Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Many postoperative patients will have drainage devices to facilitate their care. The types used most often fall into the following broad categories:
Chest tubes
Urinary drainage tubes (urinary catheters)
Gastrointestinal (GI) tubes (nasogastric [NG], feeding tubes, and gastrostomy and jejunostomy tubes)
Biliary drainage tubes (T-tubes, internal-external biliary drain)
Wound drainage tubes (Jackson-Pratt, Penrose, and other suction drains)
Problems with these tubes are frequent but generally straightforward. This section is organized by the type of tube. Intravenous (IV) lines are covered in Chapter 19 .
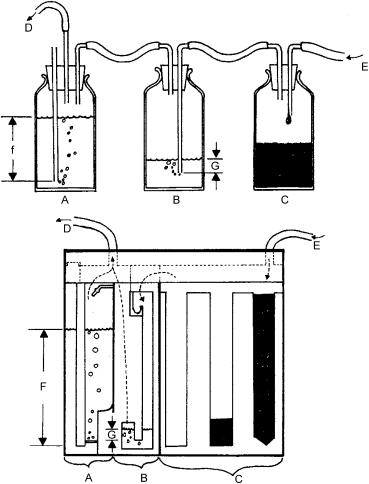
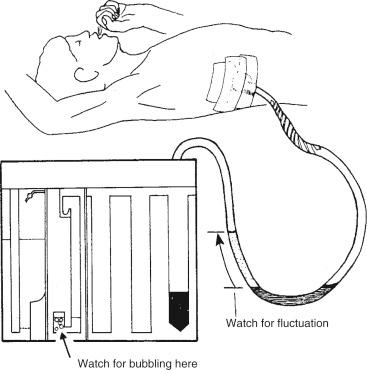
Appropriate treatment of the problems associated with chest tubes begins with a fundamental knowledge of how the tubes work. The apparatus is a means to apply external suction to the pleural cavity to rid the space of unwanted air or fluid. The collection apparatus looks complicated but may be easily understood if the components are considered separately; the apparatus may be thought of as three separate interconnected bottles ( Fig. 31.1 ), as follows:
Suction from the wall or from a vacuum device is connected to the suction control container (see Fig. 31.1A ). The volume of water in this container (F) dictates the amount of suction that is transmitted to the patient. When suction is ordered, it is ordered in units of centimeters of water (cm H 2 O), and additional suction pressure results in entraining air from the open tube, as indicated by bubbling in this chamber.
The suction control bottle (A) is connected to the underwater seal container ( B ). This container allows separation of the patient from the suction if desired, and is the site of indication of an air leak. Continued air evacuation is noted as persistent bubbling in this chamber.
The underwater seal container (B) is connected to the collection container ( C ), which is the site of fluid collection. Fluid draining from the chest tube is stored in this chamber for measurement and testing, if desired. The collection container (C) is then connected to the chest tube in the patient (E). These containers may be combined into a single box-type drainage apparatus (Pleur-Evac).
Some Pleur-Evacs are designed to allow retransfusion of drained blood, a helpful situation in trauma cases.
Percutaneous drainage of the pleural cavity may be diagnostic and therapeutic. In the setting of dyspnea and hypoxia, the need for a chest tube may be an emergent event. In the stable patient, take the extra time is necessary to adequately prepare and sedate the patient. Consider use of pigtail chest tube for pneumothorax or simple effusion.
Pneumothorax
Pyothorax
Hemothorax
Chylothorax
Persistent pleural effusion
Postoperative application after thoracic procedures
Coagulopathy
Abnormalities in platelet count or function or in clotting-factor concentrations should be corrected before insertion of the tube.
Skin infection over the site of needle insertion may carry infection into the pleural cavity.
Try to choose an uninvolved site.
Skin preparation supplies (iodine, chlorhexidine)
Local anesthetic (1% or 2% lidocaine, 0.5% Marcaine, small-gauge needle, 10-mL syringe).
Sterile gloves, eye protection, gown
Sterile towels or drapes (if not included in tube thoracostomy kit)
Sedative medication, as necessary
Continuous pulse oximetry
Chest tube of the appropriate diameter: small (16–24 Fr) for air removal and large (32–38 Fr) for fluid/blood removal. The perforated end may be cut down to facilitate a smaller patient. Placing a bevel on the end is not recommended; it may facilitate placement, but it is a perforation risk once inside the patient. If unknown whether to expect air or fluid, recommend placement of a larger French tube.
A chest tube insertion tray that includes blades, gauze, hemostats, surgical scissors, clamps, thick silk suture with needle, and drapes
Petroleum gauze
Wide, gas-impermeable, occlusive tape
Suction device or wall suction
Chest tube suction apparatus (Pleur-Evac), pre-filled with water, as necessary, and hooked to the suction device
The size and placement of the tube depend on the indication. A larger tube (32–38 Fr) and posterior placement are indicated for drainage of fluid; a smaller tube (20–24 Fr) and anterior placement is adequate for the drainage of air. The most versatile approach is laterally at the fifth to sixth interspace midanterior axillary line, about the level of the nipples or termination of the axillary hairline. From this site, the tube may be directed either anteriorly or posteriorly.
Local, with optional IV sedation and narcotic pain medicine. Conscious sedation can be considered for elective tube placement (see Chapter 4 ).
Effective local anesthetic use makes placement of a chest tube less stressful for both the patient and you. Be sure to properly anesthetize the skin, subcutaneous (SC) tissues, rib, and pleura. The deep structures are the most uncomfortable and care should be used to ensure adequate delivery of local anesthetic around the rib and pleura.
Elective chest tube placement in a relatively stable patient may be done in a controlled and safe manner using adequate premedication of the patient with sedatives and local anesthesia. This technique describes a hemostat technique; some prefer a trochar-assisted placement; however, we do not endorse that technique because of increased chance of causing an injury. In an unstable patient, defer to the most experienced hands, do not take the time necessary to premedicate, and move as quickly and safely as possible.
Prepare the patient.
Explain the procedure.
Explain the risks and alternatives.
Answer any questions.
Have a consent form prepared and signed.
Position of the patient.
Supine with the arm on the affected side extended upward
Premedicate the patient.
Short-acting benzodiazepine such as lorazepam (Ativan) 1 to 5 mg IV.
Short-acting narcotic such as fentanyl (Sublimaze) 25 to 50 mcg IV also may be necessary.
Skip all premedication (both benzodiazepine and narcotic) if the patient is dyspneic or is at risk for respiratory depression.
Prepare the skin.
Use sterile technique and sterile gloves, mask, and gown.
Plan the incision.
The mid-anterior axillary line is generally used, with anterior direction of the chest tube to remove gas and posterior direction of the chest tube to remove fluid. Find the fifth rib interspace, take care to locate the correct level to increase the safety of this procedure. Plan to make the skin incision about 1 to 2 cm below the rib interspace to be entered so that there is an oblique skin channel. This usually facilitates skin closure on removal of the tube. On occasion, the anterior midclavicular line is used to treat uncomplicated pneumothorax, generally with a pigtail tube.
Sterilely prep and drape the skin.
Infiltrate with 1% to 2% lidocaine into the skin at the entry site, around the rib at the selected interspace, and adjacent to the pleura. We recommend advancing the needle while drawing back until bubbles or fluid is encountered. Withdraw the needle slightly and deliver a bolus of anesthetic in this area. Ideally, this will anesthetize the pleura, a very painful area.
The periosteum of the top of the rib is very sensitive; do not skimp on lidocaine. Additionally, the parietal pleura is sensate and requires local anesthesia. Infiltrate the SC tunnel as well while removing the needle.
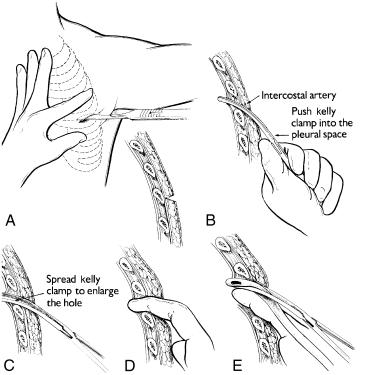
Make the skin incision over a rib.
Confirm adequate anesthesia. Cutting over the bone allows a clean, deep cut and avoids the neurovascular bundle that travels the underside of each rib. The incision should be about 1.5 times the diameter of the chest tube. Control any bleeding with pressure. Reinject with lidocaine, as necessary (see Fig. 31.2A ).
You can place a purse-string suture at the skin entry site.
Position the tie such that the loose ends are positioned inferiorly to the tube exit site, and place a single throw loosely.
Bluntly dissect toward the pleura (see Fig. 31.2B ).
Using a hemostat, create a SC channel superiorly from the skin incision to over the top of the rib at the desired interspace.
Using a fair amount of pressure, and with the hemostats closed, force the hemostats between the ribs through the intercostal muscles. Stay right on top of a rib to avoid the neurovascular bundle.
You will notice a “pop” when the pleural cavity has been entered. There also may be a noticeable gush of air or fluid through the wound.
Spread the hemostat tips to create sufficient space in the intercostal muscles to allow the tube to pass (see Fig. 31.2C ).
Remove the hemostat and insert a finger to confirm penetration into the pleural cavity and that there is no loculated lung attached to the adjacent chest wall. Be careful to avoid the sharp edges of broken ribs in the setting of trauma. (see Fig. 31.2D ).
Insert the chest tube (see Fig. 31.2E ).
Using the hemostat, grasp the perforated end of the chest tube and place it through the SC channel and the intercostal muscle opening. This often is a difficult maneuver; it may take several passes to find the channel you created. (With trochar insertion, the tube is placed over the trochar and forced into the pleural cavity without hemostat perforation of the intercostal muscles.)
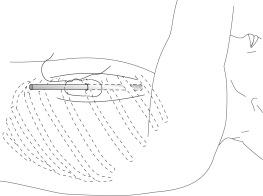
Position the chest tube.
Note that the chest tube has a mark just beyond the last perforations. When the tube has been placed into the chest and directed in the appropriate direction, insert it to the desired length. Make sure the mark is either inside the chest wall or just visible at the skin incision line, or the tube will leak.
Secure the tube.
Pull the purse-string suture snugly around the tube without adding throws. Wrap the loose ends around the tube several times to hold it in place. Make sure that several inches of suture are wrapped around the tube because this will be used to close the wound when the tube is removed. Once wrapped, the loose ends may be tied down securely ( Fig. 31.3 ). Place additional sutures, as necessary, to close the skin incision. Wrap the long ends of each suture around the chest tube and tie securely.
Connect the chest tube to the Pleur-Evac and to wall suction.
The suction pressure is defined by the volume of water (in cm of H 2 O) in the suction control chamber of the Pleur-Evac. Bubbling in the underwater seal chamber will indicate adequate suction to remove gas and will continue for as long as there is an air leak. If fluid is to be removed, it will collect in the collection chamber ( Fig. 31.1C ).
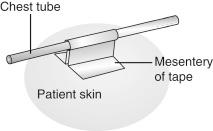
Tape the chest tube site.
Wrap the tubing at the skin site with petroleum gauze.
Apply occlusive tape in such a way that the tube site is relatively airtight and the tube is safe from being dislodged.
Further secure the tube by applying a “mesentery” tape such that unexpected pulls on the tube will pull on the mesentery instead of on the suture ( Fig. 31.4 ).
Confirm tube placement by stat bedside upright AP chest x-ray (CXR).
Reposition as necessary. Daily CXRs are recommended to follow the course of therapy and to confirm continued adequate placement of the tube. A lateral CXR may be helpful to find the exact location of the tube.
The most proximal hole in the chest tube interrupts the radiopaque band on the tube, so it is easy to determine on CXR whether the tube is adequately placed. This most proximal hole should be well within the pleural space.
Control the patient’s pain.
The tube insertion site will remain uncomfortable until the tube is removed, so make sure the patient has adequate pain relief.
Pulmonary toilet is important in a patient with a chest tube.
Make an incentive spirometer available, and instruct the patient as to its use and importance.
Send fluid efflux from the chest tube to the laboratory.
The following studies may be indicated:
Gram stain
Cultures (aerobic and anaerobic bacterial, fungal, mycoplasma)
TB culture and acid-fast bacilli
Cell count and differential
Lactate dehydrogenase (LDH)
Protein
Glucose
Cytology for malignant cells
Other studies as appropriate (amylase, triglycerides, pH, rheumatoid factor, antinuclear antibodies or complement levels, etc.). Blood for simultaneous tests for serum LDH, protein, glucose, and so on should be drawn to compare with the results of the pleural fluid.
Document the procedure.
Lack of resolution of the problem
Occasionally, more than one chest tube will be needed.
Perforation of the lung
This is more likely with a trochar placement.
Perforation of abdominal viscera
This may happen if the skin entry site is too far caudal on the chest wall.
Perforation of the heart
Persistent air leak
Check the tubing between the drainage apparatus and the patient for loose connections.
Untape the wound site and confirm that the chest tube is inserted properly.
Check whether the chest tube is fully inserted and the line is at or inside the skin line.
If the entry site is not well closed, or a “sucking” sound is noted at the site, it may be necessary to further close the site with 2-0 silk sutures. Be sure to adequately prep and anesthetize the area before repair.
Reposition the chest tube if necessary, and redress the site using petroleum gauze.
If the connections are intact and the site is dressed in an airtight manner, order a portable AP CXR to assess the patient’s lungs and the tube position.
If the CXR shows lack of resolution of pneumothorax, consider placement of a second tube.
Persistent fluid efflux
Bleeding at the entry site
Discomfort
A pigtail catheter is a small malleable catheter designed to spiral (pigtail) within the chest to stay in place. These catheters are simple to place (if done correctly) and allow for a less invasive method for draining simple fluid or air. The tube is too small and prone to blockage to drain blood or thicker fluid.
The technique is similar to placement of a central line in that Seldinger technique is used. The tube can be placed in the lateral chest similar to placement of a classic tube thoracostomy. This is desirable for drainage of simple fluid. Alternatively, the tube can be placed in the anterior chest in the mid-clavicular line approximately at rib interspace three to relieve a pneumothorax.
Prepare the patient.
Explain the procedure.
Explain the risks and alternatives.
Answer any questions.
Have a consent form prepared and signed.
Position of the patient.
Place the patient supine with the arm on the affected side extended upward.
Prepare the skin.
Use sterile technique and sterile gloves, mask, and gown.
Plan the point of entry.
The mid-anterior axillary line can be used, with anterior direction of the tube to remove gas and posterior direction of the chest tube to remove fluid. Find the fifth rib interspace, take care to locate the correct level to increase the safety of this procedure. Plan to enter with the needle directly over the rib. On occasion, the anterior midclavicular line is used to treat uncomplicated pneumothorax, enter two finger-breadths below the clavicle.
Sterilely prep and drape the skin.
Infiltrate with 1% to 2% lidocaine into the skin at the entry site, around the rib at the selected interspace, and adjacent to the pleura. We recommend advancing the needle while drawing back until bubbles or fluid is encountered. Withdraw the needle slightly and deliver a bolus of anesthetic in this area. Ideally, this will anesthetize the pleura, a very painful area.
The periosteum of the top of the rib is very sensitive; do not skimp on lidocaine. Additionally, the parietal pleura is sensate and requires local anesthesia. Infiltrate the SC tunnel as well while removing the needle.
Register the trajectory of the needle used for anesthetizing the skin to aid in the direction of your next steps.
Connect the larger-gauge finder needle to a syringe filled partially with sterile saline. Aim this needle directly over the rib and advance until you reach the bone. Adjust your angle slightly and walk the needle superiorly until you enter the pleural space.
Remove the syringe and advance the guidewire into the pleural space. Take care not to push against any resistance as this may indicate you are in the wrong space (SC, liver, lung, etc.). Once the guidewire smoothly enters the chest, you can remove the needle using Seldinger technique.
Advance the chest tube catheter of the guidewire and into the chest. Maintain proper Seldinger technique and do not let go of the wire. We recommend pinching the catheter near its entry at the skin and pushing and twisting in small increments until the catheter is nearly hubbed. Take care not the kink the catheter or the guidewire as it passes over the rib.
Remove the guidewire. Connect the catheter to the drainage container. Typically, an adapter is require to connect to the Pleur-Evac. Multiple adapters are likely to be included in the pigtail catheter kit.
Secure the catheter using suture. Ensure that it is secure but that your suture ties do not occlude the catheter. Apply a dressing and tape to further secure the catheter and tubing in place.
Confirm tube placement by stat bedside upright AP CXR.
Reposition as necessary. Daily CXRs are recommended to follow the course of therapy and to confirm continued adequate placement of the tube. A lateral CXR may be helpful to find the exact location of the tube.
Control the patient’s pain.
The tube insertion site will remain uncomfortable until the tube is removed, so make sure the patient has adequate pain relief.
Pulmonary toilet is important in a patient with a chest tube.
Make an incentive spirometer available, and instruct the patient as to its use and importance.
Consider sending fluid efflux from the chest tube to the laboratory.
The following studies may be indicated:
Gram stain
Cultures (aerobic and anaerobic bacterial, fungal, mycoplasma)
TB culture and acid-fast bacilli (AFB)
Cell count and differential
LDH
Protein
Glucose
Cytology for malignant cells
Other studies as appropriate (amylase, triglycerides, pH, rheumatoid factor, antinuclear antibodies or complement levels, etc.). Blood for simultaneous tests for serum LDH, protein, glucose, and so on should be drawn to compare with the results of the pleural fluid.
Document the procedure.
Lack of resolution of the problem
Occasionally, more than one chest tube will be needed.
Perforation of the lung
Perforation of abdominal viscera
This may happen if the skin entry site is too far caudal on the chest wall.
Perforation of the heart. Do not ever force a guidewire.
Persistent air leak
Check the tubing between the drainage apparatus and the patient for loose connections.
Untape the wound site and confirm that the chest tube is inserted properly.
Check whether the chest tube is fully inserted and the line is at or inside the skin line.
If the entry site is not well closed, or a “sucking” sound is noted at the site, it may be necessary to further close the site with 2-0 silk sutures. Be sure to adequately prep and anesthetize the area before repair.
Reposition the chest tube if necessary, and redress the site using petroleum gauze.
If the connections are intact and the site is dressed in an airtight manner, order a portable AP CXR to assess the patient’s lungs and the tube position.
If the CXR shows lack of resolution of pneumothorax, consider placement of a second tube.
Persistent fluid efflux
Bleeding at the entry site
Discomfort
In settings of persistent pneumothorax or malignant effusion, it may be necessary to perform pleurodesis. This entails infusion of an irritant into the pleural space to create scarring between the visceral pleura and the parietal pleura. On removal of the tube, the lung will remain scarred to the chest wall. This may not be a procedure typically performed by the general surgery team. Consider thoracic surgery consultation prior to removal of the tube.
Persistent malignant effusion
Persistent pneumothorax
Hypersensitivity to lidocaine or other sclerosing agents.
Tube preparation supplies (iodine, chlorhexidine, or alcohol)
Sterile gloves, eye protection
Sedative medication, as necessary
Pulse oximeter
Two 60-mL syringes with 18-gauge needles attached
Two tubing clamps
Chest tube drainage system hooked to wall suction
Sclerosing agent (exact agent per individual institutional norm).
Premedication of the patient with both a narcotic and an anxiolytic medication.
Prepare the patient.
Explain the procedure.
Explain the risks and alternatives.
Answer any questions.
Obtain informed consent, if necessary.
Place the patient on continuous pulse oximetry.
Position of the patient.
Supine
Premedicate the patient.
Short-acting benzodiazepine such as midazolam (Versed) 1 to 5 mg IV or lorazepam (Ativan) 1 to 5 mg IV.
Short-acting narcotic medication, such as fentanyl 25 to 50 mcg IV, also may be necessary.
Prepare the tube.
Clamp the chest tube on the soft rubber portion close to the patient.
Sterilely prepare a portion of the rubber tubing proximal to the clamp.
Inject the desired medication into the tube.
Elevate the tube so that the entire volume enters the chest cavity.
Place a second clamp on the tube on the plastic portion just at the chest wall.
Position the patient as follows to distribute the lidocaine:
2 minutes supine Trendelenburg
2 minutes supine reverse Trendelenburg
2 minutes right lateral decubitus
2 minutes left lateral decubitus
2 minutes prone (optional)
Unclamp the tube at the site closest to the patient and inject the sclerosing agent into the tube.
Elevate the tube so that the entire volume enters the chest cavity.
Reclamp the tube on the plastic portion just at the chest wall.
Position the patient as follows to distribute the sclerosing agent:
15 minutes supine Trendelenburg
15 minutes supine reverse Trendelenburg
15 minutes right lateral decubitus
15 minutes left lateral decubitus
15 minutes prone (optional)
Unclamp the tube and allow the sclerosing agent to drain out.
Reconnect the chest tube to suction for 24 to 48 hours or until there is no persistent air leak.
Document the procedure.
If the patient becomes dyspneic or hypoxic at any time during the procedure, unclamp the chest tube and return it to suction.
Incomplete pleurodesis is common. If there are persistent symptoms, repeat application of pleurodesis or a surgical decortication may be necessary.
Successful pleurodesis requires the development of inflammation in the pleura. Do not administer antiinflammatory medication, but be prepared to treat discomfort with a mild narcotic.
This is best done with an assistant.
Confirm that the patient is ready to have the chest tube removed.
There should be no persistent air leak, or the patient should have been stable for at least 24 hours on water seal alone.
Ongoing fluid leak or bleeding should have stopped.
The lung should be inflated on CXR.
There is no other reason to consider leaving the tube in place.
Have all equipment ready.
Blade or scissors to cut the knot from the purse-string suture (if present).
Petroleum gauze
Wide, gas-impermeable occlusive tape
Dry gauze sponges (4 in. × 4 in.)
Pulse oximeter (as necessary)
Gloves and eye protection.
Explain the procedure.
Removal of the chest tube will require patient cooperation, and it is somewhat painful. Explain well what is to occur. Use the minimum effective amount of opiate pain medication necessary as high doses can depress respiratory function.
Position the patient: upright or supine.
Remove existing tape.
If present, cut the purse-string suture at the knot, leaving the long ends intact, and unwrap from the chest tube.
Tighten the purse-string suture such that the skin closes tightly around the tube.
Confirm that the tube is free from the suture and tape.
Remove the chest tube.
Have the patient inhale completely and hold his or her breath at the peak of inhalation.
This guarantees a positive pressure in the pleural cavity and does not leave room for an involuntary gasp by the patient when the tube is removed.
While the patient is holding his or her breath, the first person pulls the chest tube out.
The same individual should place the petroleum gauze over the skin site to avoid the influx of air.
At the same time as the tube is being removed, the second person (if present) pulls the ends of the purse-string suture such that the skin seals tightly underneath the petroleum gauze bandage.
Tie down the ends.
Apply dry gauze and occlusive tape to the site.
Obtain a CXR to assess for pneumothorax.
A small amount of air is common and may be treated with 100% O 2 therapy.
Observe the patient over the next few hours for adequate breath sounds and oxygenation.
Examine the patient in 24 hours and obtain a follow-up CXR.
If respiratory distress develops at any time, evaluate the patient for replacement of the chest tube.
Lack of resolution of the problem
Perforation of the lung
Perforation of abdominal viscera
Perforation of the heart
Persistent air leak
Persistent blood leak
Bleeding at the entry site
Loss of underwater seal fluctuation
Shortness of breath (SOB)
Subcutaneous emphysema (SE)
Discomfort at the tube entry site
This is manifest by continuous bubbling in the underwater seal compartment of the drainage apparatus (see Fig. 31.1B ). It may be present with or without the application of suction to the tube.
Why was the chest tube inserted?
How long ago was the tube inserted?
Is the patient short of breath?
Has the patient undergone a surgical procedure, and if so, how long ago?
Are there any other symptoms?
Are there any changes in vital signs?
Is the chest tube on suction?
If there is a significant change in vital signs or symptoms, the patient must be evaluated immediately.
What causes persistent air leak?
Loose tubing or connectors
Air leaking into the chest
From the entrance wound
From a new bronchial or pulmonary injury
Persistent bronchopleural fistula
After thoracic surgery (lobectomy and open biopsy)
After a closed chest procedure (needle biopsy and thoracentesis)
Resulting from ruptured bleb (asthma and emphysema)
After thoracic trauma
Hypoxia, if the air leak is new or if it is associated with SOB
Pneumothorax
If the air leak is small, the patient may look comfortable. A patient who has a new pneumothorax may look acutely distressed.
Review why the chest tube was placed.
Discern if the air leak had ever resolved.
If the patient is recovering from a thoracic procedure, the air leak may persist for 2 to 5 days. A new air leak may indicate a complication derived from the procedure or from placement of the chest tube.
| VS: | Increased respiratory rate (RR; hypoxia) |
| Resp: | Unilateral decrease in aeration, and hyper-resonance (pneumothorax) |
| Tubes: | Are the connections secure? Connect to –20 mm Hg H 2 0 of suction if on water seal. |
| Special intrapleural | Some air leaks are small and will be examination: noted only during increases in pressure such as coughing |
| Additional tests: | Pulse oximetry (hypoxia) |
Check for hypoxia with a pulse oximeter.
Supply supplemental oxygen as required (see Chapter 28 ).
Check the tubing between the drainage apparatus and the patient for loose connections.
Untape the wound site and confirm that the chest tube is inserted properly.
Each chest tube has a visible line a few centimeters away from the most distal holes. The tube must be inserted such that the line is at or inside the skin incision.
If the entry site is not well closed or if a sucking sound is noted at the site, it may be necessary to close the site further with 2-0 silk sutures.
Be sure to adequately prepare and anesthetize the area before repair.
Reposition the chest tube if necessary, and re-dress the site using petroleum gauze. It is not advisable to advance a chest tube once in position as this may introduce bacteria into a sterile environment leading to empyema. Instead, it may be necessary to remove the current tube and replace at a second site.
If the connections are intact and the site is dressed in an airtight manner, order a portable AP CXR to assess the patient’s lungs and the tube position.
If the CXR shows lack of resolution of pneumothorax, consider placement of a second tube.
Why was the chest tube inserted?
How long ago was the tube inserted?
Is the patient short of breath?
Has the patient undergone a surgical procedure, and if so, how long ago was it performed?
Are there any other symptoms?
Are there any changes in vital signs?
Does the patient have a history of trauma to the chest?
Order a hematocrit as a baseline if the bleeding is brisk.
If there is a significant change in vital signs or symptoms, the patient must be evaluated immediately.
What causes excess blood efflux?
Erosion of the tube into artery or vein
Coagulopathy
Injury to an intercostal neurovascular bundle
The result of a blunt or penetrating trauma to the chest
Laceration of lung parenchyma.
Hypotension and shock if the blood loss is great
Disseminated intravascular coagulation (DIC)
Hypoxia
Massive blood loss may result in shock. The patient may be lethargic or comatose. Hypoxia will result in agitation.
Severe fluid loss may lead to tachycardia and hypotension. Hypoxia may be associated with tachypnea.
Review why the chest tube was placed.
Is the patient taking an anticoagulant such as warfarin or heparin?
Can the medication be safely reversed?
Determine the amount of blood lost and whether the current efflux rate is a change.
Check for hypoxia with a pulse oximeter.
Supply supplemental oxygen as required (see Chapter 28 ).
If tachycardia or hypotension is present, begin fluid resuscitation with normal saline (NS) or lactated Ringer’s (LR) (see Chapter 12 , Chapter 17 ).
Start a large-bore IV.
Give 500 to 1000 mL NS or LR quickly.
Send blood for a crossmatch for 4 to 6 units of packed red blood cells.
Order a portable AP CXR immediately.
If the tube is capable of autotransfusion, consider transfusion with the output.
If coagulopathy is present, correct with fresh frozen plasma or cryoprecipitate as per Chapter 26 .
If the rate of loss is greater than 30 mL/hour over 3 to 4 hours, consider returning to the operating room (or consult a thoracic surgeon, if the patient is not already a thoracic surgery patient).
Bleeding is common after open thoracic procedures.
This generally tapers off by 24 hours after the operation. If the bleeding does not abate, consider evaluating the patient for coagulopathy (prothrombin time [PT], partial thromboplastin time [PTT], fibrinogen, fibrin degradation products, and platelets) or continued surgical bleeding.
New onset of blood in the chest tube may indicate a complication of the tube. It left-sided and pulsatile, clamp the tube and hold firmly in its position. This may represent a cardiac injury, which is life threatening. If the tube is dislodged, the patient may bleed into their chest rapidly.
Why was the chest tube inserted?
How long ago was the tube inserted?
Is the patient short of breath?
Has the patient undergone a surgical procedure, and if so, how long ago was it performed?
Are there any other symptoms?
Are there any changes in vital signs?
Brisk bleeding in a patient is a serious finding, and the patient must be seen immediately. If there is a significant change in vital signs or symptoms, the patient must be evaluated immediately.
What causes bleeding around the entry site?
Inadequate hemostasis during insertion of the tube
Inadequate closure of the incision site after removal of the tube
Coagulation disorders
Trauma to intercostal vessels during insertion of the tube
Loss of patency of the chest tube
Blood from the pleural space may drain around the tube.
Hypotension and shock if the blood loss is great
DIC
Most bleeding is mild and is not associated with changes in patient condition. Severe bleeding, however, may be associated with development of shock. The patient may be lethargic or comatose. Hypoxia will result in agitation.
Severe fluid loss may lead to tachycardia and hypotension. Hypoxia may be associated with tachypnea.
Review why the chest tube was placed.
Is the patient taking an anticoagulant such as warfarin or heparin?
Can the medication be safely reversed?
Determine the amount of blood lost and whether the current bleeding rate is a change.
Note also the output through the chest tube lumen.
Check for hypoxia with a pulse oximeter.
Supply supplemental oxygen as required
Untape the wound site; inspect the wound.
If the entry site is not well closed, it may be necessary to close the site further with 2-0 silk sutures. Be sure to adequately prepare and anesthetize the area before repair. Look for sites of active bleeding and ligate as necessary.
Re-dress the site using petroleum gauze.
Apply a pressure dressing.
If the chest tube is clotted, milk the tube to attempt to clear it.
Special chest tube stripper instruments are available for this purpose, or it may be accomplished by lubricating the tube with lotion and using your fingers to milk the tube toward the drainage apparatus. If you are unable to clear the tube or if the tube size is inadequate to manage the amount of drainage, consider replacement of the tube through a different site.
Why was the chest tube inserted?
How long ago was the tube inserted?
Is the patient short of breath?
Has the patient undergone a surgical procedure, and if so, how long ago was it performed?
Are there any other symptoms?
Are there any changes in vital signs?
Loss of fluctuation of the underwater seal is a common but potentially serious problem. It indicates that the chest tube is not functioning properly. The patient should be seen fairly soon. If there is a significant change in vital signs or symptoms, the patient must be evaluated immediately.
What causes loss of underwater seal fluctuation?
Kink in the tubing
Occlusion of the tubing
Improper positioning of the chest tube within the pleural cavity
Tension pneumothorax
Accumulation of fluid within the pleural space because of inadequate drainage
A patient with a tension pneumothorax will appear acutely ill. Hypoxia, hypotension, and shock may follow.
Hypotension and tachypnea are indications of pneumothorax.
Review why the chest tube was placed.
How long has the tube been malfunctioning?
What volume has been draining from the tube?
Check for hypoxia with a pulse oximeter.
Supply supplemental oxygen as required (see Chapter 28 ).
Check the tubing between the drainage apparatus and the patient for loose connections. Look also for regions of clotting or kinking.
Confirm that the suction is appropriately applied.
Inspect the tube and drainage apparatus.
There are two regions that give clues to the function of a chest tube ( Fig. 31.5 ). The underwater seal chamber (see Fig. 31.1B ) is a low-pressure, one-way valve. Gas will bubble through this chamber if there is a continuous flow of air through the chest tube from the patient (such as a persistent air leak). Fluctuations also may be observed if there is fluid present in the tubing itself between the patient and the drainage apparatus. Often fluid will collect in dependent regions of this tubing and will act as an additional underwater seal site. Fluctuations in this region indicate normal functioning of the chest tube between this site and the patient. Have the patient cough during your observation of this region.
Attempt to milk the tubing with strippers or your fingers to loosen a clot.
If these measures do not re-establish normal chest tube function, obtain a portable AP CXR immediately.
Check for proper placement of the tube and for persistence or worsening of the intrapleural pathology. A new tube may need to be placed.
See also Chapter 28 .
Why was the chest tube inserted?
How long ago was the chest tube inserted?
Is the patient short of breath?
Has the patient undergone a surgical procedure, and if so, how long ago was it performed?
Are there any other symptoms?
Are there any changes in vital signs?
Check for hypoxia with a pulse oximeter.
Supply supplemental oxygen as required (see Chapter 28 ).
Have a 16-gauge angiocatheter available at the bedside for use for diagnosis and to treat tension pneumothorax.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here