Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Aortopexy is indicated in young patients with life-threatening tracheal obstruction secondary to severe tracheomalacia. The tracheomalacia may be primary or secondary. The secondary form is often seen in combination with esophageal atresia (EA) and vascular rings. It has also been described in combination with congenital heart disease. Symptoms vary from mild and not requiring therapy, to severe and not allowing extubation, to producing acute life-threatening events (ALTEs). Randomized controlled trials regarding the different treatment modalities do not exist. Continuous positive airway pressure ventilation is occasionally effective but is not a viable long-term therapy. Bronchial stenting has not gained popularity because of its high failure rate and sometimes more severe morbidity and mortality.
Aortopexy is a relatively straightforward operation that results in immediate relief of symptoms in about two-thirds of cases. There is little doubt that this approach is the treatment of choice in severely symptomatic infants. Moreover, the thoracoscopic technique is much less traumatic than other operative approaches, such as left thoracotomy or a low cervical–upper sternotomy approach.
Aortopexy is indicated in cases of life-threatening apnea due to tracheomalacia. In infants with severe symptoms, once this diagnosis is made, not much time should be lost before the procedure is performed.
The diagnosis of tracheomalacia is made on clinical grounds and confirmed by tracheobronchoscopy. A lateral chest radiograph can sometimes show the narrowed trachea in the thoracic aperture. In children with EA and distal fistula, clinical tracheomalacia can be documented in almost all babies. However, only a small percentage require aortopexy. Tracheomalacia can also be seen in babies with aortic arch anomalies.
We prefer to perform rigid tracheobronchoscopy under general anesthesia, but with the patient spontaneously breathing to thoroughly evaluate and control the airway. This should be done prior to determining if the child needs an aortopexy. Moreover, a flexible bronchoscope is generally used during the procedure to determine the effectiveness of the aortopexy.
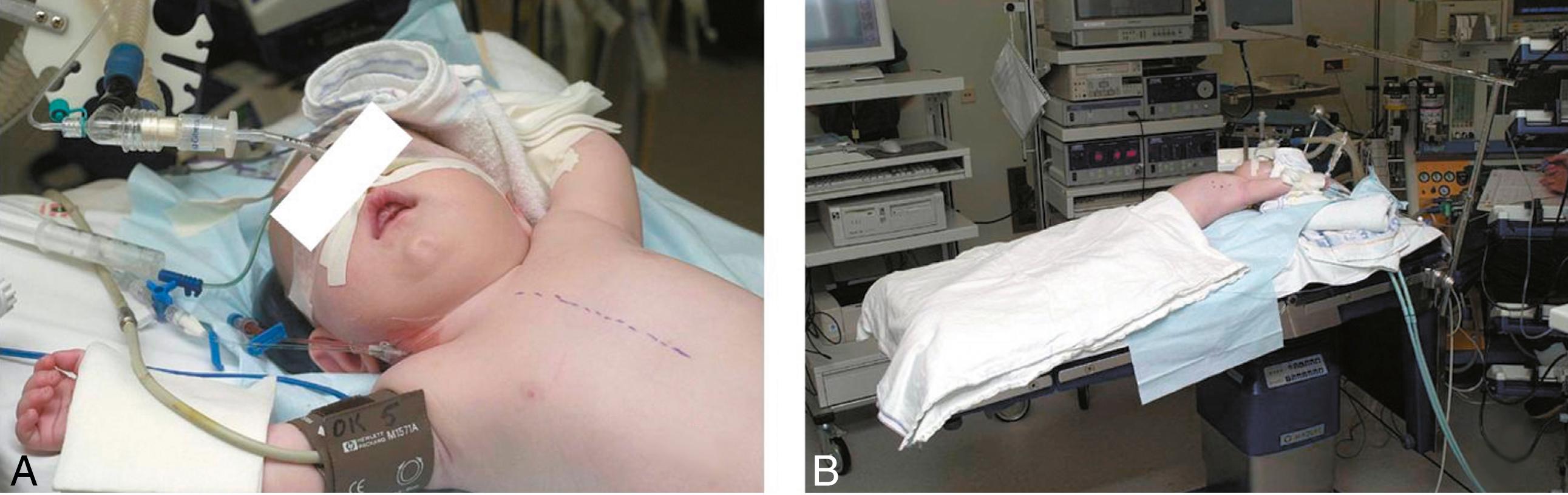
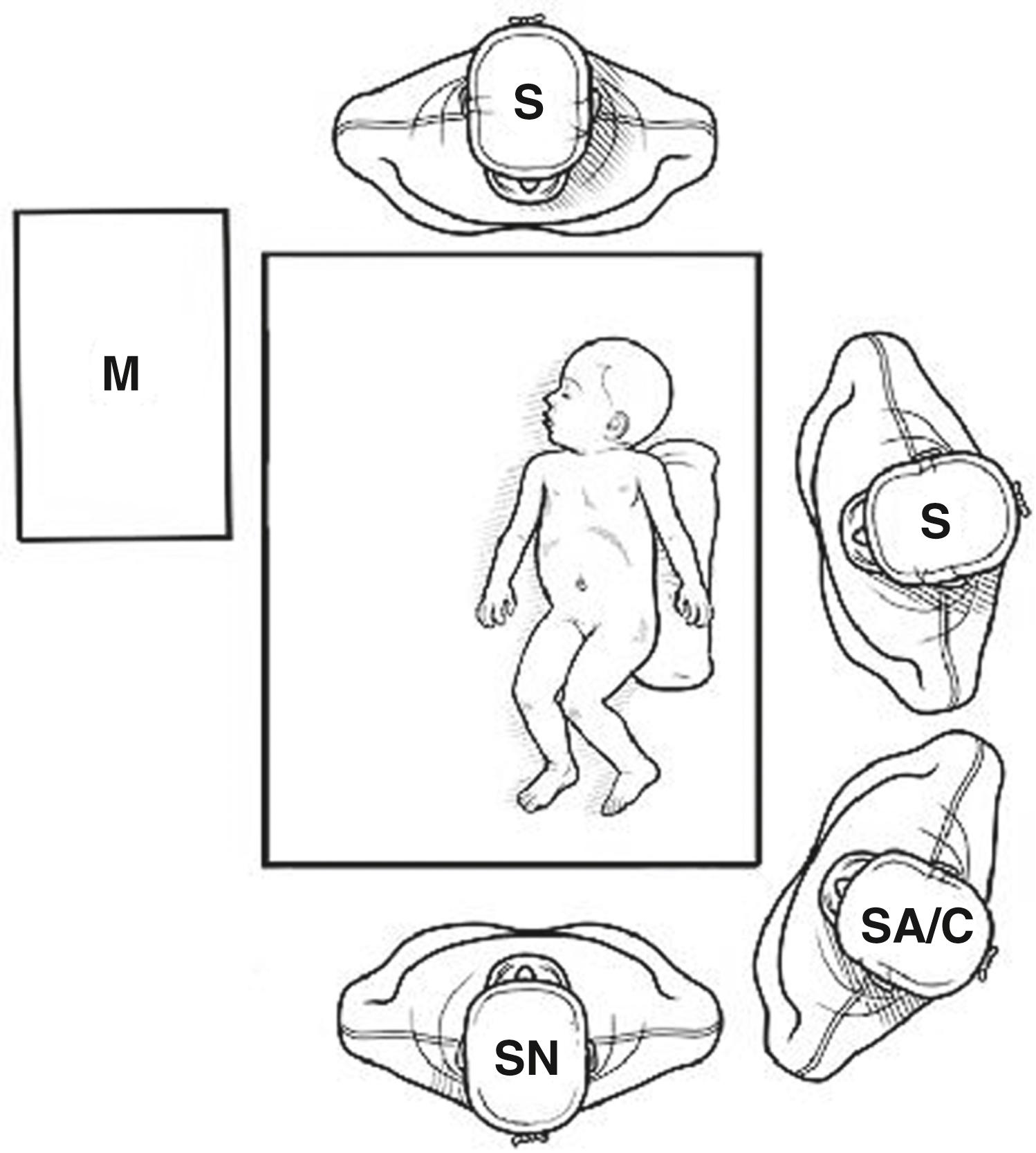
The young patient is placed supine on the operating table. The midsternal line is marked on the skin ( Fig. 38-1A ). The left chest is elevated about 15 degrees, and the operating table is tilted in reverse Trendelenburg ( Fig. 38-1B ). The surgeon stands to the left of the patient with the camera operator on the surgeon’s left and the scrub nurse at the caudal end of the short operating table ( Fig. 38-2 ). The most important monitor is positioned in front of the surgeon, at the right side of the patient. The equipment tower is placed behind the surgeon or on the right side of the table, adjacent to the monitor.
The procedure is usually performed with standard tracheal intubation, using CO 2 insufflation to collapse the lung and create adequate working space. This also allows for the placement of a flexible bronchoscope through the endotracheal tube during the procedure to evaluate the success of the aortopexy. A right mainstem intubation can be used, but the tube would need to be pulled back at the time of bronchoscopy for evaluation of the aortopexy.
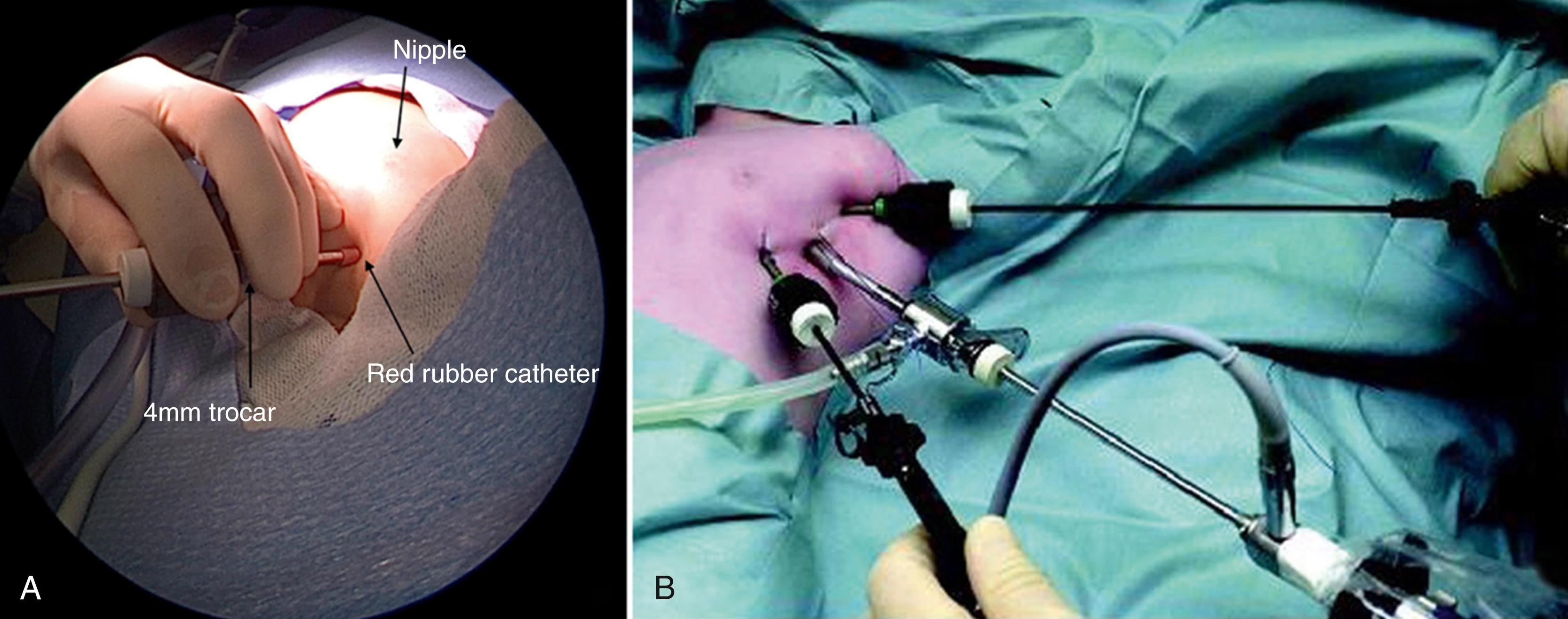
The procedure is started by inserting a Veress needle in the fourth or fifth intercostal space in the anterior axillary line (roughly at the level of the nipple). A low-flow (1 L/min) and low-pressure (6 mm Hg) CO 2 insufflation are used to create a mild tension pneumothorax to collapse the lung. The first port, a 4-mm cannula, is inserted at this site. A piece of red rubber catheter is placed on the cannula and sutured to the skin to prevent slippage ( Fig. 38-3A ). A 4-mm 30-degree lens is then introduced through this port. A 5-mm port and scope can also be used per surgeon preference. If necessary, the insufflation pressure can be increased to 8 mm Hg to achieve adequate lung collapse. Next, the two working ports are inserted, one 3-mm port for the surgeon’s left hand and a 5-mm radially expandable cannula for the right hand. The surgeon’s left-hand port is one interspace lower and more medial, and the right hand port is placed two to three interspaces higher in the axilla ( Fig. 38-3B ). The working angle between the ports should be about 60 to 90 degrees. These cannulas can also be secured to the chest wall to prevent dislodgment.
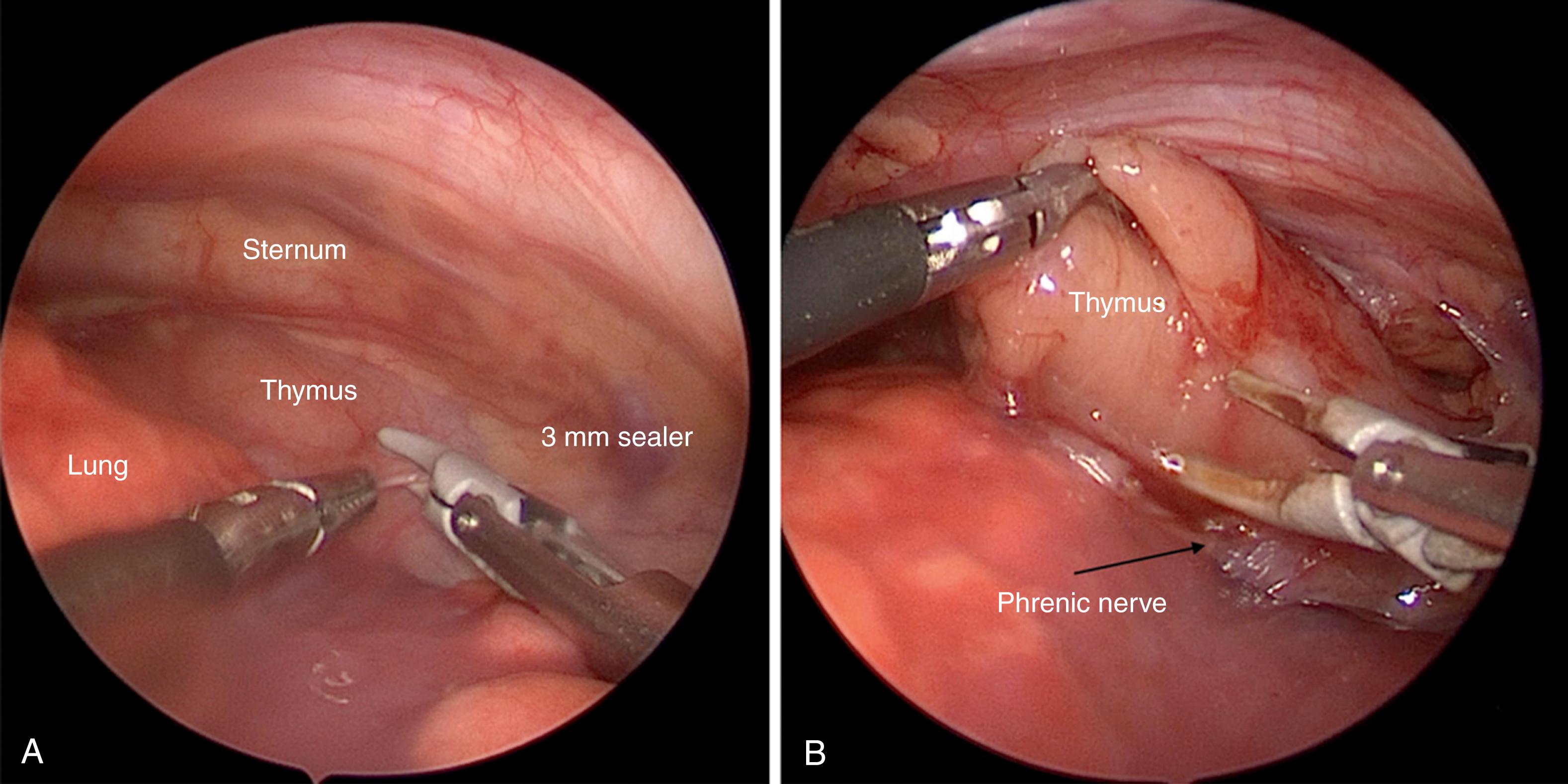
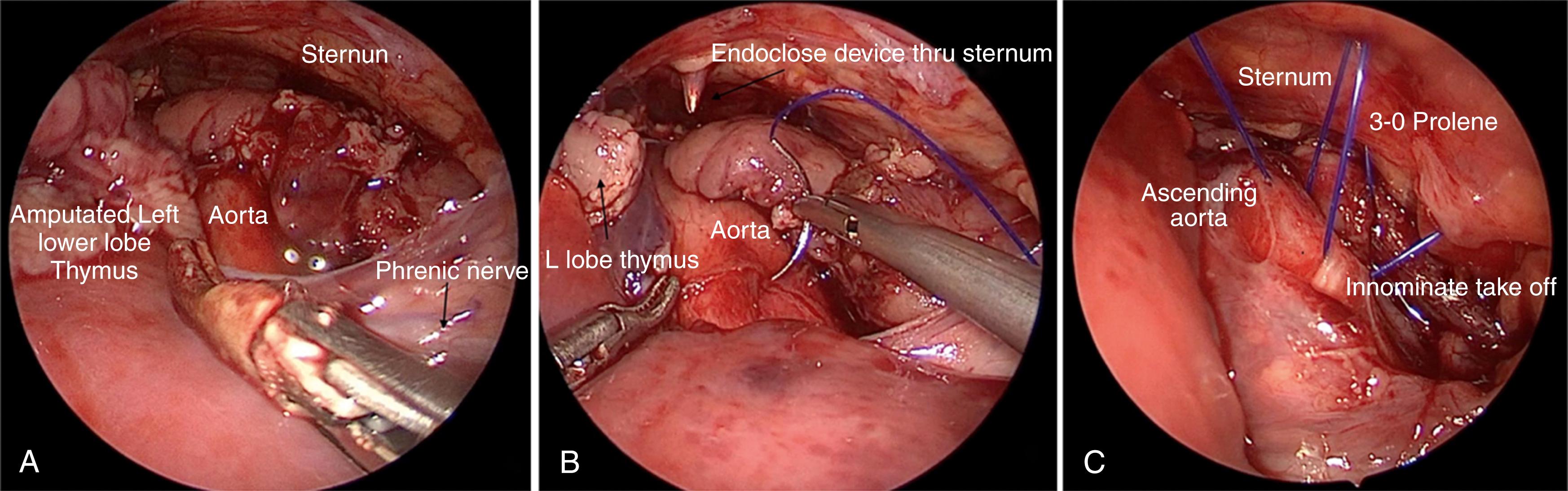
The initial dissection involves mobilization and removal of the left lobe of the thymus. This is generally accomplished through an avascular plane, with the anterior boundary being the internal mammary vessels, and the posterior boundary being the phrenic nerve ( Fig. 38-4A ). Great care is taken not to injure the phrenic nerve. The pleura is opened near the inferior border of the thymus using the 3-mm vessel sealer (Bolder Surgical, Louisville, CO), and a plane is developed along the lateral border, protecting the phrenic nerve at all times by being anterior and medial to it. Electrocautery should be avoided in this area. We prefer to excise the left thymic lobe, leaving a portion of the upper horn and isthmus to avoid bleeding from the thymic vessels. The thymus can also be mobilized posteriorly until the ascending aorta, with its pericardial reflection, and the innominate artery are seen ( Fig. 38-5A ). The aortic arch itself is also seen but is not dissected. The thymus can now be mobilized anteriorly and pushed into the right hemithorax. At the end of the operation, the thymic lobe can be removed piecemeal through one of the 5-mm incisions.
In most cases, we open the upper pericardium to expose the ascending aorta. However, the sutures can also be placed through the pericardium into the aortic wall if the surgeon prefers.
The most difficult part of the operation is placement of the three or four 3-0 Prolene sutures (Ethicon, Somerville, NJ) in the aortic wall, followed by exteriorization of the sutures. Because it is important to have a sharp needle to pass through the wall of the aorta, we pass these sutures into the mediastinum through the 5-mm accessory cannula one at a time. In infants, the sutures can also be inserted through the intercostal space adjacent to the sternum without risk of dulling the needle. A series of stitches are then placed in the aortic wall (primarily in the adventitia) on the ascending aorta, the arch, and the takeoff of the innominate artery ( Figs. 38-5B and 38-5C ). The sutures are then exteriorized, one end through the body of the sternum, and one end through the adjacent intercostal space. Exteriorization of this latter tail can be aided by making a 5-mm incision at the lateral border of the sternum at the level of the second intercostal space and slightly undermining the subcutaneous tissue. An Endo-Close device (Medtronic, Minneapolis, MN) ( Fig. 38-4B ) (depending on the size of the baby) can be passed through the sternum to catch one end of the suture and then introduced through the intercostal space adjacent to the sternum to deliver the other end. Each stitch is brought out in a slightly different space to spread out the tension. As each suture is exteriorized, it is secured with a hemostat. When all three or four sutures are exteriorized, traction is placed on all sutures at the same time, elevating the aorta off the trachea. At this point, the bronchoscope is inserted to evaluate the efficacy of the aortopexy. If adequate elevation is seen, the sutures are then tied extracorporeally. The knots are anterior to the sternum and are secured in the soft tissue under the small 5-mm incision. If elevation of the aorta is inadequate, another suture is placed, usually in the area of the aortic arch. The left lobe of the thymus is grasped with an instrument in the 5-mm cannula in the upper axilla and is removed in segments.
The CO 2 insufflation is stopped, and the stopcock on the 5-mm cannula is opened to evacuate the pneumothorax. The lung is then actively expanded by the anesthesiologist. The ports are removed and the port sites are closed with absorbable sutures ( Fig. 38-6 ). We do not usually leave a chest tube for these procedures. A chest radiograph is obtained in the postanesthesia care unit.

When the operation is successful, the effect is almost immediately evident.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here