Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Thrombolytic therapy for venous thromboembolism is an increasingly important option for the management of patients with extensive venous thromboembolic disease, namely iliofemoral venous thrombosis and pulmonary embolism (PE), which alter venous and cardiopulmonary hemodynamics and cause pathologic myocardial stretch or cellular damage. This chapter addresses those patients. Specifically, in patients with deep venous thrombosis (DVT), iliofemoral DVT (IFDVT) is associated with the most severe acute and long-term postthrombotic sequelae.
Patients with massive PE defined by sustained hypotension and those with submassive PE characterized by right heart strain are those who would benefit most by eliminating the acute obstruction of right ventricular outflow.
There is a common theme in treating both extensive venous thrombosis and large pulmonary emboli, and that is restoring hemodynamics. In the lower extremity the goal is to avoid venous hypertension (ambulatory venous hypertension), and in the cardiopulmonary circulation the goal is to correct cardiopulmonary hemodynamics and avoid chronic thromboembolic pulmonary hypertension.
The postthrombotic morbidity of IFDVT treated with anticoagulation is illustrated by a 22-year-old woman who was referred with severe venous claudication. As a high school student, this patient was the state champion in the 400-m and 800-m run. She was awarded a full college scholarship as a member of a Big Ten women's track team. Three months after starting birth control pills, she developed an extensive iliofemoral venous thrombosis. She was hospitalized, treated with low-molecular-weight heparin (LMWH) and converted to warfarin. Her leg remained swollen and her venous claudication persisted. Her symptoms limited her activity; she could no longer participate as a member of the track team and had difficulty with sustained walking. She lost her athletic scholarship and, because of family finances, could not remain in college. The result was a part-time job paying minimum wage. Her IFDVT with its postthrombotic sequelae irrevocably changed her life and the life of her future family.
Acute obstruction of the single channel outflow from the lower extremity (common femoral, external iliac, and common iliac veins) leads to high compartment and venous pressures. Qvarford and colleagues reported compartment pressures in patients presenting with IFDVT who subsequently underwent venous thrombectomy. Upon presentation, these patients had high compartment pressures, which is a surrogate for venous pressure. Following thrombus removal and restoration of venous outflow, compartment pressures significantly decreased and returned to normal in many.
The pathophysiology of chronic venous disease is venous hypertension, specifically ambulatory venous hypertension. Venous valve function and luminal obstruction are the two main components leading to ambulatory venous hypertension. However, it is this author's opinion that obstruction is far more important than valvular dysfunction in producing severe venous hypertension and the most debilitating form of chronic venous disease.
Labropoulos and colleagues measured venous pressure and calculated the arm-foot pressure differential in patients with the spectrum of postthrombotic venous disease; they showed that patients with postthrombotic obstruction of the iliofemoral venous system had the highest venous pressures (highest arm-foot pressure differential), which translates into clinical morbidity.
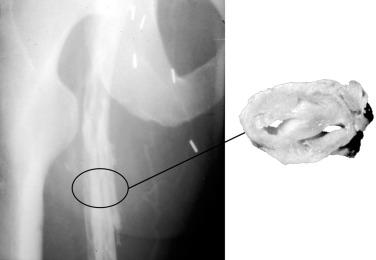
Anticoagulation alone for IFDVT reduces the risk of pulmonary embolization and reduces the extension of thrombus. Unfortunately, obstruction of the venous outflow channel remains, producing significant venous hypertension. Fig. 50.1 is a photograph of a man who had IFDVT treated with anticoagulation alone 3 months earlier. Despite therapeutic anticoagulation and wearing 30- to 40-mm ankle-gradient compression stockings, he suffered with venous claudication, swelling of the lower extremity, and skin discoloration in the lower leg, with the ascending phlebogram showing extensive deep venous obstruction. Another ascending phlebogram ( Fig. 50.2 ) of a patient with severe postthrombotic morbidity and venous ulceration 10 years after anticoagulation alone for IFDVT shows chronic recanalization but understates his venous obstruction. The day following the phlebogram, the patient underwent a classic Linton procedure. The operative photograph of a cross section of his postthrombotic femoral vein demonstrates the fibrotic obstruction with multiple, small channel recanalization which occur in these patients, causing much more obstruction to venous return than can be appreciated on the phlebogram.

Natural history studies of patients with acute DVT treated with anticoagulation alone have revealed a number of important principles. Meissner and colleagues followed patients with acute DVT with sequential venous duplex examinations. Some patients' thrombus was lysed during the first few months of follow-up, whereas in others the thrombus persisted. When thrombus lysed early (within 60 to 90 days), patients were likely to retain normal valve function. However, in patients whose thrombus did not lyse, valve reflux occurred. In longer-term follow-up studies, patients who had persistent thrombus had a significantly higher risk of recurrent DVT.
Acute DVT of the lower extremity includes a spectrum of clinical presentations ranging from asymptomatic isolated calf vein thrombosis to severely symptomatic extensive IFDVT. Cumulative evidence suggests that iliofemoral venous thrombosis is accompanied by more dramatic clinical manifestation, predicts poor immediate and long-term outcomes, and warrants a treatment strategy of thrombus removal. A likely explanation of the underuse of strategies of thrombus removal is the underappreciation of postthrombotic sequelae of extensive proximal venous thrombosis.
Kahn and colleagues performed a prospective analysis of 387 patients with acute DVT. Their intent was to evaluate postthrombotic syndrome following acute DVT. They found that patients with IFDVT had the most severe postthrombotic morbidity (odds ratio [OR] 2.23; P < .001). They also found that the patients' clinical condition at 1 month was the best predictor of long-term outcome ( P < .001).
A number of authors have followed patients with IFDVT who were treated with anticoagulation alone. These patients uniformly suffered with chronic venous disease. Within 5 years, 15% developed venous ulceration and up to 40% had venous claudication. The patients' quality of life (QOL) was significantly diminished.
An observation which is often overlooked is that recurrent DVT is more frequent in patients with IFDVT than in patients with femoropopliteal DVT. This is likely due to the large burden of thrombus resulting in postthrombotic obstruction following anticoagulation alone.
The purpose of this short section is not to address operative venous thrombectomy, which is beyond the scope of this chapter. It is to emphasize the principles of restoring patency, normalizing venous pressures, and long-term benefits are well illustrated by the randomized trial performed by Plate and colleagues. The Scandinavian investigators randomized patients with IFDVT to venous thrombectomy plus arteriovenous fistula (AVF) followed by anticoagulation or anticoagulation alone. A careful follow-up at 6 months, 5 years, and 10 years demonstrated significant benefits in those patients who underwent venous thrombectomy. Patients randomized to thrombectomy had improved patency, lower venous pressures, less leg swelling, and fewer postthrombotic symptoms compared with anticoagulation alone. These data illustrate the benefit of eliminating obstruction to venous drainage from the leg to the vena cava. The details of contemporary operative venous thrombectomy have been reviewed by Comerota and Gale.
A report by Rodriguez described a novel technique called hybrid open thrombectomy (HOT). The method uses a single surgical access to the common femoral vein to remove thrombus from the iliofemoral venous segment. The same access is used to clear more distal segments, including tibial veins, by means of careful retrograde manipulation with a guidewire followed by balloon catheter thrombectomy. Technical success comparable with pharmacomechanical thrombolysis was achieved in 38 patients.
All drugs currently used for thrombolytic therapy are plasminogen activators. That means that clot dissolution occurs as a result of plasminogen being activated, resulting in the production of plasmin, which is the active clot dissolving enzyme.
Systemic thrombolytic therapy is an inefficient method of treating acute DVT. A relatively small amount of systemically infused plasminogen activator will contact the thrombus to activate fibrin-bound plasminogen. The results of studies evaluating systemic thrombolytic therapy for acute DVT have been disappointing and generally are associated with higher than acceptable bleeding complications and lower than acceptable success rates. It is understandable that techniques that deliver the plasminogen activator into the thrombus, thereby maximally activating fibrin-bound plasminogen and minimizing the systemic delivery of the plasminogen activator will be associated with greater success rates and fewer bleeding complications.
Numerous reports have demonstrated good outcomes of catheter-directed thrombolysis (CDT) for acute DVT. Most of these reports (≥20 limbs) are listed in Table 50.1 , which also includes pharmacomechanical techniques used as adjuncts to CDT. In general, when patients with acute DVT are treated with catheter-based techniques, success rates in the range of 75% to 90% can be anticipated. The rate of bleeding complications ranges from 5% to 11%. Fortunately, serious distant bleeding is uncommon and intracranial bleeding is a rarity. Most bleeding complications are localized to the venous access site, and reports surfacing in the past 7 years generally report bleeding complications as 5% or less. Symptomatic pulmonary embolization during infusion is uncommon and fatal PE a rarity.
The National Venous Registry reported a large cohort of patients treated with lytic therapy for acute DVT. Seventy-one percent of these patients had IFDVT, and 25% had femoropopliteal DVT. It is interesting to note that patients with IFDVT seem to have had better and more durable results than patients with femoropopliteal DVT.
Patients treated in the National Venous Registry were treated with intrathrombus infusion of urokinase via CDT. In the group with acute first-time IFDVT, 65% had complete clot resolution. There was an important correlation ( P < .001) of thrombosis-free survival with the results of initial therapy. At 1 year, 78% of patients with initially complete clot resolution had patent veins and only 37% of patients who had less than 50% lysis. In the patients with first-time IFDVT who initially had successful thrombolysis, 96% of the veins remained patent at 1 year. Initial lytic success also correlated with valve function at 6 months. Thirty-eight percent of patients with less than 50% thrombolysis had normal valve function, whereas 72% with complete lysis retained normal valve function ( P < .02).
A cohort-controlled QOL study was performed to assess whether lytic therapy impacted QOL in patients with IFDVT. Patients with IFDVT treated by CDT were compared with a contemporaneous cohort of patients with IFDVT from the same institutions who were treated with anticoagulation alone. All patients treated with anticoagulation alone were candidates for lytic therapy; however, the choice of treatment was determined by physician preference. Patients were evaluated with a validated QOL questionnaire, with patients queried at 16 and 22 months following acute treatment. Ninety-eight patients were evaluated, 68 of whom were treated with CDT and 30 with anticoagulation alone. CDT was associated with better QOL than anticoagulation alone. QOL was directly related to thrombolytic success. Patients who had a successful lytic outcome reported a better Health Utilities Index, improved physical functioning, less stigma of chronic venous disease, less health distress, and fewer postthrombotic symptoms. Not surprisingly, patients in whom CDT failed had outcomes similar to those treated with anticoagulation alone. A subsequent single-center observational study demonstrated that QOL following CDT for IFDVT directly correlated with success of clot lysis.
A small randomized trial performed by Elsharawy and colleagues compared CDT with anticoagulation alone. CDT resulted in significantly better patency and valve function at 6 months. Enden and colleagues reported the results from a randomized trial of CDT and anticoagulation versus anticoagulation alone for IFDVT. Patients treated with CDT had better patency of the iliofemoral system which directly correlated with less postthrombotic morbidity than those treated with anticoagulation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here