Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Authors are grateful to Melanie French and Jesse Gaboury for their help reviewing the final version of this chapter.
In , Anthony Barker et al. published in Lancet the first report of a new contactless and painless method for stimulating the motor cortex (MC). This novel method used a device to deliver a magnetic pulse over the MC to elicit a recordable electromyographic (EMG) response over the contralateral abductor digit minimi . This was not the first time that cortical stimulation, using noninvasive methods was performed. Indeed, in Merton et al. had already successfully used skin electrodes to induce electrical currents in the brain and the spinal cord, but this was the first time that a magnetic stimulator was used to induce a pain-free, muscle-evoked potential (MEP) ( ). This was the first report of the use of transcranial magnetic stimulation (TMS). In the following 30 years, TMS has evolved to a more refined technique, with multiple diagnostic and therapeutical uses. In this chapter, we will review the basic mechanisms of TMS and its safety profile, and provide a brief overview regarding its clinical diagnostic and therapeutic utilities as well as how it can be used to understand brain and behavior.
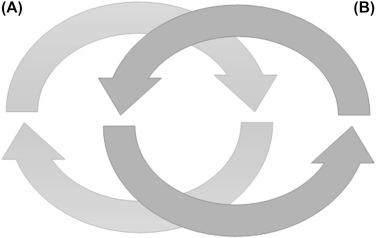
The effect of TMS can be understood, based on the electromagnetic induction principle, proposed in 1831 by Michael Faraday. Electrical current flowing over a stimulation coil creates a changing magnetic field that is able to induce current flow over nearby conductors. In TMS, the current that flows through the coil generates an electromagnetic field that is able to induce eddy currents in a nearby neuron population. Please note in Fig. 134.1 that eddy currents (A) have the opposite direction to the ones (B) that generate them.
A TMS stimulator, in basic terms, is a high-current pulse generator that is able to produce a current discharge of thousands of amperes, which in turn is able to generate a brief magnetic pulse (around 100 μs) with a magnitude that can go up to several Tesla. If the coil is placed over the head, there is little attenuation to the magnitude of the pulse when it crosses tissues such as the scalp, cranial bones, meninges and liquor and therefore the induced electrical current is able to depolarize the underlying neuron population and induce effects over neural networks.
These TMS induced effects are modulated by several biological and physical parameters such as the distance between the coil and the target area, coil orientation and shape, pulse waveform, and several pulse parameters, such as intensity, frequency, latency between pulses, and pattern of stimulation, among others.
The cortex is an inhomogeneous conductor with conductivities ranging from 0.14 S/m (Siemens per meter) for the white matter to 1.79 S/m for the cerebrospinal fluid, while cranial bones have an estimated conductivity of 0.01 S/m ( ). So, the actual current density, induced by a TMS pulse, will be dependent on the tissue conductivity, but also on the distance between the coil and the stimulation target. Although the distance of a magnetic field is theoretically infinite, the common assumption is that it decays with the square of the distance. This limits the depth of TMS induced electrical fields to a few centimeters, usually between 0.9 and 3.5 cm ( ) and thus potentially more suitable for stimulating cortical, rather than subcortical regions. This fact is why some “deep brain” TMS coils were developed with the ability to deliver 81% of the maximal, induced, electrical field at skull, at a depth of 4.5 cm, when compared to 12% from the standard 70 mm figure-8 coil ( ).
The intensity of the magnetic field and the shape of the coil not only determine the depth of the induced electrical field but also the area of stimulation. Circular coils were the first ones to be used and are usually between 80 and 150 mm in diameter. Circular coils are not very focal, as the maximal, electrical current field is induced in the outer regions of the coil, with a maximum magnetic field in the center of the coil. Thus, the site of stimulation is not actually the center of the coil, but instead the regions surrounding the outer edge of the coil. Due mainly to its size, circular coils have a good penetration into the skull, and by placing them over the vertex, they can activate both hemispheres simultaneously. In the event of a monophasic pulse, the effects of such coils in the hemispheres will be asymmetric, mainly because the effect will be greater in the hemisphere in which the current flows in a posteroanterior direction ( ). The main caveat of such coils is its lack of focality, as the induced electrical field across the outer edge of the coil is pretty much similar all around.
To increase focality, figure-8 coils were developed. By placing two round coils side by side, the current will flow in the same direction at the junction point, which results in a summation of the electrical field and allows focal stimulation to a specific target. But the figure-8 coils are smaller (usually 70 mm) than circular ones, and thus, the resulting effect is a more modest penetration. Nonetheless, this claim has been challenged by the use of double cone, figure-8 coils, which have higher penetration in the skull than the figure-8 flat coils. Overall, figure-8 flat coils have a great compromise between focality and penetration and are the most common coils used for clinical purposes and research.
TMS has been used to probe cortical excitability, facilitatory, and inhibitory cortical mechanisms, to indirectly infer about the underlying neurophysiologic neurotransmission processes and to alter cortical excitability and/or brain function. The effect of TMS will be dependent on several parameters such as pulse waveform, intensity of the electrical field, the number of pulses, as well as the interval between pulses and trains.
If a single pulse of TMS is delivered over MC, it can depolarize the motor neurons and cortical excitability can be probed noninvasively. If electrical current is delivered to peripheral nerves, it is possible to elicit an evoked electromyographic activity in the innervated group of muscles, or an MEP. Similarly, a single TMS pulse over the cortical representation of those muscles can be used to induce an evoked electromyographic response over that group of muscles. The resulting MEP can be recorded and cortical excitability can be inferred. The actual size of the MEP (i.e., amplitude) will not be a direct product of the stimulus intensity, but a combination of three factors: the number of recruited neurons, the number of neurons that will actually discharge more than once, and the TMS-induced discharge synchronization across motor neurons. This leads to an assumption that MEP amplitude then increases with TMS output intensity, which has been thought to represent increased corticospinal and spinal neural recruitment. Nonetheless, there is a considerable interindividual variation in the stimulus response variation. For instance, standardizing TMS to the resting motor threshold (RMT) (i.e., minimum intensity to elicit MEPs with 50 μV, peak-to-peak, in 50% of the trials) ( ) does not ensure that all subjects will reach the same MEP amplitude. And if the intensity is increased by 20%, the interindividual variability increases, ranging from 6% to 100% of MEP, at maximum amplitude ( ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here