Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
FNAB has tremendous utility as first interventional diagnostic procedure relative to a patient with a thyroid mass.
Diagnostic sensitivity and specificity of FNAB of a thyroid mass is high.
In many situations, surgical removal is treatment for a thyroid mass lesion irrespective of diagnosis by FNAB.
FNAB may result in a number of histologic changes in resected thyroid gland that may create diagnostic challenges:
Histologic alterations caused by FNAB may lead to an erroneous diagnosis, such as changing interpretation from a benign process to a malignant one.
Pathologists must be aware of diversity of changes that may occur induced by FNAB.
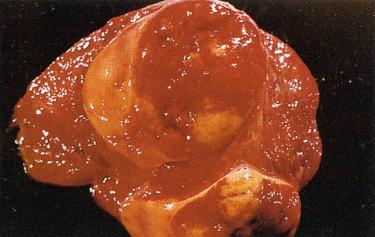
Post-FNAB histologic changes occur in numerous lesions, including adenomatoid nodules, hyperplastic lesions, follicular adenoma and its variants, follicular carcinoma and its variants, and papillary carcinoma and its variants.
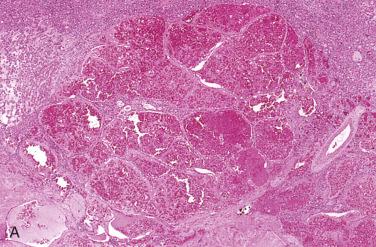
Oncocytic (oxyphilic) cells may be present in a wide variety of thyroid lesions (e.g., adenomatoid nodules, follicular adenoma, follicular carcinoma, papillary carcinoma, others) and are more prone to retrogressive changes secondary to a traumatic event such as FNAB owing to prominence of oxygen-sensitive mitochondria in these cells:
Any compromise to oxygen supply of oncocytic cells may result in retrogressive changes, including:
Cyst formation, papillary architecture, hemorrhage, infarction
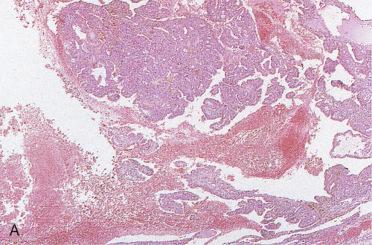
Based on type of reaction seen post-FNAB alterations may include acute or chronic type changes:
Acute changes usually identified within 3 weeks from FNAB to surgical removal and may include:
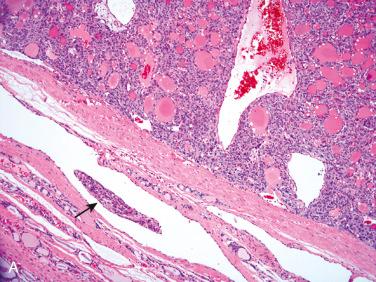
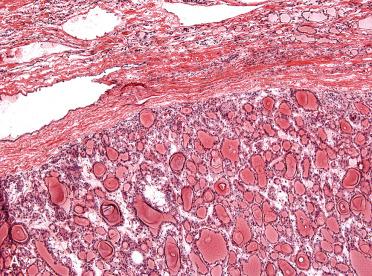
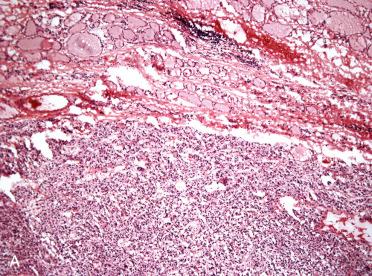
Hemorrhage with hemosiderin-laden macrophages and granulation tissue:
Represent most common findings:
Localized follicular destruction
Capsular alterations
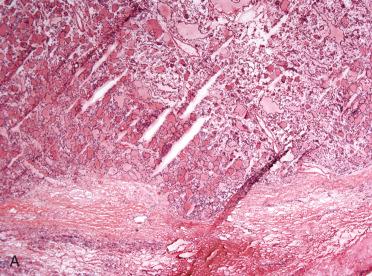
Atypical cytologic features with necrosis and mitoses:
Nuclear atypia is reactive or reparative, typically occurs near the needle tract, and includes nuclear enlargement (nucleomegaly), hyperchromasia, prominent nucleoli
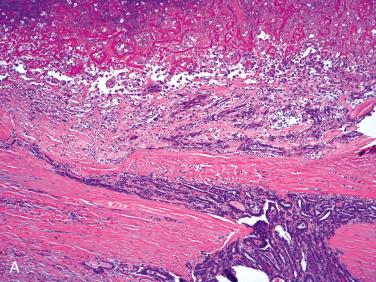
Chronic changes usually identified more than 3 weeks from FNAB to surgical removal and may include (individually or in combination):
Metaplasia:
Squamous or oncocytic cells
Mucous cell may uncommonly be identified.
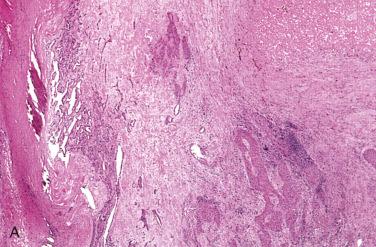
Infarction
Nuclear atypia, including nucleomegaly, hyperchromasia, and prominent nucleoli
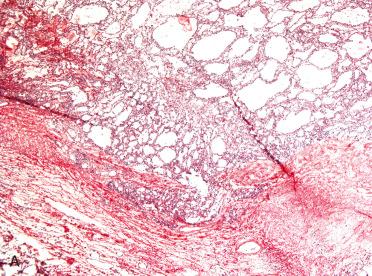
Cyst formation
Papillary architecture
Fibrosis
Calcifications
Hemorrhage (recent and remote in form of hemosiderin-laden macrophages) and/or cholesterol granuloma formation
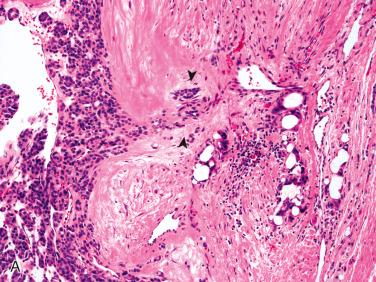
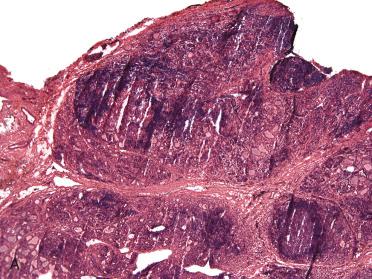
Capsular alterations with pseudoinvasive growth and/or epithelial displacement:
May take the form of a needle tract in which there is a linear-appearing “bud” into fibrous capsule
Low magnification appearance suggests capsular invasion, but at higher magnification follicular epithelium does not violate capsule.
Rather, needle tract composed of dense fibrosis as well as chronic inflammatory cells infiltrate including macrophages and giant cells with or without hemorrhage (recent and remote, latter in form of hemosiderin deposition); cholesterol granuloma formation may be present.
Epithelial displacement
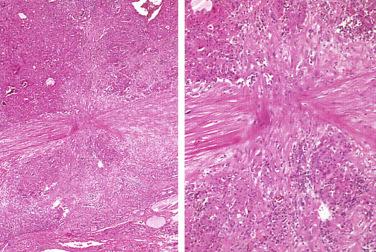
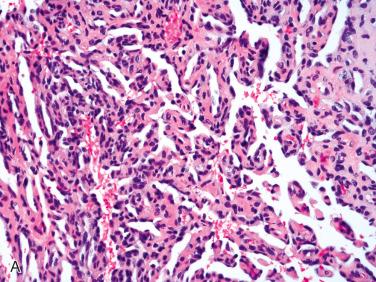
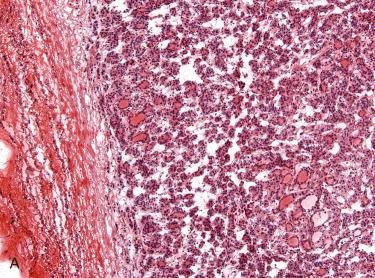
Vascular alterations, including:
Dilated vascular spaces with thrombosis, organization, papillary endothelial hyperplasia (Masson tumor-like reaction), and endothelial cell atypia:
May suggest presence of a vascular tumor such as hemangioma or even an angiosarcoma
Temporal sequence from the FNAB to surgical removal is an important factor in the interpretation of these findings.
Artifactual implantation or “invasion” of tumor cells within endothelial-lined space:
In this setting, cells float within vascular lumens and are not adherent to vessel wall and/or have associated fibrin thrombus formation as seen in true vascular invasion.
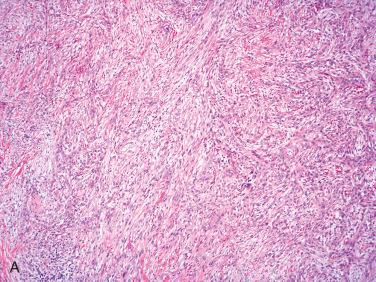
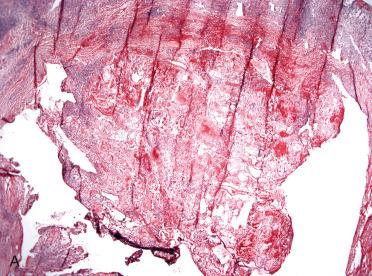
Reparative changes may be exuberant, including spindle-shaped cells (fibroblasts) that may simulate a sarcoma and have been referred to as post-FNAB spindle cell nodule.
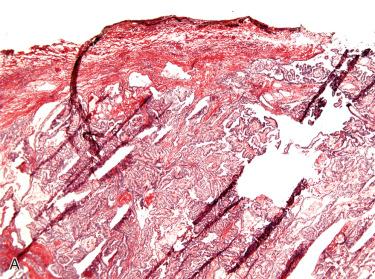
Needle tract tumor implantation :
Rare occurrence
Reported in association with papillary thyroid carcinoma
Intervals between FNAB and detection of implantation range from 2 to 131 months
Location of carcinoma cells in line of needle insertion include:
Subcutis
Within strap muscles
None of the lesions included lymph node components on pathology.
Implanted tumors surgically removed without recurrence at focal sites

Most effective in cases in which fine-needle aspiration biopsy (FNAB) results are suspicious for malignancy (Bethesda V)
Render a histologic diagnosis.
Differentiate a benign lesion (e.g., adenomatoid nodule[s], adenoma) from a malignant neoplasm that may require additional surgery (i.e., total or near total thyroidectomy).
Identification of nonsentinel nodal metastasis:
Role of sentinel lymph node sampling not established for thyroid tumors
Incisional biopsy with intraoperative consultation (IOC) may occur:
In patients with unresectable disease (e.g., undifferentiated [anaplastic] carcinoma)
To ensure adequacy for diagnosis in certain clinical settings (e.g., unresectable disease) or in relationship to certain tumor types (e.g., hematolymphoid tumors)

Establish a correct diagnosis.
Differentiate a benign (non-neoplastic or benign tumor) from a malignant tumor.
Identification of nodal metastasis in cases in which lymph nodes are resected and sent for IOC
Identify additional findings that may affect treatment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here