Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Major fetal malformations are highly associated with fetal chromosomal abnormalities, particularly central nervous system anomalies, facial abnormalities, cystic hygroma, diaphragmatic hernia, cardiac defects, gastrointestinal abnormalities, genitourinary anomalies, nonimmune hydrops fetalis (NIHF), and abnormalities involving the extremities.
The combination of nuchal translucency (NT) measurement and maternal serum analytes, pregnancy-associated plasma protein-A (PAPP-A) and free β-hCG (human chorionic gonadotropin), is the most common aneuploidy screening paradigm in the first trimester of pregnancy.
Incorporation of first trimester nasal bone documentation into NT and serum screening can increase the detection rate of trisomy 21 without significantly altering the false positive rate.
The genetic sonogram is a targeted second trimester ultrasound examination that is performed at the time of the anatomic survey and assesses for major fetal malformations as well as minor markers of aneuploidy. The presence or absence of these markers, either alone or in combination, can adjust a patient's aneuploidy risk, specifically for trisomy 21.
Likelihood ratios (LRs) have been established for each individual sonographic marker of aneuploidy; they can be multiplied by the patient's a priori risk to determine the patient's posttest odds for aneuploidy.
Thickened nuchal skinfold and absent/hypoplastic nasal bone are the sonographic markers most specifically associated with trisomy 21 in the second trimester.
In a low-risk population, pyelectasis, echogenic intracardiac foci, and choroid plexus cysts are not associated with an increased risk for aneuploidy when observed in isolation.
The finding of one sonographic marker of aneuploidy should prompt a more targeted ultrasound examination to evaluate for additional signs of aneuploidy.
In addition to biochemical screening, sonography is a noninvasive method used to perform risk assessment for fetal aneuploidy. In addition to the major congenital anomalies discussed later and listed in Table 3-1 , multiple other first and second trimester ultrasound findings are associated with aneuploidy. Such findings, commonly referred to as minor markers or soft markers, typically are not structural anomalies per se and usually have no clinical significance to the fetus except for their association with aneuploidy. The presence or absence of these minor markers can be used to adjust a patient's a priori risk for aneuploidy based on biochemical screening results or maternal age. This becomes particularly important in screening for trisomy 21, as approximately 75% of fetuses affected by trisomy 21 will not have ultrasound-detectable major congenital anomalies at the time of the second trimester anatomic survey. This is in contrast to fetuses affected by trisomies 18 and 13, of which greater than 90% will have major structural malformations detectable by sonography in the second trimester of pregnancy.
| Trisomy 21 | Trisomy 13 | Trisomy 18 |
|---|---|---|
| AV canal defect | Cardiac defects | Cardiac defects |
| Duodenal atresia | CNS abnormalities | Spina bifida |
| Ventriculomegaly | Cleft lip/palate | Micrognathia |
| Other cardiac defects | Omphalocele | Omphalocele |
| Cystic hygroma | Midline facial anomalies | Clenched hands/wrists |
| Nonimmune hydrops | Echogenic kidneys | Radial aplasia |
| Urogenital anomalies | Clubfeet | |
| Polydactyly | Cerebellar dysgenesis | |
| Rocker bottom feet | Cystic hygroma | |
| Cystic hygroma | Nonimmune hydrops | |
| Nonimmune hydrops | ||
| Congenital diaphragmatic hernia | Congenital diaphragmatic hernia |
This chapter will review the most common first and second trimester ultrasound findings associated with fetal aneuploidy. We will discuss major malformations, as well as soft markers and their screening efficiency as well as their current role in aneuploidy risk calculation in the era of first trimester biochemical screening and prenatal screening using cell-free DNA (cfDNA).
Structural abnormalities are more common in aneuploid fetuses, particularly central nervous system anomalies, facial abnormalities, cystic hygroma, diaphragmatic hernia, cardiac defects, gastrointestinal abnormalities, genitourinary anomalies, NIHF, and abnormalities involving the extremities. The large majority of fetuses with trisomies 13 and 18 have multiple major structural anomalies. Fetuses with Down syndrome, in contrast, are less likely to have structural abnormalities identified by second trimester sonography; it is reported that just 25% of second trimester fetuses with Down syndrome have sonographically detectable major congenital anomalies. In two prenatal series before 20 weeks, structural anomalies were detected by sonography in only 16% to 17% of trisomy 21 fetuses.
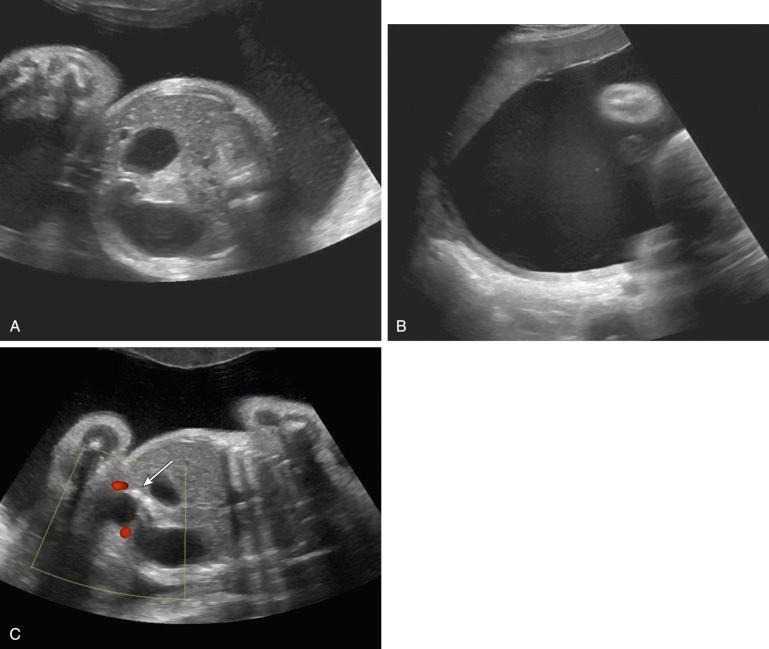
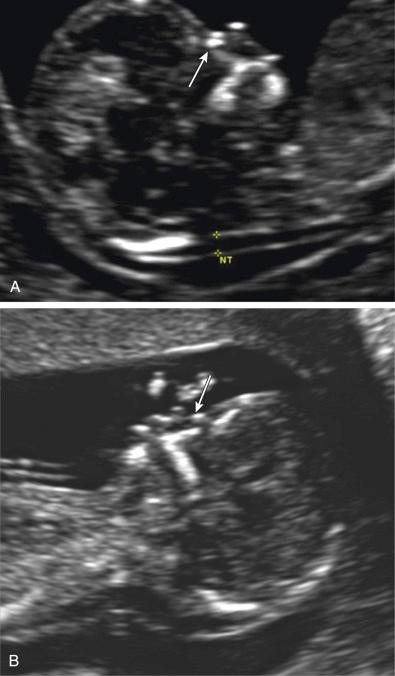
Identification of cardiac malformations on prenatal sonography substantially increases the risk for chromosomal abnormalities, with a frequency of aneuploidy reported to be as high as 22% to 32%. The frequency of aneuploidy varies with the type of cardiac defect present and is higher with hypoplastic heart ( Fig. 3-1 ), atrioventricular canal defects, tetralogy of Fallot, and double-outlet right ventricle as compared with isolated ventricular septal defects or valvular stenosis. Atrioventricular canal defects have a very high risk of aneuploidy, particularly Down syndrome. In one series of 38 atrioventricular septal defects, aneuploidy was present in 22 (58%), with Down syndrome ( n = 19), trisomy 18 ( n = 1), trisomy 13 ( n = 1), and mosaicism ( n = 1) all identified.

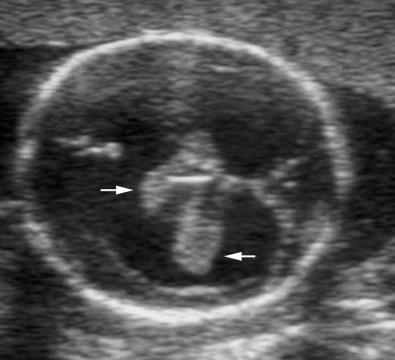
Approximately 50% of infants with Down syndrome have cardiac defects. However, most of these are ventricular septal defects ( Fig. 3-2 ) and common atrioventricular canal defects ( Fig. 3-3 ), and their detection by prenatal sonography is quite variable. One study reported that heart defects were detected in just over one half of fetuses with Down syndrome. DeVore reported that nonspecific cardiac findings (such as tricuspid regurgitation, pericardial effusion, and right-left disproportion) were present in 76% of fetuses with Down syndrome, whereas just 9% had a characteristic atrioventricular septal defect. In contrast, cardiac malformations are present in more than 90% of fetuses with trisomy 18 and 13. Studies have reported that major congenital heart defects can be identified sonographically in over 80% of fetuses with trisomy 18.


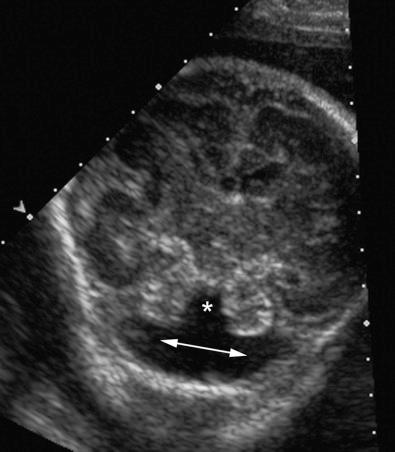
Duodenal atresia ( Fig. 3-4 ) is rarely recognized until after 20 to 24 weeks of pregnancy, when the characteristic double bubble sign (dilated fluid-filled stomach and proximal duodenum) and polyhydramnios become apparent. Duodenal atresia is the leading cause of intestinal obstruction among newborns and is highly associated with Down syndrome. Among cases of duodenal atresia detected prenatally, trisomy 21 is present in approximately one third of cases.
The differential diagnosis of NIHF is extensive ( Fig. 3-5 ); this disorder can result from a variety of both maternal and fetal causes. NIHF is recognized sonographically by ascites, pericardial effusions, pleural effusions, polyhydramnios, thickened placenta, and skin edema (see Chapter 17 ). Aneuploidy is a common cause of NIHF, accounting for up to 16% of cases. The most common karyotype abnormalities associated with hydrops include Turner syndrome (45,X); trisomies 21, 18, and 13; and triploidy. NIHF is most highly associated with aneuploidy when diagnosed earlier in pregnancy; a higher incidence of aneuploidy is identified in the second trimester as compared with the latter half of pregnancy. The combination of generalized hydrops and cystic hygroma is often referred to as lymphangiectasia, which has a very poor prognosis. Lymphangiectasia is associated with aneuploidy, especially Turner syndrome, in approximately two thirds of cases ( Fig. 3-6 ).


Hydrothorax (pleural effusion, chylothorax) has been linked to aneuploidy, especially Turner syndrome, Down syndrome, and trisomy 13. Among 82 cases of isolated fetal pleural effusion ( Fig. 3-7 ) reported in the literature, Down syndrome was present in 4.9%. Ascites (see Fig. 3-5 ) may also occur in isolation without other signs of hydrops. This finding has also been associated with aneuploidy; in one report of 18 fetuses with ascites, 5.6% ( n = 1) had Down syndrome.

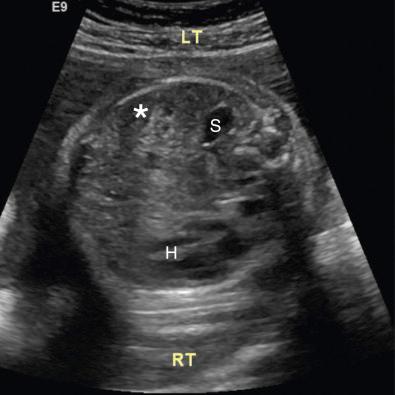
Diaphragmatic hernia ( Fig. 3-8 ) results from a congenital defect in the fetal diaphragm, with herniation of abdominal viscera into the fetal chest (see Chapter 12 ). This abnormality carries an increased risk for aneuploidy, particularly trisomy 18 (most common), trisomy 13, Down syndrome, Turner syndrome, and other chromosomal abnormalities. The frequency of aneuploidy is reported to be as high as 34%, although it generally ranges from 10% to 20% in reported series.
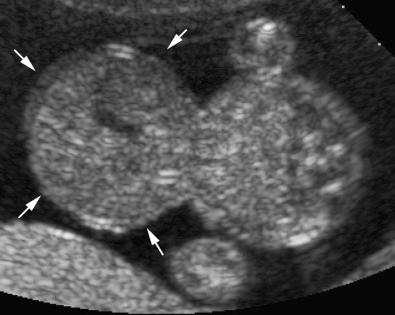
An omphalocele ( Figs. 3-9 and 3-10 ) occurs when there is a central abdominal wall defect that results in herniation of intra-abdominal structures into the base of the umbilical cord, which is covered by a membrane. Omphaloceles are associated with other fetal anomalies and aneuploidy, which complicates more than half of prenatally diagnosed cases. Associated aneuploidies include trisomies 18 and 13 (which are most frequent), Down syndrome, Turner syndrome, and triploidy. Similarly to other fetal malformations, there appears to be a higher frequency of aneuploidy in prenatal (30-40%) as compared with neonatal studies (which have a combined rate of 12%) owing to in utero lethality. In one study of 35 cases of prenatally diagnosed omphalocele, 54% had aneuploidy: trisomy 18 ( n = 17), triploidy ( n = 1), and Klinefelter syndrome ( n = 1). Small omphaloceles containing only bowel (see Fig. 3-10 ) have a higher aneuploidy risk than those containing liver, with one series reporting an aneuploidy rate of 87% in bowel only omphaloceles versus 9% in those containing liver ( Fig. 3-11 ).


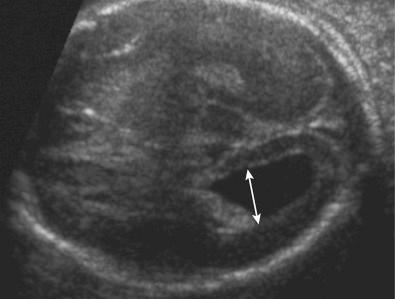
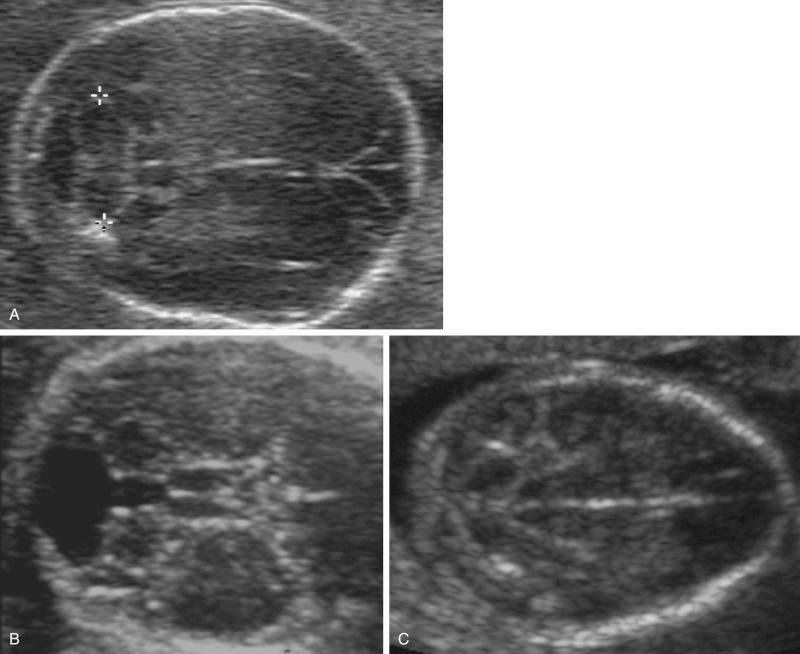
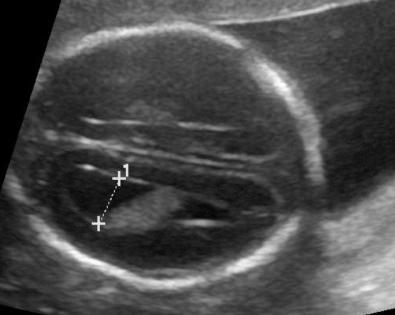
Many central nervous system abnormalities carry an increased risk for fetal aneuploidy. Cerebral ventriculomegaly ( Fig. 3-12 ), which is diagnosed when the atrial diameter of the cranial lateral ventricle reaches 10 mm or more, is relatively common finding on prenatal sonography. Ventriculomegaly (even mild) is associated with an increased risk for aneuploidy, particularly Down syndrome. However, mild ventriculomegaly may also be seen as a normal variant in the second trimester (after 20 weeks' gestation) and in male fetuses. In one study of 31 fetuses with isolated borderline ventriculomegaly (10-15 mm), 9.7% ( n = 3) were found to have aneuploidy (Down syndrome [ n = 2] and trisomy 13 [ n = 1]). In large series, 3.8% of fetuses with mild ventriculomegaly are karyotypically abnormal, with Down syndrome the most common aneuploidy. In chromosomally normal, aneuploid, and Down syndrome fetuses, mild ventriculomegaly is observed in 0.5%, 6.8%, and 5.5%, respectively.
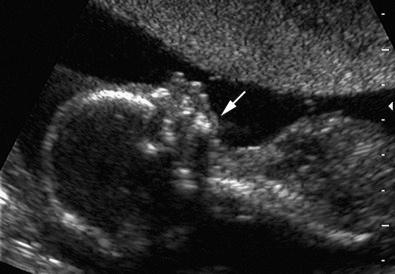
Hydrocephalus ( Fig. 3-13 ) and spina bifida ( Fig. 3-14 ) are both associated with chromosomal abnormalities, primarily trisomy 18, trisomy 13, and triploidy. In a review of 107 fetuses with central nervous system abnormalities, aneuploidy was found in 3%, 8%, and 33% of fetuses with hydrocephalus, hydrocephalus and spina bifida, and spina bifida alone, respectively. In one study of 38 fetuses with trisomy 18, 19% had neural tube defects and 8% had ventriculomegaly or hydrocephalus.

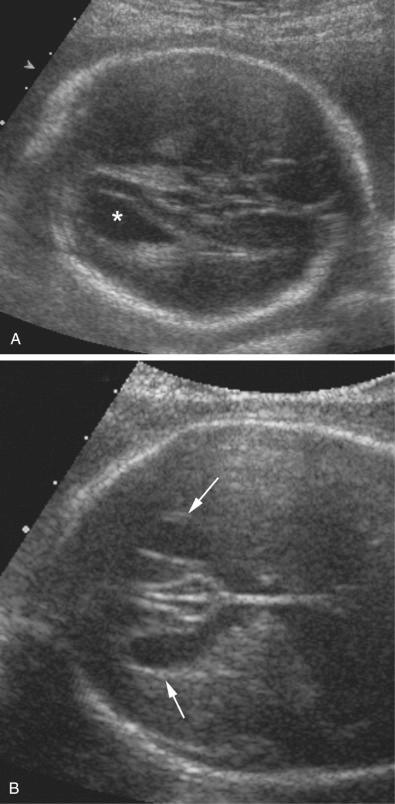
Cerebellar abnormalities, such as Dandy-Walker malformation (DWM) or cerebellar hypoplasia, are associated with an increased risk for aneuploidy ( Figs. 3-15 to 3-17 ). Trisomy 18 is the most common aneuploidy seen with these anomalies, but other chromosomal abnormalities may also be observed. Agenesis of the corpus callosum ( Fig. 3-18 ) can be complete or partial. The diagnosis is made by showing absence of the complex formed by the corpus callosum and cavum septum pellucidum, along with various other sonographic findings such as colpocephaly (disproportionate enlargement of the occipital horns) ( Fig. 3-19 ). Aneuploidy is reported in approximately 20% of prenatally diagnosed cases, primarily trisomies 18, 8, and 13, although a variety of other chromosomal abnormalities are also reported. A study reported in 2009 examined cases of agenesis of the corpus callosum diagnosed prenatally and postnatally. Among the prenatally diagnosed cases, aneuploidy was present in 8%, as compared with 4% in postnatal cases.

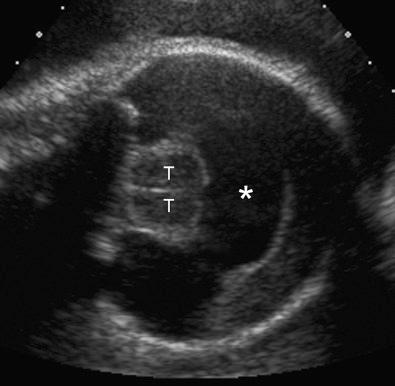
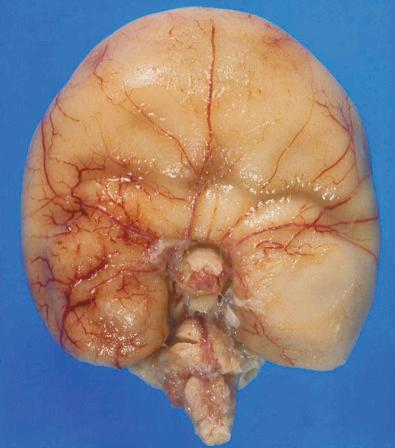
Holoprosencephaly ( Figs. 3-20 and 3-21 ) is a midline abnormality of the brain, resulting from absent or incomplete division of the prosencephalon (embryonic forebrain) and formation of the midline structures. It is embryologically related to development of the midface, hence the common association with median facial anomalies ( Fig. 3-22 ). There are three major types of holoprosencephalies, depending on the degree of anatomic abnormality: alobar, semilobar, and lobar. Aneuploidy is present in 50% to 60% of fetuses with alobar or semilobar holoprosencephaly. Of the various types of chromosomal abnormalities, trisomy 13 or a variant of trisomy 13 is the most common (found in 50-75% of those with abnormal karyotype). However, a wide variety of other aneuploidies has been reported. In fetuses with trisomy 13, holoprosencephaly was reported in 39%. When other abnormalities are present, in addition to holoprosencephaly, the risk for aneuploidy is increased.

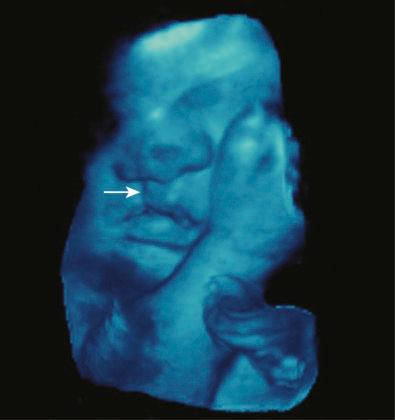
Abnormalities of the facial profile are common in fetuses or neonates with chromosomal abnormalities. Some chromosomally abnormal fetuses or neonates demonstrate micrognathia ( Figs. 3-23 and 3-24 ), a sloping forehead (see Fig. 3-24 ), flattened profile ( Fig. 3-25 ), or retrognathia . In one study examining the sonographic features of 38 fetuses with trisomy 18, approximately one half (53%) had facial anomalies identified. Twenty-nine percent had an abnormal profile (excluding micrognathia), 21% had micrognathia, and 18% had hypotelorism.


The presence of cleft lip/palate ( Figs. 3-26 and 3-27 ) is associated with aneuploidy such as trisomies 13 and 18, especially when other anomalies are also present. One study of fetuses with cleft lip and palate reported aneuploidy in 0%, 32%, 59%, and 82% in unilateral cleft lip, unilateral cleft lip and palate, bilateral cleft lip and palate, and median cleft lip and palate, respectively.

Ocular anomalies, such as hypotelorism ( Fig. 3-28 ), hypertelorism, microphthalmia, anophthalmia, and cyclopia (see Fig. 3-22 ), can be associated with fetal chromosomal abnormalities. Most importantly, when they are seen along with other malformations (especially holoprosencephaly), the risk of aneuploidy is particularly increased.

Genitourinary abnormalities can be associated with fetal chromosomal abnormalities. The highest frequency of aneuploidy has been reported in those fetuses with urethrovesical obstruction (bladder outlet obstruction), most commonly trisomy 18 or 13. In one cohort of 39 fetuses with obstruction at or distal to the urethrovesical junction, chromosomal abnormalities were reported in 23%. With urinary tract abnormalities that are more proximal, aneuploidy is reported with less frequency. In unilateral renal abnormalities such as ureteropelvic junction obstruction and multicystic dysplastic kidneys, the risk of aneuploidy is low.
Although the presence of most congenital malformations significantly increases the risk for fetal aneuploidy, there are some notable exceptions. They generally involve disorders that are thought to result from tissue or vascular disruption, such as gastroschisis, tumors, limb-body wall complex, hydranencephaly, and amniotic band syndrome .
The term nuchal translucency (NT) was first coined by Nicolaides and colleagues in 1992 to describe the finding of an increased translucent region behind the neck of fetuses who were diagnosed with aneuploidy at the time of chorionic villus sampling. This group published the first large cohort study on the association between NT and aneuploidy in 1995. This sonographic marker for aneuploidy was subsequently validated by several investigators and is now an integral component of most first trimester screening tests for chromosomal disorders. Despite widespread use of the NT measurement, the pathologic basis for enlargement of the NT in fetuses with aneuploidy is not known. Suggested mechanisms include a decrease in cardiac function and impaired circulation, increased collagen and hyaluronan content within fetal skin, dysfunction within the jugular-lymphatic drainage system, and increased intrathoracic pressure.
The most common first trimester screening paradigm combines the measurement of the NT with serum markers including PAPP-A and hCG to modify a woman's a priori risk for aneuploidy based on her age. The reported sensitivity for trisomy 21 detection using the combined first trimester approach alone ranges from 80% to 91%, with a specificity of 91% to 96%. When the first trimester approach is combined with second trimester serum markers including unconjugated estriol, alpha-fetoprotein, and inhibin A in a modified sequential or integrated protocol, the sensitivity approaches 95% with specificity ranging from 95% to 98%.
Detection rates for aneuploidies other than trisomy 21 are lower, but the NT is similarly enlarged, with many different chromosomal abnormalities. The combined first trimester screening test or the presence of cystic hygroma detected 78% of all non–Down syndrome aneuploidies with a 6% false positive rate in the FASTER (First and Second Trimester Evaluation of Risk) trial, a large multicenter trial of aneuploidy screening in over 30,000 pregnant women.
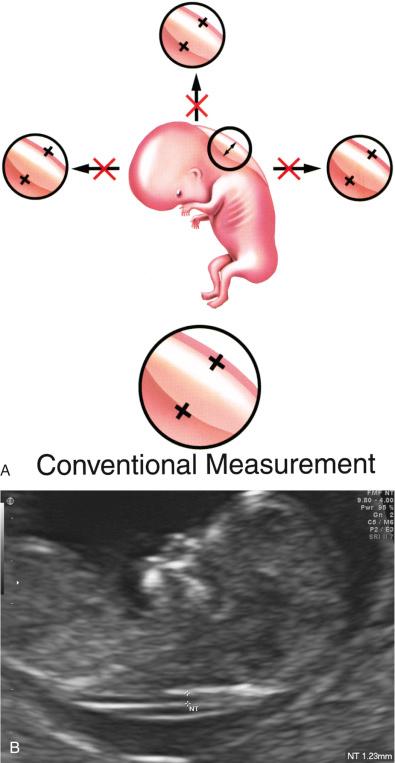
It is important to emphasize the need for meticulous technique in evaluating the NT, which must be measured accurately to achieve the previously described screening efficiency. An important observation since the introduction of NT-based aneuploidy screening is the importance of maintaining good quality measurements to achieve optimal screening effectiveness. Unlike biochemical markers that display low interrater variability, NT measurement can be subject to large interobserver variation if not performed under a strict protocol. Measurements should be performed when the crown-rump length measurement is between 36 and 84 mm, depending on the laboratory used. In addition, some important criteria must be fulfilled for a good quality measurement ( Fig. 3-29 ):
The image should be magnified to occupy 75% of the screen and should show only the fetal head, neck, and upper thorax.
The fetus must be in the midsagittal plane.
The fetal neck must be in a neutral position—not hyperextended or hyperflexed.
Three echogenic lines indicating the inner and outer borders of the fetal skin and the amnion must be displayed.
The ultrasound calipers must be placed with the horizontal cross on the inner borders of the echolucent space and perpendicular to the fetal axis.
The measurement of the NT must be taken at the widest space.
The impact of poor quality measurements of the NT on aneuploidy detection can be twofold. Undermeasurement can result in lower detection rates, whereas exaggerated measurement can increase the false positive rate. A modeling study by Cuckle suggested that a 10% undermeasurement may result in a 6% reduction in the trisomy 21 detection rate. In a multicenter study published shortly after the introduction of NT-based screening, the importance of adequate training and monitoring of sonographers was highlighted by a reported low detection rate for Down syndrome of 31%. The Nuchal Translucency Quality Review (NTQR) program and the Fetal Medicine Foundation are two organizations that provide NT training, certification, and oversight and have helped ensure maintenance of high-quality programs offering first trimester screening. Despite the institution of these quality assurance steps, a 2015 review of approximately 1.5 million ultrasound images performed for NT measurement still revealed wide variability among providers, with the more experienced providers demonstrating measurements closer to the expected norms.
When NT-based screening was first introduced, absolute or categoric NT cutoffs were suggested to define an abnormal screening result. It was soon realized that the NT increases with gestational age even in the short-term window between the 10th and 14th weeks when these tests are performed. Therefore, NT measurements must be adjusted for gestational age. The approach to adjusting involves converting the NT to multiples of the median (MoM) for gestational age and using either the 95th percentile for the MoM or the delta value of the observed NT from that expected for the gestational age or crown-rump length. Sophisticated software is used to perform such calculations, and these measurements are now considered the gold standard. However, it is also important to note that an enlarged NT (greater than 3.0 mm) may be considered an indication for diagnostic testing, regardless of gestational age correction, given that the risk for aneuploidy exceeds 1 in 6 at this threshold. Further adjustment using first trimester serum analytes will not significantly alter the risk for aneuploidy in most cases.
Cystic hygromas represent an abnormality of the fetal lymphatic system and occur in approximately 1 in 285 first trimester pregnancies. This diagnosis is made when the nuchal space is enlarged with large posterior or posterolateral fluid-filled cavities noted within the fetal neck, with or without the presence of septations. This edema can extend caudally along the upper back of the fetus ( Fig. 3-30 ). The presence of a cystic hygroma in the first trimester confers a 50% risk for fetal aneuploidy, with the most common chromosomal abnormalities being Turner syndrome (45,X), trisomy 21, and trisomy 18. In euploid fetuses with cystic hygomas, 50% to 60% will be diagnosed with major fetal structural abnormalities later in pregnancy. Debate continues as to whether cystic hygromas represent a continuum of thickened NT and if the presence or absence of septations alters the aneuploidy risk. Based on the available data, it would appear that in the presence of either a thickened NT or cystic hygroma with or without septations, the aneuploidy risk remains comparably very high, and this distinction is clinically relatively unimportant. In either case, invasive diagnostic testing should be offered.

The appearance of a small nose with a low nasal bridge in children and adults with Down syndrome initially led to the investigation of the fetal nasal bone as a marker for this condition. In 2002, Sonek and Nicolaides reported on three unselected first trimester fetuses with Down syndrome. Two of those fetuses had sonographically undetectable nasal bones, and the third had a nasal bone that was below the 2.5th percentile in length for gestational age. A 2003 study performed NT screening on 5532 fetuses from 5425 pregnancies and found that the nasal bone was absent in 70% of fetuses with Down syndrome versus in 0.2% of euploid fetuses. Not only did the authors show an association of absent nasal bone with Down syndrome, but they also demonstrated that appropriate imaging of the nasal bone was attainable in a large percentage of the study population, with a 99.8% visualization rate.
Additional studies have confirmed the association of absent nasal bone and Down syndrome. One study demonstrated that a successful view of the fetal profile could be obtained in 1752 of 1906 consecutive fetuses undergoing NT scanning (91.9%). In this study, the nasal bone was absent or hypoplastic in 12 of 19 fetuses with chromosomal abnormalities and in 8 of 10 with trisomy 21. Absence of the nasal bone was recorded in only 24 of 1733 chromosomally normal fetuses (1.4%). In an additional study, investigators successfully assessed the nasal bone in 1027 of 1089 (94.3%) fetuses and found that the nasal bone was absent in 10 of 1000 (1.0%) unaffected cases and in 10 of 15 (66.7%) Down syndrome cases.
To assess the nasal bone sonographically, the fetal profile is first viewed in the midsagittal plane. The transducer can then be rocked sideways to maintain the angle of insonation at 45 or 135 degrees. The nasal bone is visualized as an echogenic line below and parallel to the overlying skin. When present, the nasal bone and skin appear similar to an equal sign ( Fig. 3-31 ). Although obtaining sonographic images of the fetal nasal bone is straightforward, there is a learning curve associated with developing proficiency. In 2003, Cicero and colleagues determined that it took sonographers with NT imaging expertise an average of 80 nasal bone images, with a range of 40 to 120, to become competent in examining the fetal nasal bone.
Recent research has attempted to incorporate nasal bone evaluation into current first trimester screening protocols in order to improve the accuracy of aneuploidy diagnosis. In 2005, a prospective cohort study assessing the utility of incorporating nasal bone assessment into screening with standard first trimester markers (NT, free β-hCG, PAPP-A) was performed. Incorporating nasal bone measurement improved the detection rate of Down syndrome to 90% and reduced the false positive rate to 2.5%. Cicero and colleagues observed similar results with the incorporation of fetal nasal bone into first trimester screening.
It has been noted that race and ethnicity are associated with an absent nasal bone. In a study reported in 2003, in 3358 karyotypically normal fetuses, absent nasal bone was identified in 2.8% of Caucasians, 10.4% of African Caribbeans, and 6.8% of Asians. The finding of racial variation and absent nasal bone was reinforced by another large series of patients. In that study, the fetal profile was successfully examined in 5851 cases (98.9%), and absent nasal bone in chromosomally normal fetuses was seen in 2.2% of Caucasians, 9.0% of African Caribbeans, and 5.0% of Asians. These findings have led investigators to question whether the simple presence or absence of the nasal bone is applicable when evaluating the nasal bone in the first trimester, given that race and ethnicity may not be known or easily incorporated into risk adjustment.
The ductus venosus is a unique fetal blood vessel that shunts highly oxygenated blood from the umbilical vein to the right atrium, after which it is shunted through the foramen ovale to provide oxygenated blood to the fetal circulation. Doppler study of the ductus venosus normally will show triphasic, pulsatile forward flow. However, an absent or reversed a wave during atrial systole has been observed in cases of fetal cardiac malformations and aneuploidy. In 1998, Matias and colleagues demonstrated the feasibility of first trimester ductus venosus Doppler sonography to screen for aneuploidy, showing that 57 of 63 (90.5%) chromosomally abnormal fetuses had either an absent or reversed a wave. A subsequent study by Prefumo and colleagues demonstrated a positive LR of 7.05 for Down syndrome in the setting of abnormal ductus venosus flow in a high-risk population undergoing chorionic villus sampling. Using ductus venosus Doppler studies as an adjunct to NT screening appears to be more discriminatory than using either test alone.
In chromosomally normal fetuses with a normal NT, abnormal ductus venosus blood flow in the first trimester has been associated with adverse fetal outcome such as congenital heart disease and fetal growth restriction. Despite these reports, the technical feasibility of successfully interrogating such a small fetal vessel (~2 mm) with Doppler sonography in the first trimester of pregnancy may preclude its practical use in screening for fetal abnormalities.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here