Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
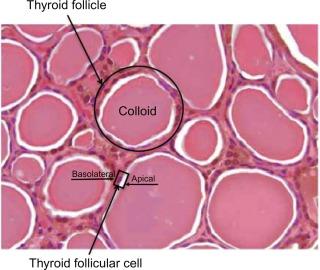
The basic functional unit of the thyroid gland is the thyroid follicle. The thyroid follicle contains a single layer of thyroid follicular cells that form a sphere with a follicular lumen, which is filled with a colloid protein aggregate. Thyroid follicular cells are polar; the apical membrane is adjacent to the follicular lumen, and the basolateral membrane is the one in contact with capillaries and the circulatory system ( Figure 3.1 ). Thyroid hormone synthesis is activated by the binding of thyroid-stimulating hormone (TSH) to the TSH receptor on the basolateral membrane, which activates adenylate cyclase and increases intracellular cyclic adenosine monophosphate (cAMP). This initiates the cascade that results in thyroid hormone synthesis and secretion, which includes iodide transport, synthesis of thyroglobulin, iodination of thyroglobulin, and secretion of the thyroid hormones (see Figure 3.1 ).
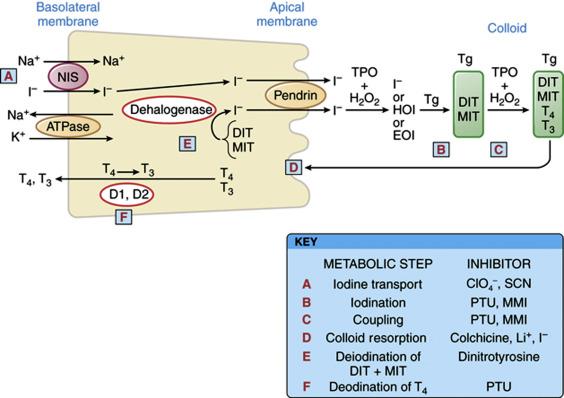
After the binding of TSH, the initial step in the thyroid hormone synthesis pathway is iodide transport across the basolateral membrane, mediated by the Na + /I (NIS) symporter. NIS is a sodium-dependent transporter, so iodine is only transported with an inward sodium gradient, which is in turn maintained by the action of the Na-K-ATPase. The transported iodide ion becomes covalently attached to the precursor thyroid hormone glycoprotein, thyroglobulin, at the interface between the apical membrane and the follicular lumen by the enzyme, thyroperoxidase (TPO). Tyrosine molecules in the thyroglobulin molecule are then iodinated to form monoiodotyrosines (MITs) and diiodotyrosines (DITs) ( Figure 3.2 ). Incorporation of iodide into protein is referred to as organification . The bioactive thyroid hormones, L-thyroxine (T4) and triiodothyronine (T3), are formed by the coupling of two DITs or one DIT with one MIT, respectively, by TPO (see Figure 3.2 ). T4 and T3 remain attached to thyroglobulin and are stored as colloid within the follicular lumen, where they remain available for release through TSH stimulation. In healthy and iodine-sufficient individuals, the majority of thyroid hormone in colloid is stored as T4 with a small amount (~ 20%) stored as T3. Upon stimulation of the TSH receptor, a cytoplasmic vesicle is formed for uptake of colloid into the follicular cell through pinocytosis (see Figure 3.2 ). The cytoplasmic vesicles fuse with lysosomes, from which proteases hydrolyze the peptide bonds of thyroglobulin to release T4 and T3 into the cytoplasm. The thyroid hormone transporter, monocarboxylate transporter 8 (MCT8), is expressed in the thyroid gland and is important for transport of T4 and T3 out of the thyroid gland and into the circulation. Production of thyroid hormone varies widely between 75 and 250 mcg daily.
In the blood, approximately 99.97% of T4 and 99.7% of T3 are bound to the binding proteins, thyroxine binding globulin (TBG), transthyretin (also known as prealbumin ), and albumin. Of these, TBG has the highest affinity to bind thyroid hormone (binding approximately 75% of both T4 and T3 in circulation) and is the most clinically relevant among the binding proteins. Transthyretin, previously referred to as prealbumin , binds approximately 20% of the circulating T4 and < 5% of T3. Albumin has the lowest affinity for thyroid hormone, but is the most abundant of the proteins and binds 5% of the T4 and 20% of the T3. In total, most of the thyroid hormones in circulation are in the bound state and biologically inactive. The unbound thyroid hormones, free T4 and free T3, enter the target cells. In some tissues, such as those from the brain and pituitary, specific thyroid hormone membrane transporters are required for thyroid hormone uptake, principally MCT8. T3 binds with a much greater affinity to the thyroid hormone receptors and for a longer period of time, compared with T4, and is regarded as the primary active thyroid hormone.
T4 is synthesized exclusively by the thyroid gland, whereas T3 is produced primarily in peripheral tissues from the deiodination of circulating T4. Only about 20% of the daily T3 requirement is synthesized directly by the thyroid gland. The activation of T4 to T3 requires the 5′-deiodinase enzymes type 1 (Dio1) and type 2 (Dio2). These enzymes are differentially expressed, with Dio1 predominantly in the liver and Dio2 in tissues that require local T3 production, such as the brain, pituitary, muscle, and brown fat. In the setting of fluctuating T4 levels, deiodinase activity is modulated to maintain normal circulating and target tissue T3 levels ( Figure 3.3 ). When serum T4 levels fall, as in hypothyroidism, Dio2 is activated locally by a deubiquitination process that reduces Dio2 degradation, increases Dio2 activity, and promotes greater conversion of T4 to the bioactive T3. Normal serum T3 levels are maintained until the serum T4 becomes very low.
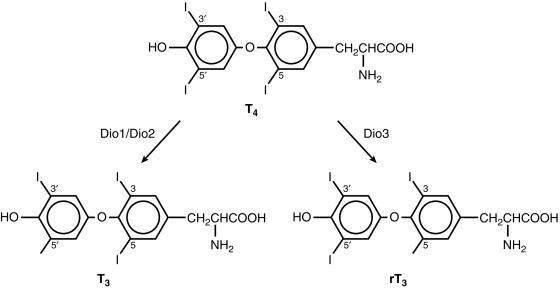
Thyroid metabolism is influenced by illness and drugs. The activity of Dio1 and the resulting T3 level is reduced in malnutrition, critical illness, and by the action of certain medications (e.g., beta-blockers, ipodate, amiodarone, dexamethasone, propylthiouracil). During starvation and acute illness, expression of the 5 deiodinase type 3 (Dio3) is increased and converts the bioactive T4 and T3 to two biologically inactive molecules, reverse T3 (rT3) and 3,3′-diiodothyronine (T2).
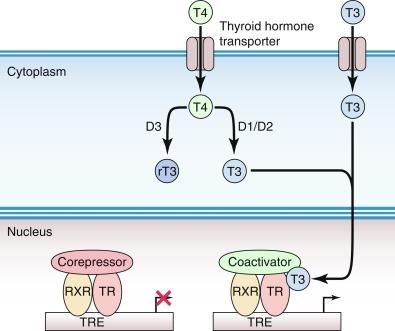
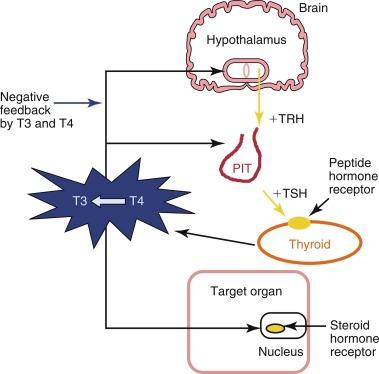
The available free T3 binds to a nuclear thyroid hormone receptor at the target tissue, alters gene expression, and regulates cellular function ( Figure 3.4 ). The thyroid hormone nuclear receptor (THR) is a protein within a superfamily of receptors that bind steroid and steroid-like hormones such as retinoic acid, vitamin D, and estrogen. The THRs mediate the majority of biologic activities of T3. Two THR genes , alpha and beta, encode four THR isoforms (alpha 1, beta 1, beta 2, and beta 3). The transcriptional activity of THRs is regulated by the binding of T3, the type of thyroid hormone response elements located on the promoters of the T3 regulated gene, by the developmental- and tissue-dependent expression of THR isoforms and by nuclear cofactors or coregulatory proteins.
There are also nongenomic actions of iodothyronine (T4) that are not mediated by intranuclear THR. Action at the plasma membrane is mediated by the integrin alpha-v beta 3 receptor that binds T4, and activates ERK1/2, which leads to changes in membrane ion transport, such as the Na( + )/H( + ) exchanger, and is also involved in other important cellular events such as cell proliferation.
Significant changes in thyroid physiology occur during pregnancy and can make the interpretation of serum thyroid function tests challenging. During the first trimester of pregnancy, serum TBG concentrations increase by up to 50% as a result of altered estrogen induced glycosylation, which prolongs TBG half-life. The elevated TBG levels increase the quantities of protein-bound T4 and T3, which results in an increase in total serum T4 and T3 concentrations; however, in euthyroid individuals, the active or free levels of T4 and T3 remain normal.
In addition, during the first trimester of pregnancy, levels of placental human chorionic gonadotropin (hCG) steadily increase. Because hCG is a weak TSH receptor agonist, this results in a small increase of free T4 (although still within the normal range) and a concomitant decrease in TSH, below the lower reference range in up to 15% of normal women in the first trimester. Serum TSH concentrations should thus be assessed using trimester-specific ranges during pregnancy. The changes of reduced TSH and elevated FT4 are more pronounced in pregnancies associated with higher levels of hCG, such as multiple gestations and hyperemesis gravidarum, and are most extreme in hydatidiform moles. The physiologic suppression of TSH does not require medical intervention and usually normalizes after the first trimester of pregnancy.
The evaluation of a chronically ill or hospitalized patient with abnormal serum thyroid function tests can often be challenging. Nonthyroidal illness is not considered a primary thyroid disorder, and its pathophysiology is not completely understood, although it is known that the elevation of cytokines and hypoxia plays a significant role. It is generally recommended to avoid measuring serum thyroid function tests during acute illness, unless thyroid dysfunction is thought to be a significant contributor to the illness.
Severe nonthyroidal illness is accompanied by significant alterations in thyroid physiology. Due to the decreased availability in all of the thyroid binding proteins, serum total T4 and total T3 levels are reduced, whereas free levels are usually normal or slightly low ( Figure 3.5 ). Total T3 levels are further decreased due to reduced Dio1 activity, which converts T4 to T3. A relatively greater amount of T4 is metabolized to the inactive metabolite, reverse T3 (rT3), by Dio3, although measurement of rT3 does not reliably distinguish nonthyroidal illness from primary hypothyroidism. The degree of serum rT3 elevation, depressed T3/rT3 ratio, and decreased FT3 and FT4 concentrations have been associated with higher mortality among patients in the intensive care unit (ICU). Treatment with T4 or T3, however, does not consistently improve outcome. Whether other T4 metabolites, including 3,3′-diiodothyronine (3,3′-T2); 3,5-diiodothyronine (3,5-T2); and 3-iodothyronamine (3-T1AM), have functional roles in nonthyroidal illness remains unclear.
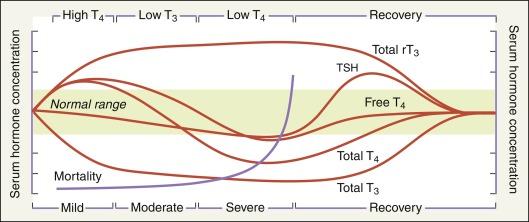
It is important that the diagnosis of primary thyroid dysfunction is not established during severe illness based solely on an abnormal serum TSH. In nonthyroidal illness, serum TSH concentrations may be low, normal, or high, due to the TSH-lowering effects of commonly used medications (glucocorticoids, dopamine) in patients managed for a nonthyroidal illness or from a reversible form of acquired central hypothyroidism in severe nonthyroidal illness. During the recovery phase, the TSH may briefly rise above the upper reference range, as suppression of TSH lessens, before it normalizes. When possible, thyroid evaluation after recovery from an acute illness is recommended in patients suspected of having intrinsic thyroid disease.
TSH is produced from the pituitary after stimulation by thyrotropin-releasing hormone (TRH), a modified three-amino acid peptide produced by neurons of the paraventricular nucleus in the hypothalamus. TRH signaling from the hypothalamus is achieved through a portal venous system located in the infundibulum of the pituitary stalk, which allows communication to the pituitary. Both TRH and TSH gene expression are decreased by excess thyroid hormone levels via negative feedback mechanisms ( Figure 3.6 ). Both the hypothalamus and pituitary have high levels of Dio2, so T4 levels are the primary feedback. T4 is converted locally to T3, which suppresses TRH and TSH gene expression.
Pituitary TSH is secreted in a pulsatile manner—higher levels at night and lower levels during the day, the inverse of the cortisol cycle. Although pulse frequency is increased nocturnally to result in a diurnal variation of TSH concentrations, levels remain within the reference range. Generally, laboratory testing of serum TSH concentrations during daylight hours is not substantially affected by the diurnal variation of TSH secretion, but results outside the reference range may occur in euthyroid individuals when drawn outside of these times.
TSH stimulates the synthesis and release of thyroid hormone from the thyroid gland. TSH production from the anterior pituitary is inverse log-linearly regulated by serum thyroid hormone concentrations; when there are small decreases in thyroid hormone levels in circulation, large increases in serum TSH stimulate thyroid hormone production by the thyroid gland. This negative feedback loop between serum TSH and the serum-free thyroid hormones is able to maintain circulating thyroid levels within a tight range.
Serum TSH is the preferred screening test in the evaluation of thyroid function in the ambulatory patient, regardless of whether the patient is taking thyroid hormone replacement medication. For the healthy patient in an ambulatory setting, the diagnosis of hypothyroidism or hyperthyroidism may be determined with approximately 98% sensitivity and 92% specificity using serum TSH. In addition, TSH has a narrow intraindividual variability of ± 0.5 mIU/L, such that thyroid dysfunction may be present if there are significant changes in TSH values over time in an individual, even if they remain within the reference range. In certain situations, however, such as known or suspected pituitary or hypothalamic dysfunction, recent hyperthyroidism, critical illness, starvation, use of certain medications (dopamine or high-dose glucocorticoids), interference with serum thyroid autoantibodies, and thyroid hormone resistance syndromes, the TSH level is inaccurate for the thyroidal status and should not be used in isolation to determine thyroid function. In addition, the presence of interfering heterophile antibodies (antibodies against the animal-derived antibodies used in the immunometric assay) may rarely cause abnormally high or low TSH levels. These conditions should be suspected when the pattern of the TSH levels does not correlate to the clinical presentation or when the peripheral serum hormone levels do not change as expected with elevated or suppressed serum TSH concentrations.
Serum TSH assays have evolved considerably since measurements were first described in the 1960s, when the functional sensitivity was between 1 and 2 mIU/L. The commonly used second-generation TSH assays have an improved functional lower limit of 0.10 to 0.20 mIU/L, which is able to differentiate between euthyroid and hyperthyroid states but does not indicate the degree of hyperthyroidism. In contrast, a third-generation TSH assay can detect levels as low as 0.01 to 0.02 mIU/L and is helpful when there is a challenging pattern of serum thyroid function tests that include an extremely suppressed TSH. In the rare instance they are needed, fourth-generation immunochemiluminometric assays are capable of detecting TSH levels in the range of 0.01 to 0.001 mIU/L.
A serum TSH level measured in an ambulatory population that lies within the reference range is generally considered evidence of normal thyroid function and requires no additional testing ( Figures 3.7 and 3.8 ). Reference ranges for serum TSH can vary slightly from one commercial laboratory to another. It should be noted that normal ranges, which are based on the epidemiologic distribution of serum TSH concentrations in healthy populations, from which serum thyroid autoantibody positivity and iodine status (both of which can affect TSH), may be variable. If an abnormal screening TSH result is encountered, the circulating thyroid hormone levels should be assessed (see Figures 3.7 and 3.8 ). The specific pattern of tests will allow further insight into whether clinical thyroid dysfunction should be suspected.
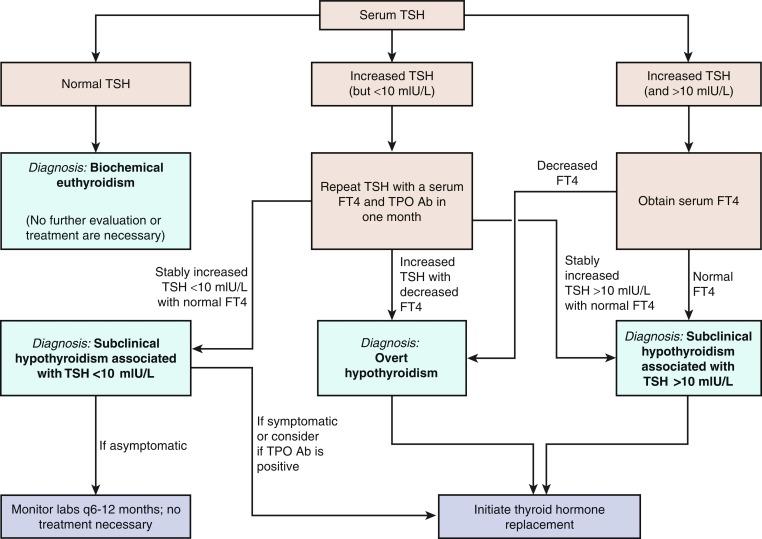
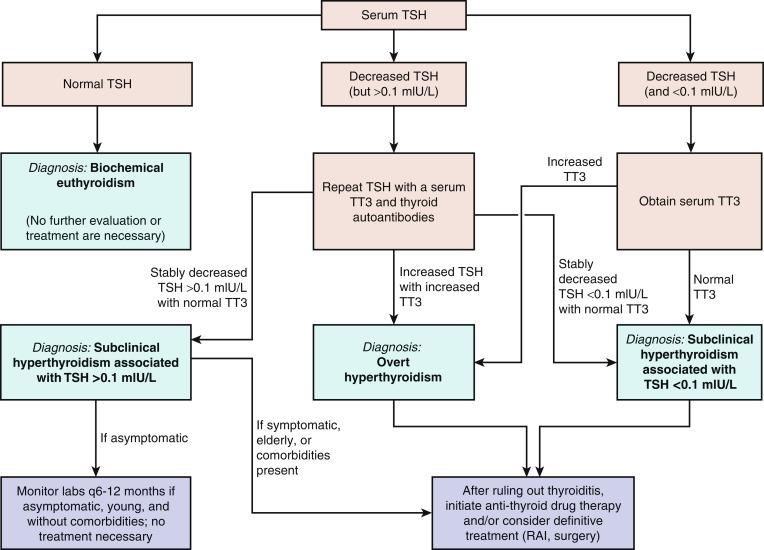
Serum TSH should be the initial choice for the screening of thyroid dysfunction. When the TSH alone is not believed to be sufficient for diagnosis, as in the examples proposed earlier, serum thyroid hormone levels should be assessed.
Serum total T4 (TT4) and total T3 (TT3) concentrations are a measure of both the bound and free hormone levels of these two hormones. TT4 or TT3 levels should be interpreted in the context of the clinical situation, because many clinical conditions and medications alter the concentrations of thyroid hormone binding proteins and/or compete with the binding of thyroid hormones to the binding proteins. As such, measured TT4 and TT3 levels may be affected, even though the bioactive free levels and thus, the thyroidal status, remain unchanged.
T3 is the active thyroid hormone and is primarily useful in the diagnosis and management of patients with hyperthyroidism and occasionally, to differentiate Graves’ disease (TT3/TT4 ratio > 20) from subacute thyroiditis (TT3/TT4 ratio < 12). Measurement of serum TT3 is not usually helpful if hypothyroidism is suspected because the activity of Dio2, which converts T4 to the biologically active T3, increases while serum T4 falls, thus maintaining normal T3 levels until the overall thyroid hormone levels are very low. rT3, which may be elevated during nonthyroidal illness, is not biologically active. As such, the utility of measuring it and other forms of inactive iodothyronine are limited during the evaluation of thyroid status.
Finally, the human anti-mouse antibodies (HAMAs) that interfere with TSH testing can also interfere with the thyroid hormone assays. HAMA positivity may result in artificially elevated or reduced TT4, TT3, FT4, and FT3 levels. Patients who have received therapeutic monoclonal antibody treatment may be at increased risk of develop interfering positive HAMA titers.
Bioactive free T4 concentrations can be estimated using a variety of indirect (analog, immunometric, and two-step labeled hormone assays) or direct methods (equilibrium dialysis, ultrafiltration), and are the most commonly used measurements of circulating thyroid hormone levels.
Generally, most laboratories estimate free T4 by either the analog immunoassay or a calculated FT4I corrected to thyroid hormone binding capacity. The former is readily available and provides quick results; it does not directly measure the free T4 concentration but is a reliable estimate of FT4 levels in most patients, based on one-step, two-step, or labeled antibody approaches. This type of free T4 estimate is especially sensitive to abnormal serum albumin levels and should not be used with conditions such as familial dysalbuminemic hyperthyroxinemia, pregnancy, or severe nonthyroidal illness. For example, it is common to have a free T4 lower than the reference range in a euthyroid pregnant woman due to the high estrogen state of pregnancy greatly increasing serum TBG concentrations, thus resulting in inaccurate FT4 measurements.
The serum FT4I measurement is a calculated value that is the product of the total T4 concentrations and a correction factor related to the number of available thyroid hormone binding sites ( Table 3.1 ). This correction factor may be called a thyroid hormone binding ratio (THBR), T3 resin uptake (T3RU), or T3 uptake (T3U). The T3RU is inversely related to the free thyroid hormone binding sites but is now used in only a few laboratories.
| Clinical Condition | Free Thyroxine | Free T3 | TSH | Thyroid Autoantibodies |
|---|---|---|---|---|
| Subclinical hypothyroidism | Normal | Normal | Mildly elevated, usual range of 5-10 mIU/L | Can be TPO positive or negative |
| Hypothyroidism due to Hashimoto’s disease | Low | Normal or low | Elevated, usually > 10 mIU/L | Usually TPO positive |
| Central hypothyroidism | Low | Normal or low | “Inappropriately” normal or low | Negative |
| Subclinical hyperthyroidism | Normal | Normal | Low | TRAb or TSI may be positive |
| Hyperthyroidism due to Graves’ disease | Elevated | Elevated | Low | TRAb or TSI positive |
| TSH-secreting pituitary adenoma | Elevated | Elevated | “Inappropriately” normal or elevated | Negative |
| Thyroid hormone resistance due to mutation of thyroid hormone receptor beta | Elevated | Elevated | “Inappropriately” normal or elevated | Negative |
Free T4 by equilibrium dialysis is the gold standard and measures the 0.03% of T4 that is biologically active and unbound to protein. This assay is available only at reference laboratories and is useful to directly determine free T4 levels when other testing does not provide a clear result.
Hyperthyroidism and hypothyroidism are often the result of autoimmune diseases, in which immunoglobulin G (IgG) antibodies, such as thyroid peroxidase (TPO Ab, previously known as antimicrosomal antibodies ), thyroglobulin (Tg Ab), and the TSH receptor (TSHR Ab), are formed against thyroid proteins.
More than 90% of patients with autoimmune thyroid disease (Hashimoto’s thyroiditis and Graves’ disease) will have elevated titers of second-generation assays for TPO Ab and Tg Ab. When biochemical hypothyroidism is found, measuring TPO Ab can be helpful, because its result can provide additional information regarding the etiology of the thyroid dysfunction. Median serum TSH concentrations are increased within the reference range among those with serum TPO Ab and Tg Ab positivity, compared with those without TPO Ab titers, and are a predictor for the development of biochemical thyroid dysfunction in euthyroid individuals. In individuals with subclinical hypothyroidism, both serum TPO Ab positivity and sonographic characteristics suggestive of chronic thyroiditis are associated with an increased likelihood of progression to overt hypothyroidism.
The TSHR Abs are a group of immunoglobulins that produce Graves’ hyperthyroidism, measured as TSH receptor binding, TRAB (TSH-receptor antibody) or in a functional bioassay, thyroid stimulating immunoglobulin (TSI). TSH receptor antibodies are being increasingly recommended for monitoring activity of disease to assess response to therapy in Graves’ patients. Less commonly, TSH receptor binding antibodies can block the TSH receptor and produce hypothyroidism. In the setting of normal serum thyroid function, thyroid antibodies should generally not be measured except in special circumstances, such as a history of hyperthyroidism during pregnancy or recurrent miscarriages. In these situations, both the stimulating and inhibiting TSHR Abs can cross the placenta to affect fetal thyroid function and potentially induce fetal goiter. Although serum thyroid antibody positivity during pregnancy is associated with a higher risk of postpartum subacute thyroiditis, antibody screening in pregnant women is not currently recommended.
Thyroglobulin (Tg) is a large glycoprotein that is stored as colloid, the primary storage form of thyroid hormone, in the lumen of thyroid follicles. It is continuously secreted into circulation from the thyroid gland, thereby reflecting the mass of normal and malignant thyroid tissue. Higher serum concentrations result from TSH stimulation and/or injury of thyroid tissue. However, for the individual with an intact thyroid gland, its clinical value for evaluating thyroid dysfunction or goiter is limited in the era of modern serum thyroid function testing and imaging. However, the demonstration of a suppressed serum Tg level in such a patient can be useful in differentiating factitious thyrotoxicosis (from exogenous thyroid hormone ingestion) from excessive endogenous thyroid hormone release of any etiology. In this situation, when thyrotoxicosis is due to ingestion of exogenous thyroid hormone, normal thyroid hormone production is suppressed and serum Tg levels are decreased. In contrast, if excess thyroid hormone is produced from the thyroid, serum Tg levels are elevated.
In current clinical practice, the primary use of serum Tg concentrations is as a tumor marker in patients with differentiated thyroid cancer that is obtained to detect persistent and/or recurrent disease after a total thyroidectomy and radioactive iodine ( 131 I) ablation. Most Tg assays have only first-generation functional sensitivity between 0.5 and 1 ng/mL, but the second generation Tg assays are rapidly becoming the standard and have an improved functional sensitivity of 0.05 to 0.1 ng/mL. The Tg assay can be made more sensitive to detect persistent or recurrent tumor after stimulation by TSH, either endogenously by withholding thyroxine treatment in an athyreotic patient or with administration of recombinant human TSH (rhTSH), the latter of which results in an approximate tenfold increase in basal serum Tg concentrations.
Detection of persistent and/or recurrent disease in thyroid cancer depends on the performance of Tg immunometric assays, which currently have suboptimal sensitivity and high interassay variability. Virtually all immunometric methods will report an undetectable Tg level in euthyroid Tg Ab positive controls, and approximately 25% of patients with differentiated thyroid cancer have a positive serum TgAb titer. Thus when a suspicious lymph node or neck mass is detected in an individual who has undergone a total thyroidectomy, an unmeasurable basal or rhTSH-stimulated Tg in the setting of a positive serum TgAb level does not necessarily exclude thyroid cancer recurrence. It is reasonable in this relatively uncommon situation to measure Tg instead by Tg Ab-resistant radioimmunoassay (RIA) or liquid chromatography tandem mass spectrometry, which are available at some specialty endocrine laboratories.
When the serum Tg Ab titer is positive, it may also be used as a surrogate marker of tumor persistence/recurrence. In one study, a > 50% decrease of Tg Ab levels within the first year after a total thyroidectomy was associated with the absence of tumor recurrence/persistence in all patients studied, and tumor recurrence/persistence was present in 37% of patients who had any rise of serum Tg Ab within the same period. Thus thyroid cancer patients with rising Tg antibody levels are at high risk for disease persistence/recurrence and should be evaluated promptly. In addition, the sensitivities and absolute values reported by different methods of measuring Tg and TgAb are highly variable. It is essential to always use the same Tg and TgAb method when following an individual over time for tumor persistence/recurrence.
Finally, the presence of interfering heterophile antibodies (antibodies against the animal-derived antibodies used in the immunometric assay) may rarely result in abnormally high or low serum Tg levels. The most common interfering antibodies are HAMAs, which were discussed earlier. Clinically, this should be suspected when an elevated serum Tg level is inappropriate for the clinical situation and does not increase with rhTSH stimulation. When heterophile antibody is suspected, the clinician should repeat the test using a commercially available heterophile-blocking tube (HBT) or measure Tg with an RIA assay.
Thyroid gland imaging studies with radionuclides provide both structural and functional information and can be very useful in determining the etiology of biochemical hyperthyroidism. In contrast, thyroidal nuclear imaging is not recommended in the evaluation of a patient with hypothyroidism. For nuclear imaging, scans using radioactive iodine isotopes are most preferred, because these directly reflect the active accumulation (trapping) of iodine by the thyroid follicular cell and covalent attachment (organification) of iodine to thyroglobulin.
The preferred radionuclide for diagnostic nonthyroid cancer imaging is 123 I, because this isotope emits only gamma rays that pass through tissue without significant cellular damage. In contrast, 131 I emits both gamma rays for imaging, as well as damaging beta particles, and is thus used for the treatment of hyperthyroidism and thyroid cancer to destroy iodine-avid thyroid tissue. For diagnostic imaging, 123 I is administered orally with the measurement of iodine uptake and gamma scintigraphy images obtained 4 and/or 24 hours later. Measured thyroidal uptake depends on the activity of NIS and overall iodine status as determined by the amount of circulating nonradioactive iodine. When there is an excess of nonradioactive iodine, the measured radioactive iodine uptake is reduced due to the competition between radioactive and nonradioactive iodine uptake by the thyroid follicular cells. Sources of excess nonradioactive iodine include kelp, seaweed, seafood, iodine-rich medications and agents (amiodarone, saturated solution of potassium iodide [SSKI], Lugol’s solution, povidone iodine, tincture of iodine, iodoform gauze), and radiographic contrast media used commonly in computed tomography (CT) scans and gallbladder studies.
An alternate radionuclide is technetium 99m pertechnetate ( 99m Tc), which is administered intravenously. Images are obtained much more rapidly than 123 I, usually on the order of 30 to 60 minutes after the administration of the radionuclide tracer. Although 99m Tc will be trapped by the thyroid follicular cells, there is no iodine moiety for attachment to thyroglobulin, and therefore does not as accurately mimic the thyroidal uptake of iodine as radioiodine nuclides. Thus 123 I thyroid scans have 5% to 8% fewer false negative results than 99m Tc scans. However, because 99m Tc scans are easier, faster, more readily available and less expensive to perform, they have largely replaced 123 I scans at some institutions. Studies of direct comparison of radioiodine and 99m Tc thyroid scans have been highly concordant in patients without nodules and in those with cold nodules. One study reported that of 273 patients with thyroid nodules, only two had increased uptake with pertechnetate and no uptake with radioiodine. However, if the results of the 99m Tc scan are not in agreement with the clinical picture, an 123 I scan should be performed.
Although nuclear scans are useful in the differential diagnosis of biochemical hyperthyroidism, other radiologic modalities (e.g., ultrasonography, CT, and magnetic resonance imaging [MRI]) provide information regarding structural anatomy of the thyroid and provide no functional data. The primary role of thyroid ultrasound is in the initial evaluation of thyroid nodules, as recommended by the American Thyroid Association and the American Association of Clinical Endocrinologists. Although thyroid ultrasound does not have a role in the initial evaluation of biochemical thyroid dysfunction, it may demonstrate changes that are consistent but are not necessarily diagnostic of chronic lymphocytic thyroiditis, subacute granulomatous thyroiditis, and postpartum thyroiditis. Some individuals with subclinical hypothyroidism and sonographic features suggestive of chronic thyroiditis are at significant risk for developing overt hypothyroidism requiring thyroid hormone replacement therapy.
Commons signs and symptoms of hypothyroidism ( Box 3.1 ) are mostly nonspecific, and some patients may not display any signs or symptoms. Symptoms may be insidious, and in the elderly and middle-aged women, nonspecific complaints may be interpreted as signs of normal aging or depression. Symptoms of hypothyroidism depend on the degree and duration of the disease but most frequently include weight gain, fatigue, constipation, and menstrual irregularities/infertility.
Weight gain
Fatigue
Cold intolerance
Hyponatremia
Hypothermia
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here