Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
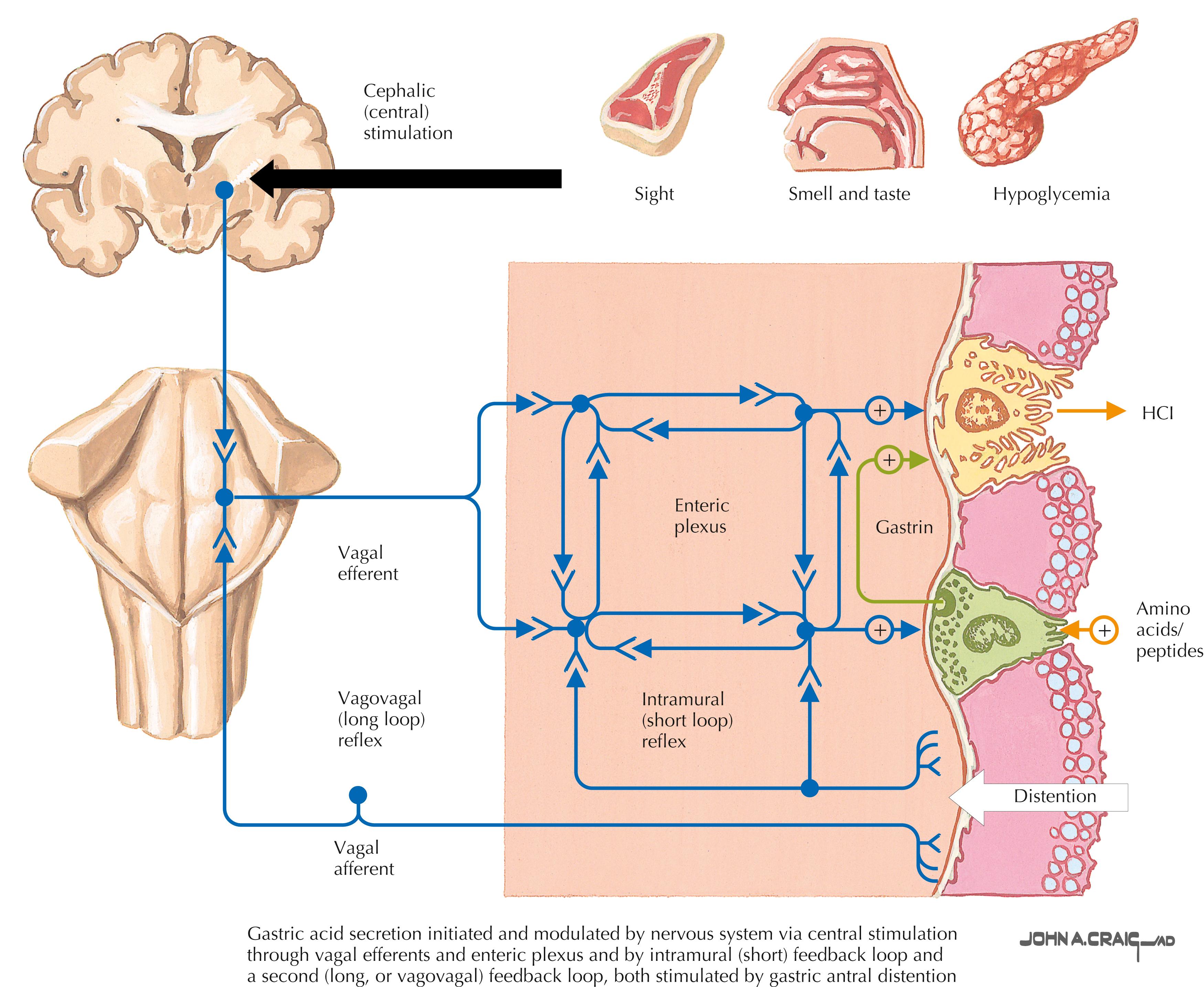
Gastric acid production contributes to duodenal and gastric ulcer formation. Intraluminal gastric acid is released by parietal cells, which in turn are stimulated via three mechanisms: gastrin, histamine, and acetylcholine. All three mechanisms activate the hydrogen-potassium ATPase-releasing hydrogen ions into the stomach lumen. Specifically, acetylcholine is released in response to parasympathetic stimulation, which travels in the fibers of the vagus nerves ( Fig. 7.1 ). When pharmacologic therapy is not enough to decrease acid production, surgical vagotomy intervention can be applied to interrupt this neural pathway anatomically. There are three different techniques options described: truncal vagotomy (TV), selective vagotomy (SV), and highly selective vagotomy (HSV). Furthermore, technological advances have allowed for these operations to be performed with minimally invasive techniques, which have translated into fewer procedure-related complications.
Although acid-reducing surgery has become an operation with few indications, it is still an essential tool in the surgeon armamentarium. Vagotomy is currently indicated for intractability or complication of peptic ulcer disease in a stable patient who has failed maximum medical therapy and more recently, owing to the rapid increase of bariatric surgeries worldwide, as a surgical treatment alternative for marginal ulcers post-Roux-en-Y gastric bypass (RYGB). When performing acid-reducing surgeries, surgeons must understand the anatomy, physiopathology, and clinical implications of different techniques and approaches as well as their potential postoperative complications.
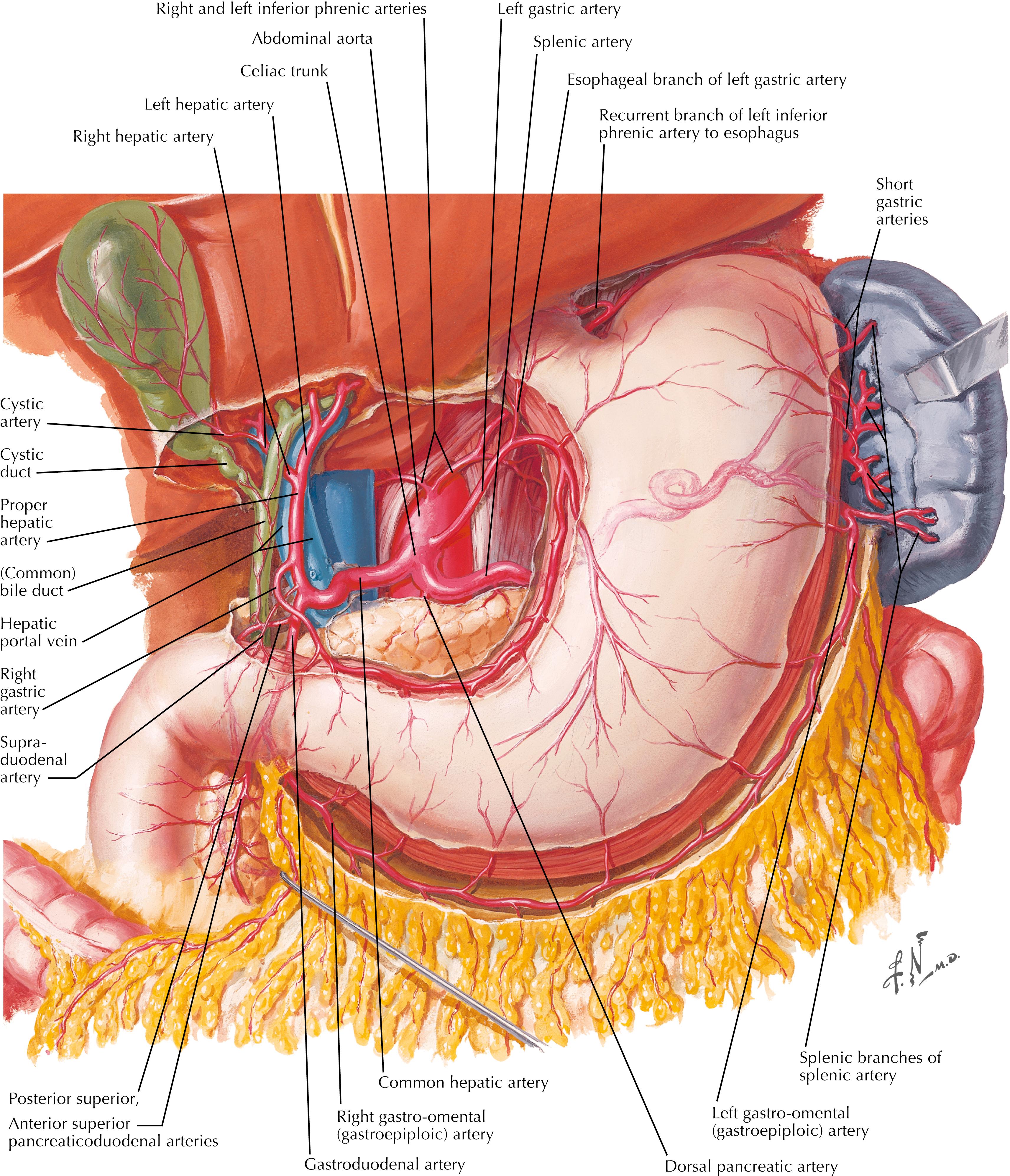
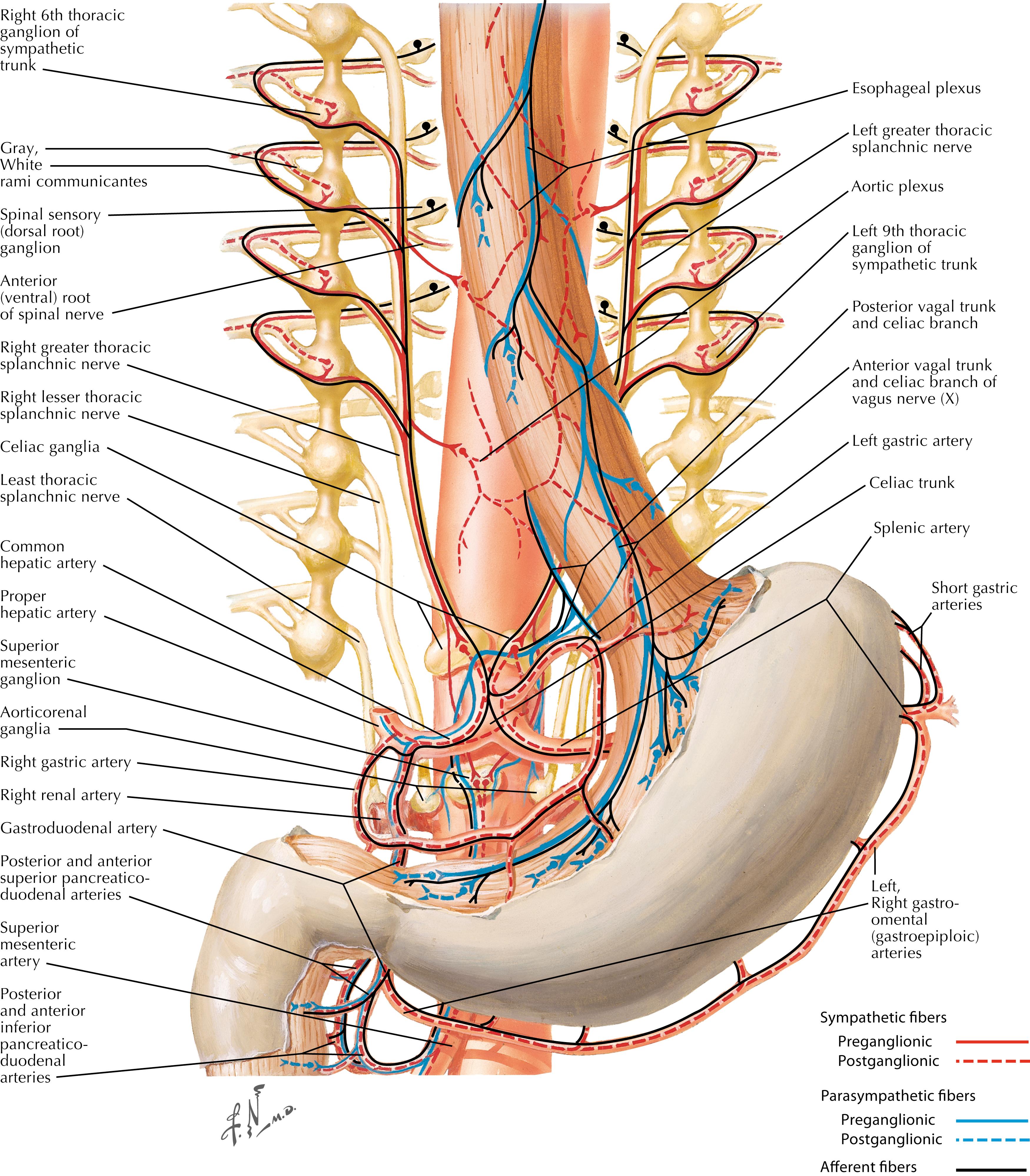
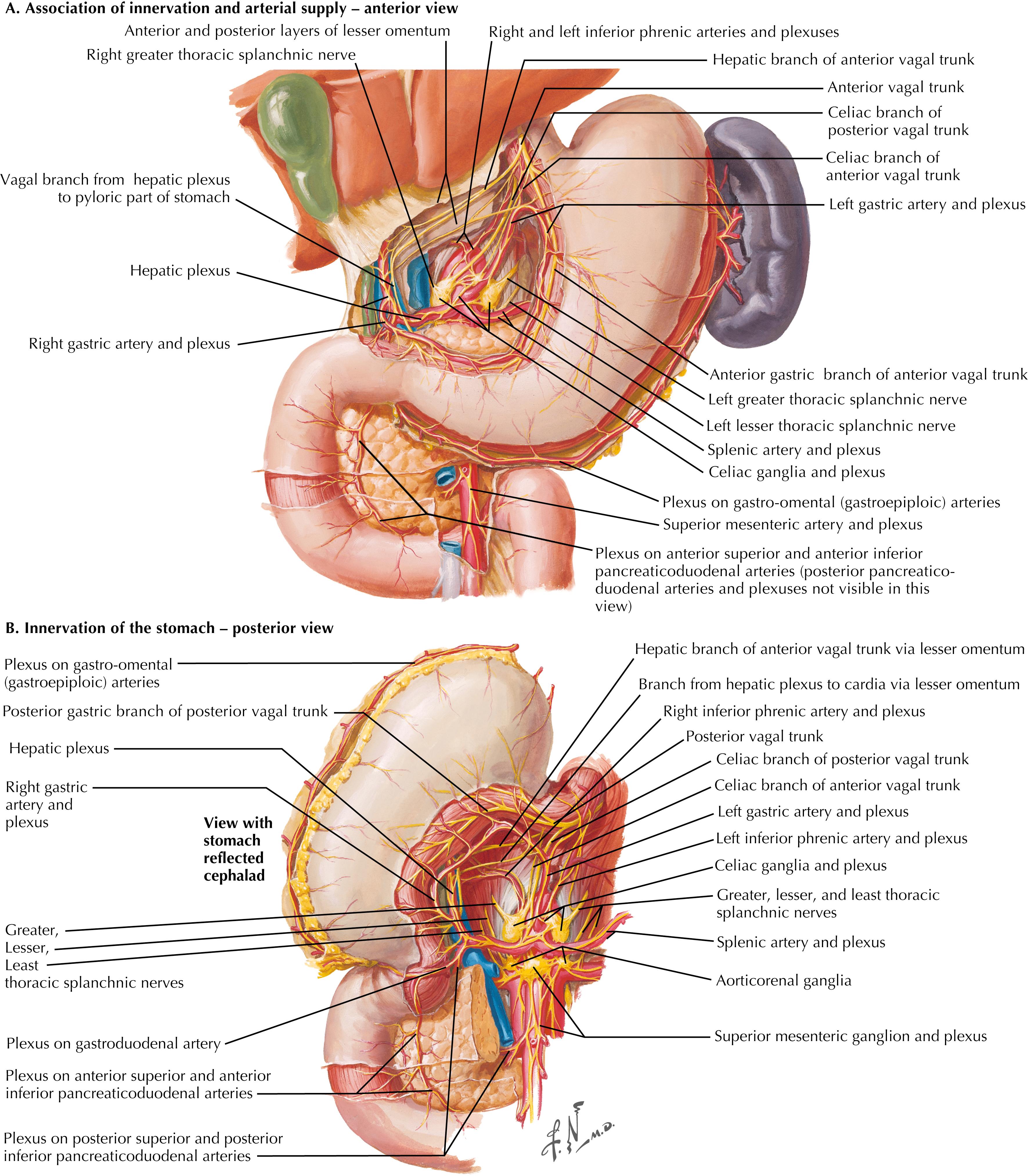
Sympathetic innervation follows that of the arterial supply of the stomach ( Figs. 7.2 through 7.4 ). Parasympathetic innervation, on the other hand, is controlled by the right and left vagus nerves, which enter the thoracic cavity along with the esophagus. As the two trunks enter the abdomen, they rotate so that the left trunk becomes anterior and the right trunk posterior to the esophagus. Both trunks innervate the stomach along the lesser curvature and induce the parietal cells to secrete hydrochloric acid as well as control the motor activity of the stomach. The left vagus nerve gives off branches that innervate the liver, biliary tract, and gallbladder. The right vagus nerve innervates the colon, small intestine, and pancreas. Importantly, the right branch also creates a small branch behind the esophagus named the “criminal nerve of Grassi,” which, if missed and not divided, can lead to recurrent disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here