Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acute aortic dissection is one of the most common catastrophes involving the aorta. Dissection of the aorta is characterized by the separation of the aortic media by pulsatile blood, with variable extents of proximal and distal extension along the aorta and its branches. The process of dissection creates a false lumen in the aortic wall that parallels the aortic true lumen. In the majority of cases, a primary intimal tear initiates the dissection and allows blood flow communication between the true and false lumens, which are separated by a dissection flap or septum. Because this acute event is rarely associated with a preexisting aneurysm and the aortic intima (true lumen) is actually smaller than normal, the older term dissecting aneurysm is misleading and inappropriate; to be semantically correct, an aortic dissection should be called a false aneurysm . A thorough understanding of the pathophysiology of aortic dissection is critical for prompt diagnosis and effective management in the acute setting. On the other hand, aortic dissection in its chronic phase is responsible for a substantial proportion of thoracic aortic disease and aortic rupture due to false aneurysmal degeneration of the false lumen. Numerous advances in diagnostic modalities, medical and surgical treatment, and long-term management have changed the prognosis for patients with this lethal condition. This chapter summarizes current knowledge regarding the diagnosis and treatment of Stanford type A aortic dissection.
The observations by Morgagni in 1761 were followed by multiple early anatomic and postmortem reports describing aortic dissection, including the famous autopsy report on King George II of England in 1776. In 1802, Maunoir, describing this disease, used the term dissection . Almost 20 years later, René Laennec coined the term aneurysme dissequant, or dissecting aneurysm, believing that this entity represented the early stage of a saccular aneurysm. Later, in 1863, Peacock published a comprehensive review of 80 cases of aortic dissection. Until the last half of the twentieth century, the diagnosis of aortic dissection was almost exclusively an autopsy finding. Antemortem diagnosis was made in only 6 of 300 cases reviewed by Shennan in 1934. The use of contrast angiography for the diagnosis of aortic dissection was reported by Paullin and James. The first attempt to treat this condition was described in 1935 by Gurin and colleagues, who used surgical iliac artery fenestration to relieve lower extremity ischemia. Although quickly abandoned, cellophane wrapping of the dissected aorta was also attempted to prevent rupture. In 1955, DeBakey and associates launched the modern era of surgical management with graft replacement of the dissected aorta. Subsequently, the same group introduced the use of cardiopulmonary bypass during clamping of the descending thoracic aorta. The first large clinical series of patients with an aortic dissection was published in 1958 by Hirst and colleagues ; analyzing 505 cases allowed these authors to emphasize the high mortality rate and the glaring rarity of antemortem diagnosis at that time. The modern medical approach to aortic dissection with use of pharmacologic agents to diminish aortic dP/dt (anti-impulse therapy) was introduced by Wheat and associates in 1965. The venerable DeBakey type I, II, III classification of aortic dissection was introduced the same year. The simplified Stanford classification system (type A or type B) based on pathophysiologic characteristics was proposed in 1970 by Daily and colleagues. Since then, other important advances have followed, such as less invasive and more accurate diagnostic modalities, improved anesthetic methods, safer extracorporeal perfusion techniques, profound hypothermic circulatory arrest for thoracic aortic arch surgery (introduced by Griepp and coworkers from Stanford in 1975), improved and safer prosthetic vascular grafts, and refinement of cardiovascular surgical techniques.
It is important to understand and to apply accurately the classification of aortic dissection in order to treat patients most appropriately and to compare rigorously the results of various medical and surgical therapeutic interventions reported from different institutions. Considerable confusion about classifying aortic dissections has arisen in the past. Numerous systems have been proposed, beginning in 1955 with nine categories initially suggested by DeBakey and associates. The more widely used DeBakey type I, type II, and type III three-category classification scheme was introduced in 1965 ; importantly, DeBakey modified this scheme in 1982 to conform with the Stanford A/B functional criteria based on whether the ascending aorta is involved, regardless of the location of the tear and distal extent of dissection. Despite the use of different labels, a consensus has emerged concerning the essential elements of a common functional classification system of aortic dissection. The key point of all classification systems used today is the presence or absence of involvement of the ascending aorta, regardless of the location of the primary intimal tear and irrespective of the antegrade extension of the dissection process. The simplified Stanford classification approach as proposed by Daily and associates in 1970 has gained broad acceptance during the past 44 years. If the dissection involves the ascending aorta, it is a Stanford type A, which corresponds to a DeBakey type I, University of Alabama “ascending,” Massachusetts General Hospital “proximal,” and Najafi “anterior” dissection. Both DeBakey type I and type II dissections involve the ascending aorta; type I extends beyond the innominate artery, whereas type II is confined just to the ascending aorta. If the ascending aorta proximal to the innominate artery is not involved in the process, the dissection is called a Stanford type B, DeBakey type III, descending, distal, or posterior dissection ( Fig. 70-1 ), even though many of these patients have some limited extent of retrograde dissection involvement in the arch, a point that is not broadly appreciated. A subtype of dissection in which the primary intimal tear is in the descending aorta or even farther distal, yet the dissection process propagates in a retrograde fashion to involve the arch and ascending aorta, was originally termed a DeBakey type III-D by Reul and colleagues in 1975, but now is simply termed a retro-A dissection . Retro-A dissections constitute approximately 6% of all type A dissections, and recently they have been seen more frequently as a complication of stent-graft descending thoracic endovascular aortic repair (TEVAR).
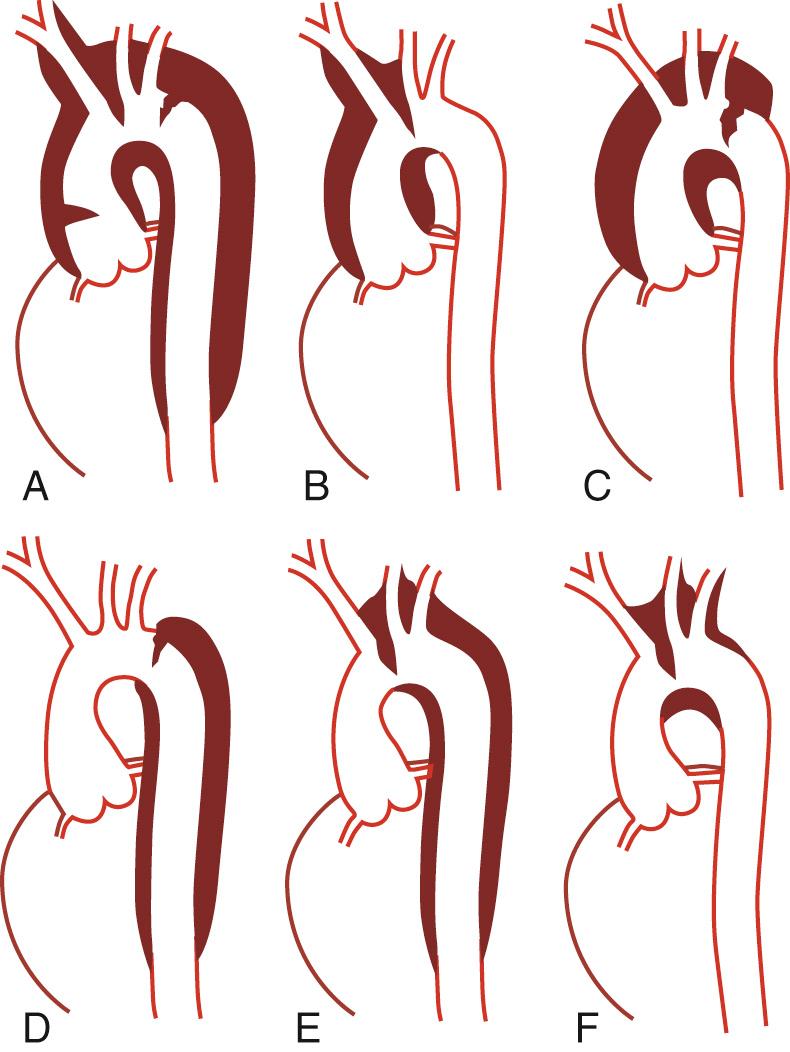
This functional classification approach reflects the pathophysiology of aortic dissection, considering that involvement of the ascending aorta is the principal predictor of the biological behavior of the disease process and the most common fatal complications; moreover, it simplifies diagnosis because it is easier to identify involvement of the ascending aorta accurately than to determine the exact site of the primary intimal tear (or tears) or the extent of propagation of the dissection process. Furthermore, the Stanford classification system facilitates clinical decision making and expedites definitive management. Patients with acute Stanford type A dissections should be treated surgically in essentially all cases; individuals with Stanford type B dissections can be treated with open surgical intervention, with an endovascular TEVAR, or with medical management, depending on the presence or absence of major complications. More specifically, patients with type A dissections require a median sternotomy, total cardiopulmonary bypass (CPB), and profound hypothermic circulatory arrest (PHCA); those with type B dissections are approached surgically using a left posterolateral thoracotomy, total CPB with PHCA, partial CPB, or isolated left heart bypass.
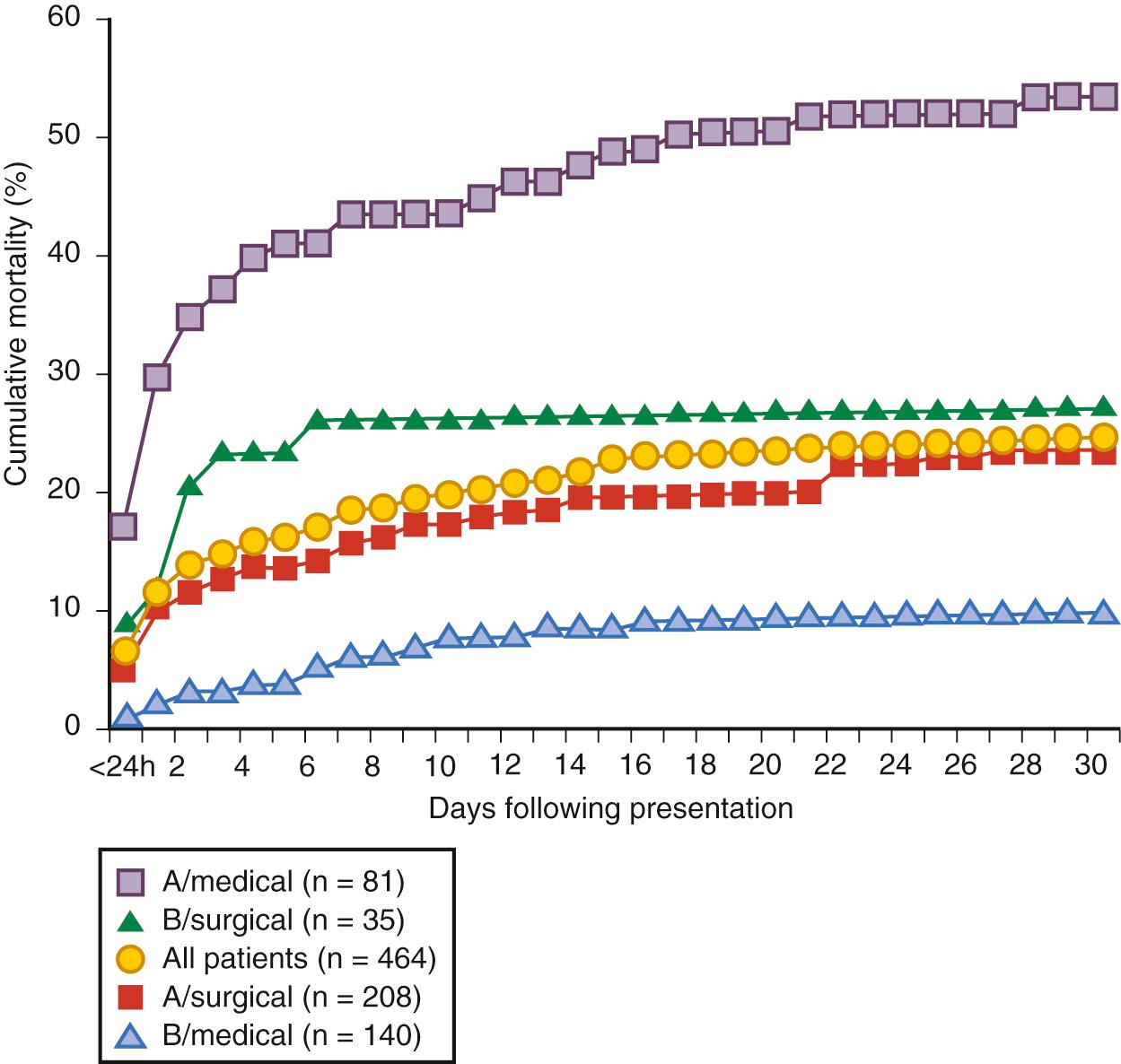
Aortic dissections diagnosed within 14 days of the onset of presenting symptoms are defined as acute; those diagnosed more than 14 days after onset are classified as chronic dissections. According to the International Registry of Acute Aortic Dissection (IRAD) investigators, the cumulative mortality after acute type A and type B dissection treated medically reached a plateau after the fourteenth day after presentation, demonstrating the prognostic importance of this venerable but arbitrary 14-day time distinction ( Fig. 70-2 ). DeBakey and colleagues introduced the term subacute to describe dissections between 2 weeks and 2 months old, but this distinction has been rarely used; however, the term subacute has recently gained popularity because of the use of TEVAR and can mean anything between 2 weeks and 6 or more months. Its use should be rejected because it is ambiguous.
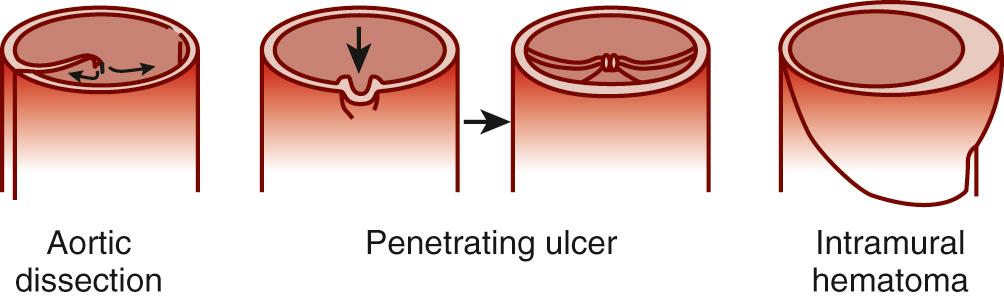
During the past two decades, advances in vascular imaging technology have led to increasing recognition of intramural hematoma (IMH) and penetrating atherosclerotic ulcers (PAUs) as distinct pathologic variants in the spectrum of acute aortic diseases, which can evolve into classic aortic dissection. Both are characterized by the absence of the classic intimal flap dividing the aorta into true and false channels. IMH can be caused by an ulcer penetrating into the internal elastic lamina or can occur spontaneously without any intimal disruption. IMH can involve the ascending aorta (type A IMH) as well as the descending aorta (type B IMH). On occasion, IMH can suddenly evolve into classic aortic dissection with blood flow in both lumens, as different phases of a dynamic aortic pathologic process. PAUs occur most commonly in the descending thoracic aorta in older patients. Distinguishing IMH (with or without a PAU) or PAU from classic aortic dissection is critical because the pathophysiologic process, clinical behavior, prognosis, and management of these lesions can differ, depending on which segment of the aorta is involved and the patient's symptomatic status.
Aortic dissection is seen in all age groups, although the majority of the cases occur between the ages of 50 and 69 years. In a series of 464 patients reviewed in the IRAD registry, mean age was 63 years. Two thirds of aortic dissections involve the ascending aorta (Stanford type A) and a third involve the descending aorta (Stanford type B). Typically, patients with type B dissection are older than those with type A dissection. Dissection in patients younger than 40 years typically is a type A dissection. According to the IRAD investigators, younger patients with acute aortic dissections are less likely to be hypertensive and are more likely to have Marfan syndrome, bicuspid aortic valve, some other connective tissue disorder, or prior aortic surgery. In all studies, there is a clear male predominance with an estimated male-to-female ratio ranging from 2 : 1 to 3 : 1. Although less frequently affected by acute aortic syndromes, women are older at the time of diagnosis with a mean age of 67 years and have worse outcomes, perhaps due to atypical symptoms and delay in diagnosis. Hirst and colleagues found a higher incidence of aortic dissection in African Americans, which might be related more to hypertension than to any intrinsic racial pathologic weakness of the aorta. Similarly, a high prevalence of hypertension may also explain why the incidence of aortic dissection and its variants is higher in Japan and other Asian countries.
The true incidence of aortic dissection is difficult to determine because many patients die without the correct diagnosis being made antemortem. It is not widely appreciated that acute aortic dissection is the most common clinical catastrophe involving the aorta. Moreover, its incidence has been increasing in the industrialized world, in part because of increasing life expectancy and more years exposed to elevated blood pressure. In a 1964 Danish study of 6480 autopsies covering 90% of a regional population, the incidence of acute aortic dissection was 5.2 per million population per year, higher than the incidence of ruptured abdominal aortic aneurysm (3.6 per million population per year) and more than four times the prevalence of ruptured thoracic aortic aneurysm (1.2 per million population per year). In the seminal 1958 pathologic series by Hirst and associates, acute aortic dissection was found in 1% to 2% of autopsies. In the 1970s, it was estimated that the incidence of acute aortic dissection in an urban population containing many African Americans in the southeastern United States might be as high as 10 to 20 cases per million population per year, or approximately 2000 to 4500 new cases each year. According to a review of all thoracic aortic diseases among the residents of Olmsted County, Minnesota, between 1980 and 1994, the annual incidence of acute aortic dissection was estimated at 3.5 per 100,000 person-years. More recently, in a comprehensive review of the entire Swedish national health-care registry during a 15-year period, it was observed that the incidence of thoracic aortic aneurysm and dissection had increased substantially between 1987 and 2002; specifically, the incidence of thoracic aortic disease rose by 52% in men and by 28% in women during this period to reach 16.3 cases per 100,000 per year and 9.1 cases per 100,000 per year, respectively. In general, these prevalence estimates undoubtedly underestimate the real incidence because they do not capture patients who die suddenly of a complication of aortic dissection and who are presumed to have succumbed to coronary disease or an arrhythmic event in the absence of a postmortem examination; importantly, this was not the case in the report from Sweden, where many dissections were identified only at the time of forensic autopsy, which is still performed almost universally in that country. Most physicians tend to think that ruptured abdominal aortic aneurysms are more common; this misconception comes from the fact that ruptured abdominal aortic aneurysm is diagnosed correctly more often than is acute aortic dissection.
According to the historical autopsy analyses, untreated acute aortic dissection is a highly lethal event. In the study by Shennan published in 1934, 40% of patients with dissection involving the ascending aorta died immediately, 70% within the first 24 hours, 94% within the first week, and 100% within 5 weeks. In 1967, Lindsay and Hurst reported that one third of patients sustaining an acute aortic dissection died within 24 hours, 50% within 48 hours, 80% within 7 days, and 95% within the first month. In patients with chronic dissection, only 15% were still alive after 5 years. In patients with dissection involving the descending thoracic aorta (Stanford type B), 25% had died 1 month after onset. Later, Anagnostopoulos and coworkers, in a large collected series of 963 cases of patients not surgically treated with aortic dissection of all types, reported a cumulative mortality of 70% at 1 week and 90% at 3 months, but as in other retrospective investigations the true patient denominator was unknown.
Most patients with untreated acute type A dissection die of intrapericardial rupture culminating in cardiac tamponade; other causes of death include acute aortic valvular regurgitation resulting in left ventricular failure, coronary ostial compromise causing acute myocardial ischemia, occlusion of aortic branches supplying the cerebral or visceral circulation, and free aortic rupture. Patients with untreated acute type B dissection usually die of aortic rupture or of distal end-organ malperfusion (occlusion of major aortic branches resulting in ischemic injury to vital abdominal organs, termed thoracoabdominal malperfusion). In the Stanford experience, lower extremity ischemia at presentation did not significantly increase surgical mortality risk, whereas occlusion of major abdominal tributaries resulting in renal or splanchnic ischemia was associated with very high mortality rates.
Only 10% of acute dissections are estimated to “heal” spontaneously, eventually becoming chronic dissections. Distal reentry sites are found in nearly all cases, allowing decompression of the false lumen. After acute aortic dissection, the false lumen usually remains patent but may thrombose rarely, depending mainly on the presence, size, and site of distal false lumen reentry sites. When the false lumen remains patent, it is prone to progressive expansion over time, resulting in the formation of a false aneurysm. It is noteworthy that a large fraction of acute serious or fatal dissection complications are caused by a non-reentering false lumen, which compromises distal blood flow by extrinsically narrowing or occluding the true lumen.
In patients with aortic dissection, the prevalence of hypertension varies between 45% and 80%, being highest in patients with acute type B dissection. Untreated hypertension promotes medial smooth muscle cell degeneration and other changes in the aortic wall, which may increase the susceptibility for aortic dissection. Although there is no evidence to suggest that hypertension initiates the actual process, it is a major risk factor.
Heritable connective tissue disorders such as Marfan, Ehlers-Danlos, and Loeys-Dietz syndromes are associated with an increased risk of aortic dissection. The Marfan syndrome is inherited as an autosomal dominant trait and is characterized by mutations of the FBN1 gene encoding the glycoprotein fibrillin 1, which is a major component of elastic fibers of the extracellular matrix in various organs. In addition to cardiovascular manifestations, including mitral valve prolapse, progressive aortic root dilation, aortic valve regurgitation, and aortic dissection, these patients can have several other ocular and musculoskeletal abnormalities. The diagnosis of Marfan syndrome is made according to the revised 2010 Ghent criteria (major and minor), which characterize the involvement of different organ systems, as well as genetic testing identifying a FBN1 mutation. When a patient demonstrates the classic Marfan syndrome phenotype, the diagnosis is rarely in doubt; however, many patients have only some of the characteristic phenotypic features (variable penetrance), including aortic root dilation with or without aortic valve regurgitation, which has been called the forme fruste of Marfan syndrome. Aortic-related complications, including acute dissection and rupture, are the leading causes of death in patients with Marfan syndrome. If a patient with Marfan syndrome has a family history of aortic dissection or other aortic catastrophe at an early age, the risk of dissection or rupture is considerably higher. The prevalence of Marfan syndrome in patients presenting with acute aortic dissection ranges between 5% and 12%.
Patients with Ehlers-Danlos syndrome, particularly those with type IV (vascular type) Ehlers-Danlos syndrome, which is transmitted in most cases as an autosomal dominant trait, have arterial weakness of all large and muscular arteries; type IV Ehlers-Danlos syndrome is characterized by a procollagen type 3 (COL3A1) abnormality and an increased risk of aortic dissection or spontaneous rupture of peripheral arteries or a hollow abdominal viscus. Aortic rupture has also been reported in patients with Ehlers-Danlos syndrome type I and type VI. Extremely fragile arteries are found in patients with Ehlers-Danlos syndrome, and vascular procedures, including simple arterial puncture and suture repair, can be fraught with devastating complications. The diagnosis of (vascular type) Ehlers-Danlos syndrome is based on genetic testing identifying a mutation in the gene COL3A1 coding for type III procollagen.
Loeys-Dietz syndrome is a more recently recognized autosomal dominant connective tissue disorder characterized by premature arterial aneurysms (typically aortic root aneurysm) and aortic dissection along with diffuse peripheral arterial tortuosity. It is caused by heterogeneous mutations in the genes encoding transforming growth factor β receptors 1 and 2 (TGFBR1 and TGFBR2), and the diagnosis is confirmed through identification of these mutations. Phenotypic features of Loeys-Dietz syndrome include hypertelorism, bifid uvula or cleft palate or both, hyperlucent skin, and generalized arterial hypertortuosity, especially of the extracranial carotid or iliac arteries. In these patients, the risk of aortic rupture and aortic dissection exceeds that of any other known connective tissue disorders. In addition, aortic rupture and dissection occur at a younger age (even in infants) and at small (almost normal) aortic diameters.
More recently, a genetic basis of nonsyndromic familial thoracic aortic aneurysms and dissection has been defined involving multiple defective genes. Specifically, several gene mutations have been identified causing various defects in cell signaling pathways (TGFBR2 mutations different than in Loeys-Dietz syndrome) and protein synthesis of components in the contractile apparatus of vascular smooth muscle cells (MYH11 and ACTA2 mutations), resulting in thoracic aortic aneurysms and aortic dissection occurring at aortic diameter less than 5 cm.
Congenital heart problems, such as bicuspid aortic valve and coarctation of the aorta, are associated with an increased risk of aortic dissection compared with that in the general population. In an analysis of 186 autopsies of patients who died of type A aortic dissection, it was found that the prevalence of unicuspid or bicuspid aortic valves was 9%. The risk of perioperative and late postoperative dissection is also increased in patients with a bicuspid aortic valve after any type of cardiac surgery, especially in patients with dilation of the ascending aorta. Aortic dissection predominantly involves the ascending aorta in patients with coarctation and the transverse arch is relatively hypoplastic, and the dissection may not propagate beyond the aortic isthmus. Simultaneous management of an acute type A aortic dissection in patients with uncorrected severe coarctation is challenging and may require modification of the CPB arterial cannulation strategy and occasionally the use of an extra-anatomic thoracic aortic graft to bypass the coarctation.
Aortic dissection is a rare complication of cardiac catheterization and other percutaneous diagnostic and therapeutic interventional techniques involving manipulation of catheters inside the thoracic aorta. Catheter and guidewire injuries are usually self-limited, localized subintimal dissections that only rarely require surgical intervention. On the other hand, life-threatening iatrogenic dissections can occur during endovascular device deployment (TEVAR or transfemoral percutaneous aortic valve replacement) or open surgical procedures; among 7000 cardiac operations, iatrogenic aortic dissection complicated 0.3% of cases. These can be due to ascending aortic cannulation, retrograde dissection after femoral artery cannulation, aortic cross-clamp or partial occluding clamp injury, and intimal injury at the site of a proximal bypass graft anastomosis. The incidence of iatrogenic perioperative type A aortic dissection is higher in patients undergoing off-pump coronary artery bypass grafting, which was attributed to multiple ascending aortic manipulations for construction of the proximal anastomoses.
In women younger than 40 years, approximately 50% of dissections occur during the third trimester or during labor and delivery; a substantial proportion of these women have connective tissue disorders, such as Marfan syndrome, or a bicuspid aortic valve associated with a dilated tubular segment of the ascending aorta. The hemodynamic and hormonal alterations of pregnancy, culminating in the third trimester, are thought to be the causes of dissection in susceptible individuals.
One of the cardiovascular complications of cocaine use, particularly crack cocaine inhalation, is acute aortic dissection. Aortic dissection in this setting occurs presumably as a consequence of abrupt, severe hypertension and catecholamine release, and this diagnosis should be considered in cocaine or methamphetamine abusers presenting with chest pain.
Aortic dissections also occur more frequently than in the general population in patients with autosomal dominant polycystic kidney disease, Turner syndrome, Noonan syndrome, and Alagille syndrome. Inflammatory diseases such as Takayasu arteritis, giant cell arteritis, Behçet disease, autoimmune disorders such as systemic lupus erythematous, and infection of the aorta, such as syphilis, have been rarely associated with acute aortic dissection.
In 1929, Erdheim was the first to describe what he called “cystic medial necrosis,” a nonspecific pathologic process involving medial smooth muscle cell loss, elastic lamellar disruption, and acid mucopolysaccharide accumulation within the aortic media. This abnormal architecture is believed to lead to changes in the distribution of both circumferential wall stress and shear stress in the aortic media, potentially leading to an intimal tear. The word cystic is actually a misnomer, because these medial lesions do not form true cysts (they are not lined by epithelial cells). The term necrosis is also incorrect because it is singularly absent. In young patients (particularly those with a heritable connective tissue disorder), the elastic elements of the aortic media are disrupted and disorganized; in older individuals, it is the smooth muscle elements of the aortic media that are abnormal because of aging and hypertension, and probably represent changes associated with repeated aortic wall injury and repair. Thus, the well-known moniker “cystic medial necrosis” should be abandoned and replaced by more specific terms relating to alterations of the elastic fibers (“elastic type”) and smooth muscle cells (“smooth muscle type”) in the media in younger and older patients, respectively. In patients with inherited connective tissue disorders, such as Marfan syndrome, pathologic examination of the aortic wall frequently revealed pronounced medial degeneration, with severe loss of elastic lamellae and accumulation of mucoid substance within the media. These young patients typically have an acute type A dissection. On the other hand, in older individuals, type B dissections are more common and are associated with medial degeneration characterized by loss of smooth muscle cells. It was proposed that the coexistence of activated T lymphocytes and macrophages and markers of apoptotic vascular cell death in the aortic media of patients with aortic dissection may contribute to the two pathways leading to medial degeneration, namely, loss of vascular smooth muscle cells and degradation of the extracellular matrix. Increased contents of collagen types I and III as well as increased activity of connective tissue growth factor have been observed in the media and adventitia of patients with aortic dissection ; these phenomena are likely to be responsible for the reduced aortic distensibility and compliance. Another contributing factor to progressive degradation of the extracellular matrix is excessive activation of matrix metalloproteinases, particularly matrix metalloproteinase 9, which are zinc-dependent proteolytic enzymes that can disrupt the balance composition of vascular smooth muscle cells and extracellular matrix proteins. Specific nucleotide polymorphism of the gene encoding matrix metalloproteinase 9, more specifically, the presence of the −8202A/G allele, seems to be associated with an increased risk of aortic dissection.
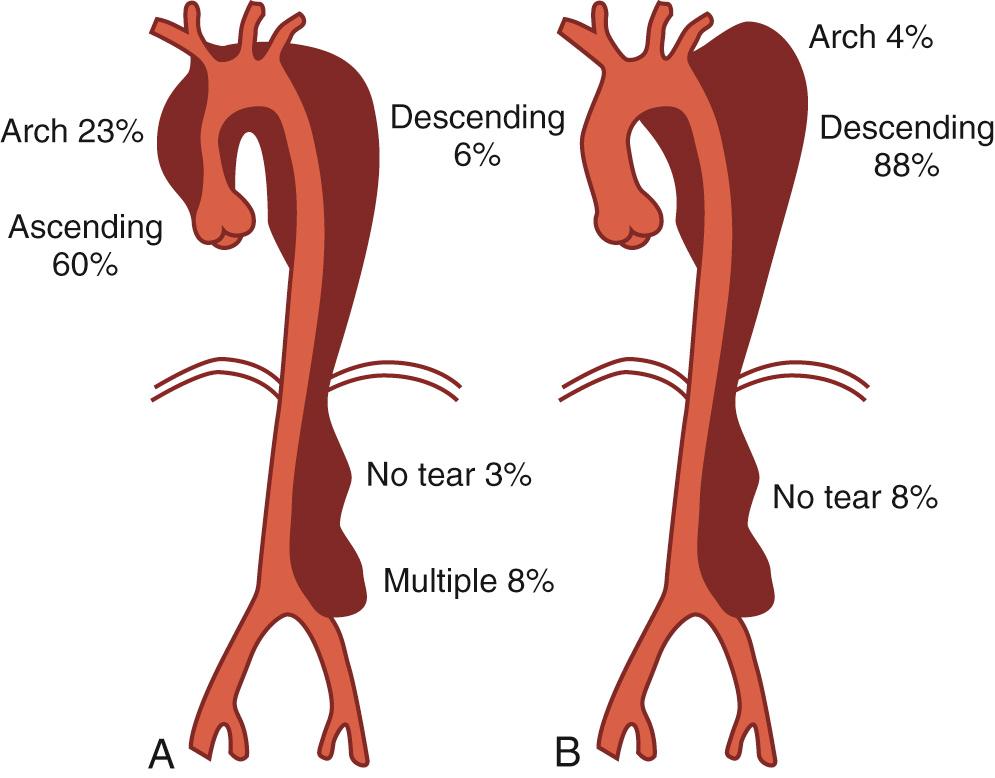
Most authorities believe that the initiating event in aortic dissection is a tear in the intima allowing blood to enter the aortic wall that culminates in progressive separation of the medial layers of the aorta (elastic and circumferential smooth muscle fibers) with propagation of the dissecting hematoma. The primary intimal tear allows communication between the true aortic lumen and the false lumen. Only 2% to 4% of aortic dissections do not have an identifiable primary intimal tear and are usually confined to the descending thoracic aorta. Rarely in patients with connective tissue disorders, a localized intimal disruption can be present without extensive undermining of the intima, pseudoaneurysm development, or any false lumen, what we colloquially call “intimal stretch marks.” If they are associated with a localized hematoma within the wall, they have a “mushroom cap” appearance. Whether an intimal tear is the precipitating event in all aortic dissections is still debated. IMH owing to rupture of the vasa vasorum is another potential but infrequent initiating event leading to frank dissection. Rupture of the intima usually happens at points of maximal wall stress along the thoracic aorta. Intimal tears are usually transverse in orientation and typically involve one half to two thirds of the aortic circumference. Infrequently, total disruption of intimal continuity with a complete circumferential tear can lead to intimo-intimal intussusception and mechanical obstruction of blood flow because of gross prolapse of the circumferential intima. In type A dissections, the majority of intimal tears (60% to 70%) are located in the ascending aorta, usually just distal to the sinotubular junction ( Fig. 70-3 ). In 10% to 20%, the intimal tear is located in the aortic arch, most commonly on the lesser curvature. The intimal tear can also originate in the proximal one third of the descending aorta, near the aortic isthmus (“retro-A dissection”). In less than 5% of cases, the intimal tear can be located in the abdominal aorta, and the dissection will either be confined to the abdominal aorta or propagate in a retrograde fashion to involve the ascending thoracic aorta.
Within the aortic wall, the false lumen is situated between the inner two thirds and the outer one third of the aortic media. On pathoanatomic examination, the dissected aorta is a false aneurysm, because the aortic intima containing the true lumen is not dilated and actually is smaller than normal. Once initiated, aortic dissections usually propagate antegrade or “downstream” but may also extend in a retrograde direction. The dissection often proceeds in a spiral fashion down along the aorta. Propagation of the dissection depends on several factors, including rate of increase of aortic systolic pressure (or aortic dP/dt), magnitude of aortic diastolic elastic recoil and stiffness, mean and peak arterial pressure, and aortic wall integrity and strength. The mainstay of medical treatment of aortic dissection, as described by Wheat and Palmer in 1965, is directed at reducing aortic dP/dt, called anti-impulse therapy . In the ascending aorta, the false lumen usually occupies the right anterior portion; in the arch, the false lumen usually is located along the greater curvature and may extend into the innominate, left carotid, or left subclavian arteries. In the descending and abdominal aorta, the false lumen often runs along the anterior and lateral aortic walls, frequently incorporating the take-off of the left renal artery. Distal progression of the dissection may be limited by extensive atherosclerosis or anatomic constraints such as aortic coarctation, infrarenal abdominal aortic aneurysm, or abdominal aortic graft anastomosis. Otherwise, in young individuals the dissection almost always involves the entire thoracic and abdominal aorta and extends into the iliac arteries. Limited Stanford type A, DeBakey type II dissections are rare in our experience. In patients surviving the acute episode, the false lumen usually remains patent but rarely may thrombose spontaneously. The presence of distal reentry sites or fenestrations contributes to persistent patency of the false lumen. Partial or complete thrombosis of the false lumen may allow “healing” of the aorta; conversely, if the false lumen reenters distally and stays patent, it is prone to progressive false aneurysmal enlargement. A patent distal false lumen is observed in up to 90% of patients after surgical repair of acute type A dissections and may portend an adverse prognosis associated with a higher incidence of late “downstream” false aneurysmal degeneration. Reentry sites are usually multiple and frequently occur at the ostia of sheared off branches, such as the intercostal, visceral, renal, or iliac arteries. Reentry into the true lumen, described by Peacock in 1843 as “an imperfect natural cure of the disease,” allows decompression of the false lumen and is the rationale behind surgical and percutaneous flap fenestration techniques.
In 1920, Krukenberg first described aortic IMH as a “dissection without intimal tear.” IMH is believed to originate from rupture of the vasa vasorum within the outer third of the media, resulting in the circumferential accumulation of blood ( Fig. 70-4 ), with no apparent intimal defect visualized on imaging studies. IMH can occur spontaneously in predisposed individuals (e.g., older and hypertensive patients) or be a secondary phenomenon after the rupture of an atheromatous plaque through the internal elastic lamina and the formation of a penetrating atherosclerotic ulcer allowing extravasation of blood into the aortic wall (see Fig. 70-4 ). The natural history of these lesions was not well characterized until the last two decades. The evolution of IMH may either be benign, with a stable clinical course and eventual healing, or a progressive, often fatal disease, with extension, evolution into classic aortic dissection, aneurysmal degeneration, or aortic rupture. In recent years, it was recognized that IMH involving the ascending (type A IMH) or descending (type B IMH) aorta can occasionally portend a different clinical course from that of classic aortic dissection, especially if it is detected incidentally in asymptomatic patients undergoing cross-sectional imaging. Conversely, patients with acute severe chest pain are more prone to disease progression and aortic rupture, similar to those with full-blown acute dissections, especially in the presence of an associated deep penetrating ulcer. We believe that IMH of the ascending aorta usually has a malignant prognosis almost identical to that of acute type A aortic dissection, and these patients should be treated accordingly.
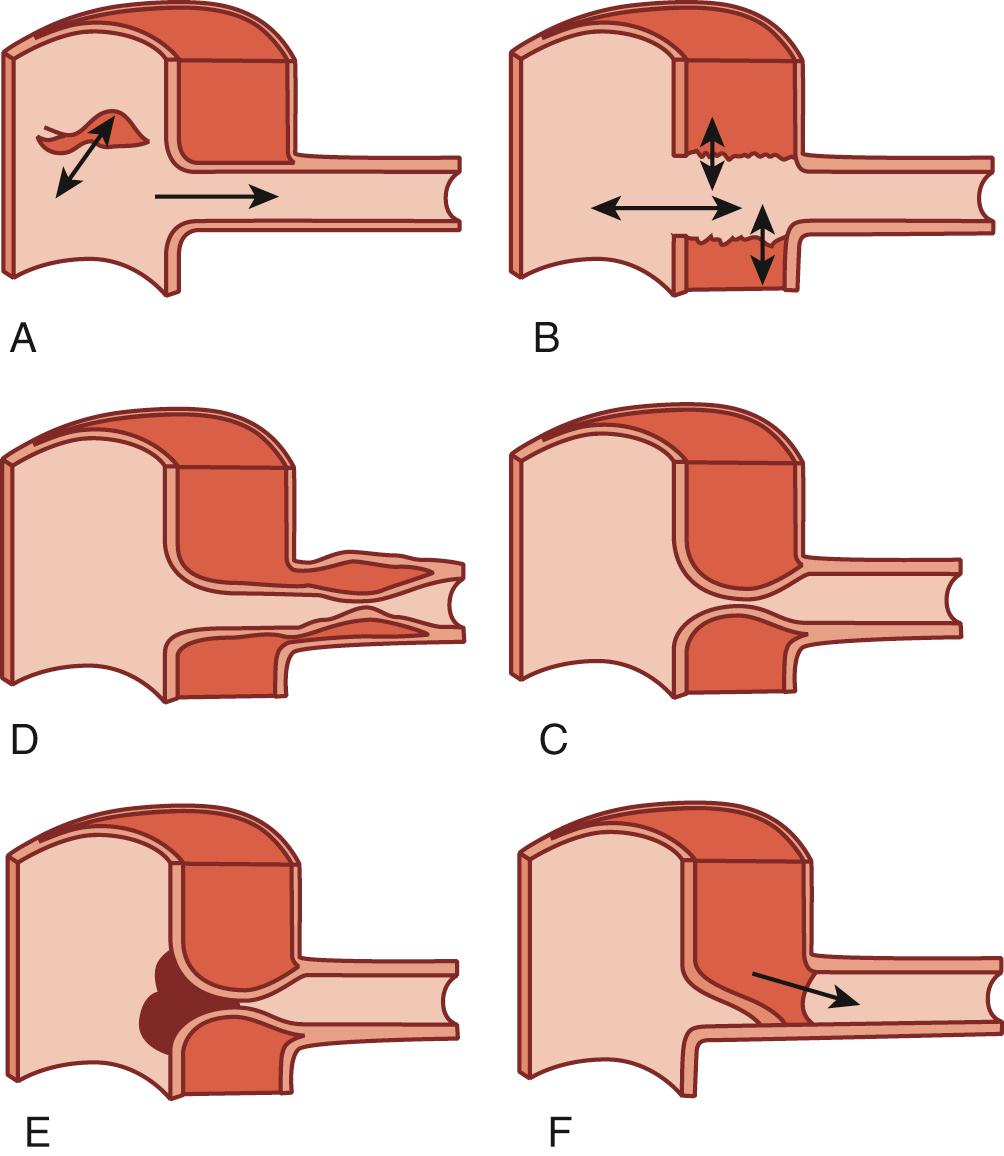
Peripheral branch vessel ischemia or malperfusion arises when the dissection process compromises blood flow to various aortic tributaries through several mechanisms, including extrinsic compression of the true lumen by the pressurized false lumen (particularly a false lumen that does not reenter), an intimal flap compromising the orifice of the branch artery ( Fig. 70-5 ), and occlusion of the tributary if the dissection continues into the branch because of false lumen extrinsic compression of the true lumen distally. A useful pathophysiologic classification of aortic branch compromise was proposed by Williams and associates : static obstruction occurs when the dissection flap extends into a branch vessel, resulting in mechanical compromise of flow; dynamic obstruction occurs when the dissection flap narrows the aortic true lumen above the branch because of a large false lumen or when the flap prolapses into the vessel origin. As the dissection progresses in a spiral fashion along the aorta, some aortic branches may be spared and continue to be perfused by the true lumen, whereas other arteries may be perfused exclusively from the false lumen after being sheared off; in this latter scenario, the affected branch subsequently becomes permanently dependent on the false lumen for perfusion. In some cases, compression by the false lumen may almost eliminate the entire aortic true channel (true lumen collapse or true lumen obliteration) with resultant severe distal thoracoabdominal malperfusion. The pattern of branch artery involvement and the degree of perfusion compromise determine the clinical presentation, which is enormously variable and often leads to delay before the correct diagnosis is established. Indeed, acute aortic dissection has been called “The Great Masquerader” because the symptoms can mimic those of many other acute illnesses. In the large autopsy series by Hirst and colleagues, the most commonly affected aortic branches were the iliac arteries, followed (in descending order) by the innominate, left common carotid, left subclavian, coronary, renal, superior mesenteric, and celiac axis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here