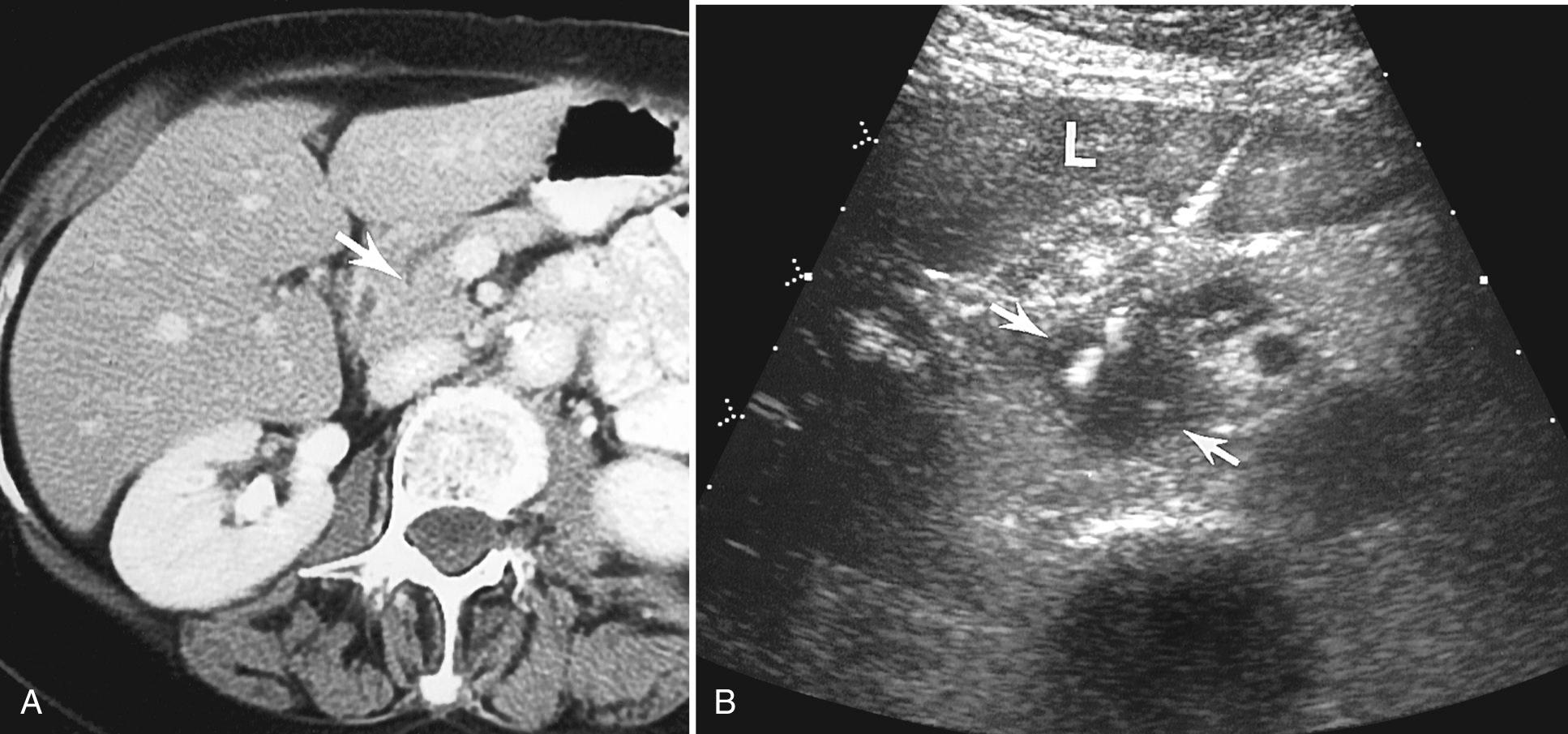
At our institution, most pancreatic biopsies are done with CT guidance because depth of the pancreas and presence of overlying bowel gas and hyperechoic abdominal fat can make visualization of the needle difficult. Nevertheless, biopsy of pancreatic masses in normal-size and slender patients can be done accurately under ultrasound guidance ( Fig. 17.6 ).
The gastrointestinal (GI) tract may be traversed when biopsying the pancreas. With ultrasound, the stomach or bowel is either displaced or compressed. Brandt et al. demonstrated the safety of traversing the GI tract (stomach, small bowel, colon) in performing percutaneous biopsies in 66 procedures. Most of these biopsies were performed using a 21-gauge needle, with no complications related to the biopsy route in these patients.
A particular advantage of ultrasound over CT is the ability to biopsy pancreatic masses in an off-axis plane, which is very useful if overlying vessels are present on CT. Ultrasound-guided biopsy has 93% to 95% accuracy, compared with 86% to 100% accuracy for CT guidance.
In some series, the biopsy success rate for the diagnosis of pancreatic carcinoma has been lower than the success rate for the diagnosis of malignant lesions in other organs of the abdomen. This may be related to sampling error, because significant desmoplastic reaction often accompanies pancreatic adenocarcinoma. By targeting the central hypoechoic portion of the pancreatic mass, the clinician can improve the diagnostic yield. In addition, core biopsy, either alone or in addition to FNA, results in improved diagnostic performance compared with FNA alone.
The differentiation between benign serous and potentially malignant mucinous pancreatic tumors can be difficult with imaging alone. Unfortunately, cystic pancreatic malignancies are difficult to accurately diagnose with percutaneous biopsy; a definitive diagnosis was achieved in only 60% of patients in one study. In biopsy of a cystic pancreatic lesion, it is critical to obtain epithelial cells, either in the wall of the lesion or within the cyst fluid. Analysis of percutaneous fluid aspirates from a cystic lesion has also been proposed as an aid to distinguish cystic neoplasms from pseudocysts. A high amylase level is consistent with a pseudocyst. The presence of tumor markers with the cyst fluid may also be helpful in suggesting a cystic neoplasm.
The safety of percutaneous biopsy of the pancreas has been well established, with a complication rate of 0.8% to 2%. A historic review reported six deaths related to pancreas biopsy. Five of these deaths were attributed to pancreatitis and one to sepsis. No pancreatic cancer was found in either the biopsy specimen or the postmortem examination of these patients, suggesting an increased risk for developing pancreatitis after biopsy of normal pancreas. In this same large review of percutaneous biopsies, 10 of 23 cases of needle track seeding occurred after the biopsy of pancreatic malignancies. For this reason, biopsy may not be indicated in patients who are surgical candidates.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here