Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The management of neurogenic thoracic outlet syndrome (nTOS) requires a comprehensive, multidisciplinary approach, including a prominent role for surgical treatment in well-selected patients. Establishing the diagnosis can be challenging, and disappointing results of treatment have led some authorities to question the need for surgical management of nTOS, and even to challenge whether the condition actually exists (see Ch. 123 : Thoracic Outlet Syndrome: Pathophysiology and Diagnostic Evaluation). The purpose of this chapter is to review current understanding of the diagnosis, optimal management, and surgical techniques for nTOS.
As shown in Figure 124.1 , the anatomy of the thoracic outlet is composed of several bony and soft tissue structures, as well as nerves and blood vessels which traverse the space.
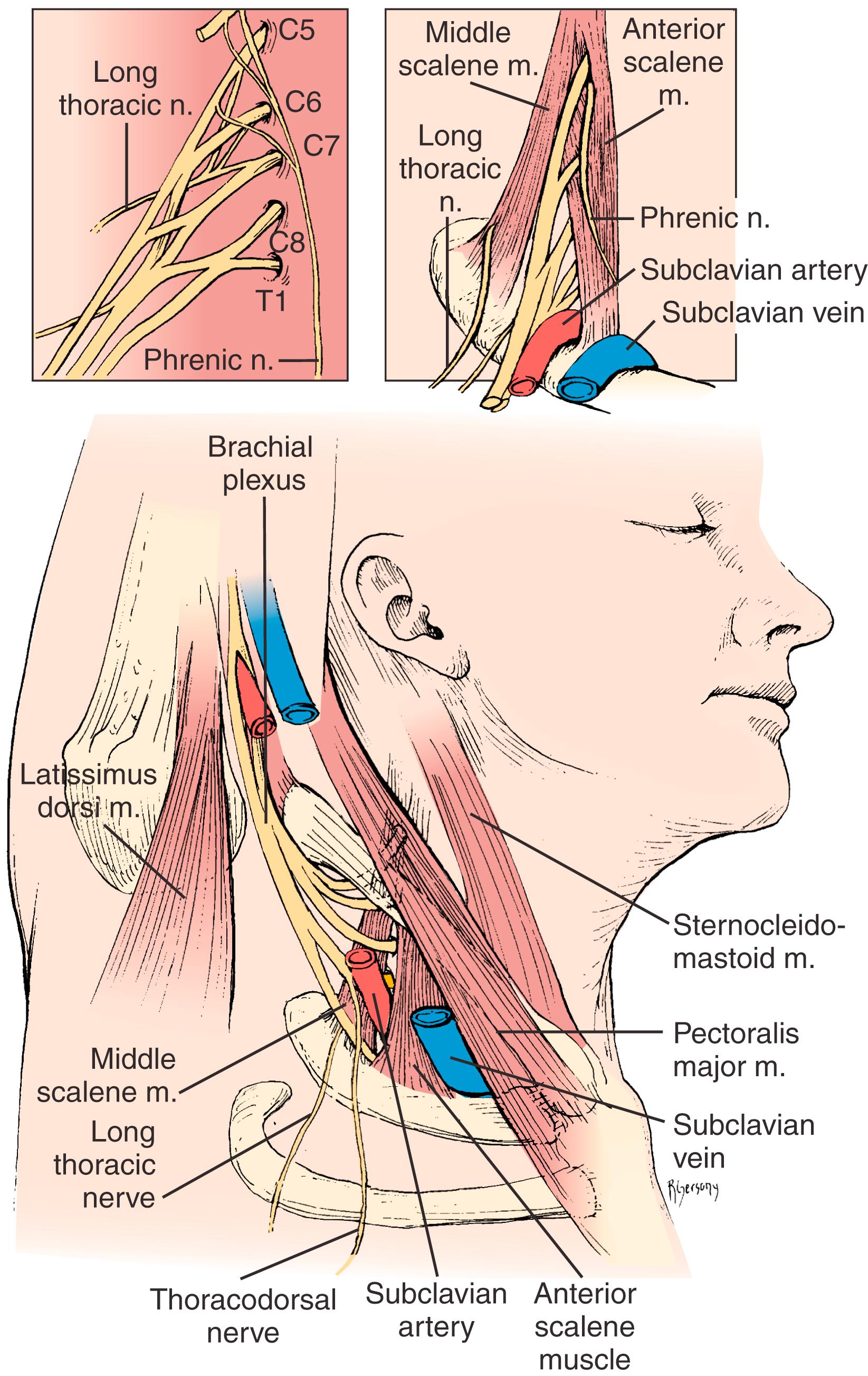
The scalene triangle is traversed by the brachial plexus , organized into three trunks: the upper trunk (formed by the fused C5 and C6 nerve roots), the middle trunk (composed of the C7 nerve root), and the lower trunk (formed by fusion of the C8 and T1 nerve roots). The phrenic nerve, the long thoracic nerve, and the cervical sympathetic chain also pass through the thoracic outlet. The phrenic nerve passes lateral to medial descending anteriorly along the anterior scalene muscle, and then behind the subclavian vein into the mediastinum to innervate the diaphragm. The long thoracic nerve passes through the middle scalene muscle, where its three components typically fuse into a single nerve, before descending to supply the serratus anterior muscle. The cervicodorsal sympathetic chain lies along the posterior inner aspect of the ribs.
The conventional description of scalene triangle anatomy occurs in no more than one-third of individuals, with several common variations in soft tissue structure. , The most frequent muscular variation is the scalene minimus muscle , which originates within the plane of the middle scalene muscle, passes between various brachial plexus nerve roots and inserts upon the first rib with the anterior scalene muscle. Fascial bands across or between individual nerve roots can exist, attaching to either the first rib or extrapleural fascia. During TOS operations, a dense fascial band crossing over the T1 nerve root origin is commonly encountered. Several other muscular and fascial variations have been described and classified ( Table 124.1 ). ,
| Type 1: | Extending from anterior tip of an incomplete cervical rib to the middle of the first thoracic rib; inserts just posterior to the scalene tubercle on the upper rib surface. |
| Type 2: | Arises from an elongated C7 transverse process in the absence of a cervical rib and attaches to the first rib just behind the scalene tubercle; associated with extension of the transverse process of C7 beyond the transverse process of T1 on AP spine radiographs. |
| Type 3: | Both originates and inserts on the first rib; starts posteriorly near the neck of the rib and inserts anteriorly just behind the scalene tubercle. |
| Type 4: | Originates from a transverse process along with the middle scalene muscle and runs on the anterior edge of the middle scalene muscle to insert on the first rib; the lower nerve roots of the brachial plexus lie against this band. |
| Type 5: | The scalene minimus muscle, arising with the lower fibers of the anterior scalene muscle, runs parallel to this muscle but passes deep to the muscle to cross behind the subclavian artery and in front of or between the nerve roots, and inserts on the first rib; any fibers passing anterior to or between the plexus but posterior to the artery. |
| Type 6: | Scalene minimus muscle inserting onto Sibson fascia over the cupula of the pleura instead of onto the first rib; labeled separately to distinguish its point of insertion. |
| Type 7: | Fibrous cord running on the anterior surface of the anterior scalene muscle down to the first rib, attaching to the costochondral junction or sternum; lies immediately behind the subclavian vein where it may be a cause of partial venous obstruction. |
| Type 8: | Arises from the middle scalene muscle and runs under the subclavian artery and vein to attach to the costochondral junction. |
| Type 9: | Web of muscle and fascia filling the inside posterior curve of the first rib, compressing the origin of the T1 nerve root. |
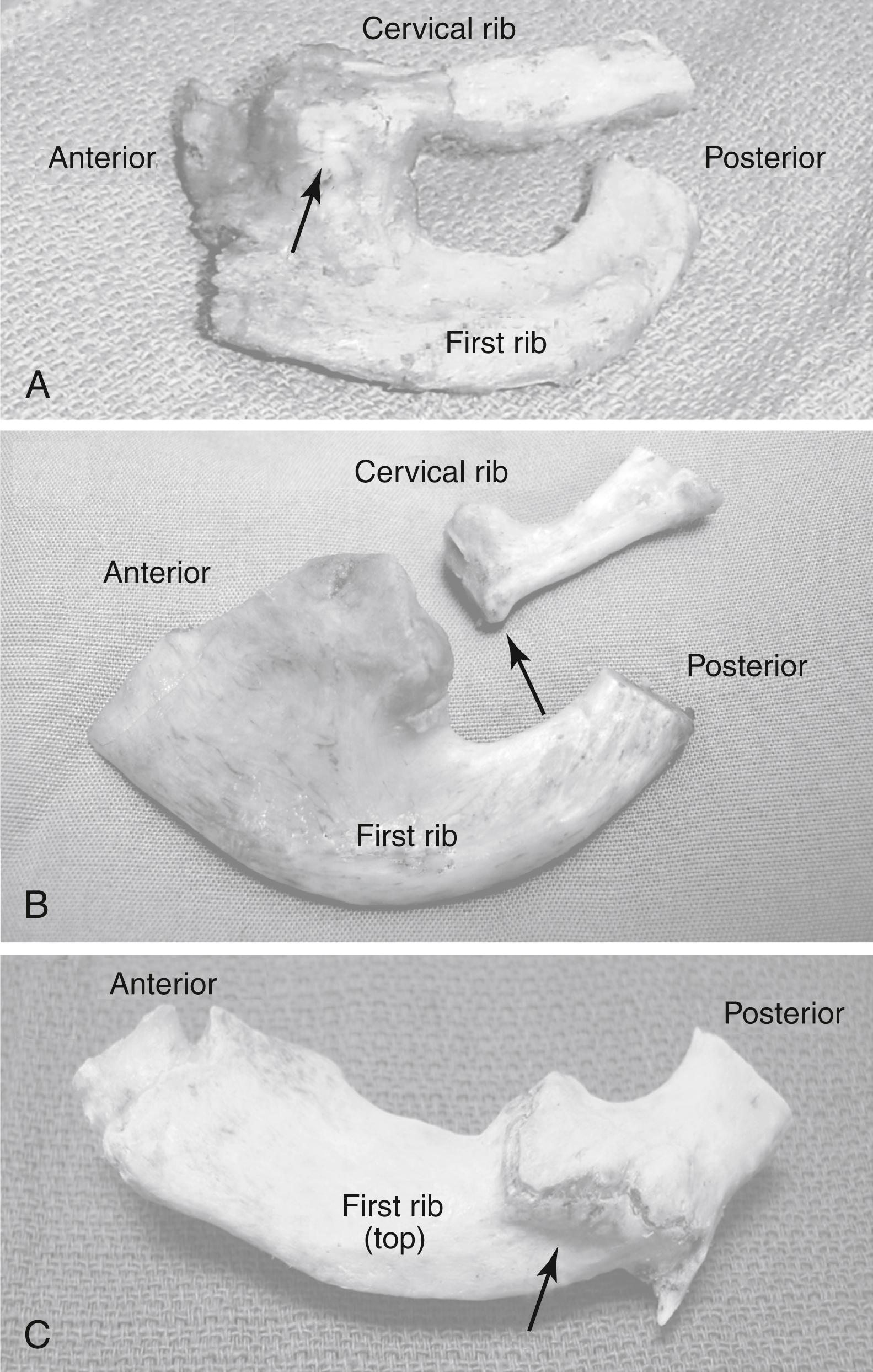
Cervical ribs occur in approximately 0.45%–1.5% of the population and up to 5% of TOS patients. They arise in the plane of the middle scalene muscle and typically attach to the midlateral first rib as an immobile bony fusion or as a fully developed joint ( Fig. 124.2A ). Incomplete cervical ribs arise as bony or cartilaginous extensions from the C7 cervical vertebrae without joining the first rib, and in some cases are attached to the first rib only by a band of cartilage or tendinous tissue ( Fig. 124.2B ). Rudimentary (hypoplastic) first ribs are infrequently recognized, and tend to lie higher in the neck than normal and often insert into the second rib rather than the sternum. Previous trauma may also result in first rib abnormalities, such as fractures with formation of thickened callous at the site of bony healing ( Fig. 124.2C ).
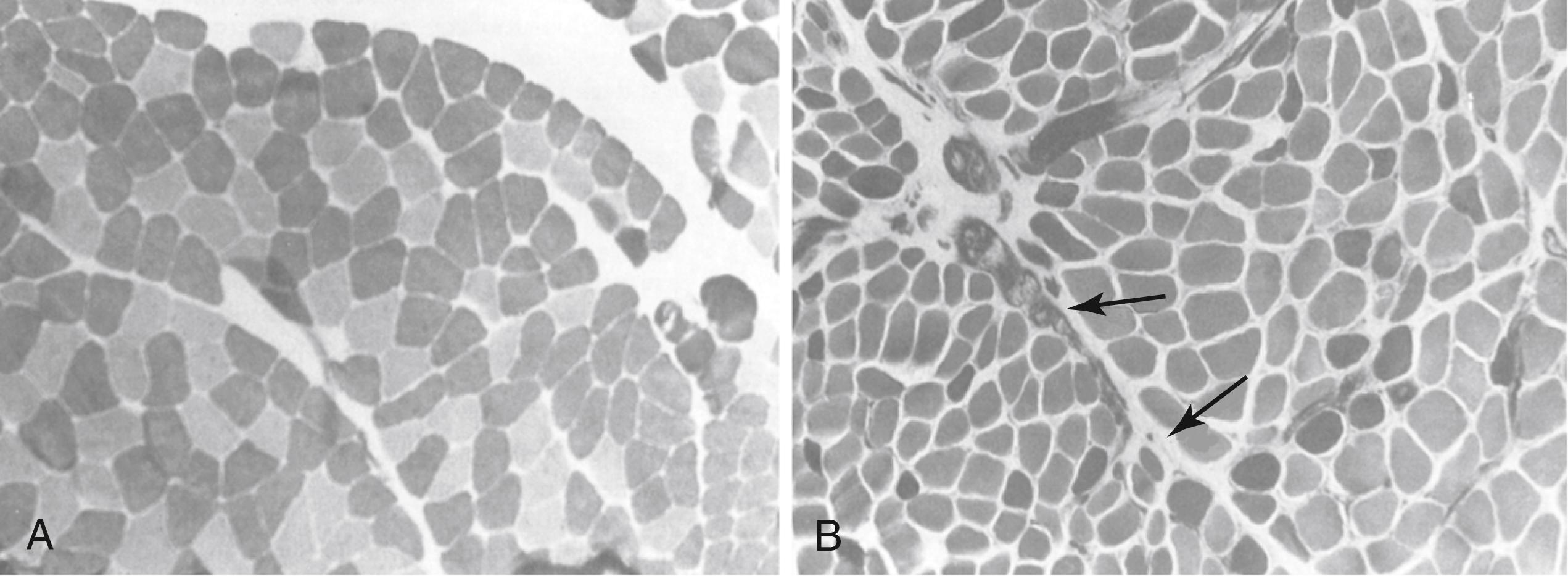
Microscopic studies of scalene muscles from nTOS patients have consistently revealed two major abnormalities: (1) type I muscle fiber predominance and (2) endomesial fibrosis ( Fig. 124.3 ). , Although the anterior scalene muscle normally has an equal distribution of type I (“slow-twitch”) and type II (“fast-twitch”) muscle fibers, type I fibers compose up to 78% of scalene muscle fibers in nTOS patients with associated atrophy and pleomorphism of type II fibers. Additionally, markedly thickened connective tissue matrix surrounds individual muscle fibers, and in some cases there are mitochondrial abnormalities resembling those seen in muscular dystrophy. These histopathologic changes are thought to occur in response to long-standing muscle injury, sustained muscle spasm, and abnormal tissue remodeling, and are therefore consistent with the frequent history of neck trauma in nTOS patients.
Neurogenic TOS is caused by a combination of predisposing anatomical factors and previous neck trauma. Even with normal anatomy, neurovascular structures traversing the thoracic outlet are at risk for compression with regular daily activity. Activities involving sustained or repeated arm elevation or vigorous neck turning may place tension on the scalene muscles, potentiating positional compression of underlying nerve roots. Further anatomic risk factors include congenital structural variants, such as scalene muscle variations, abnormal tendinous bands, or cervical rib anomalies. However, many people without neurogenic symptoms harbor such variations; these variations lower the threshold for, rather than cause, symptom development following injury.
Most nTOS patients describe some form of previous head, neck, or upper extremity trauma, followed by a variable interval of days to weeks before symptom onset. A varying temporal relationship between scalene injury and sustained brachial plexus compression and irritation may obscure recollection of the inciting injury. Persistent upper extremity use in aggravating activities may worsen symptoms and lead to progressive disability, and medical attention is not usually sought until symptoms are advanced. In many cases, injury results from repetitive strain on the scalene muscles from activities such as prolonged computer keyboard use, rather than any single event. Age-related changes in posture (e.g., shoulder slumping and stooping of the neck) may also be significant factors leading to development of extrinsic neural compression.
Neurogenic TOS most frequently occurs between 20 and 40 years of age, and approximately 70% of patients are women. Individuals engaged in a variety of occupational or recreational activities involving heavy lifting or repeated use of the arm(s) in elevated positions may develop nTOS. Patients may also develop nTOS with no apparent anatomical variations or history of trauma. There are no medical conditions or known inherited patterns predisposing to nTOS.
The diagnosis of nTOS rests largely upon clinical pattern-recognition, with diagnostic suspicion raised by a stereotypical history and symptoms. The provisional diagnosis of nTOS is supplemented by physical examination and may be supported by a limited number of diagnostic studies. In most cases such studies are of value primarily in the exclusion of other (more common) conditions within the differential diagnosis. No single diagnostic test has a sufficiently high degree of specificity to completely prove or exclude the diagnosis of nTOS. ,
Primary nTOS symptoms include pain, dysesthesias, numbness, and weakness. These symptoms usually occur throughout the affected hand or arm without localization to a specific peripheral nerve distribution, and often involve different areas of the entire upper extremity. Extension of symptoms to the shoulder, neck, and upper back is common, and in many patients such symptoms may be perceived as the most functionally disabling. Although symptoms are often limited to one upper extremity, bilateral symptoms are seen; in such cases the dominant extremity is often more symptomatic at first, with the opposite extremity becoming involved over time, perhaps due to compensatory overuse. The aforementioned characteristics allow distinction of nTOS from nerve compression disorders affecting the ulnar nerve at the elbow (cubital compression syndrome), median nerve at the wrist (carpal tunnel syndrome), or other related conditions. Almost all nTOS patients describe reproducible symptom exacerbation by activities requiring elevation and/or sustained use of the arms or hands. Supine positioning and raising arms overhead may elicit symptoms, resulting in pain and difficulty sleeping at night.
Headaches are common in nTOS, most likely due to referred occipital pain from secondary spasm within the trapezius and paraspinous muscles. Although nTOS and migraine headaches often occur together, there is currently no evidence for a specific link between these conditions.
Prolonged severe extrinsic peripheral nerve compression can result in muscle weakness and atrophy, but such findings are rare in nTOS patients, probably due to the intermittent nature of nerve compression. Most commonly, hand or arm pain with affected extremity use may be perceived as weakness, causing avoidance of using the arm or exacerbating positions. This distinction should be clarified to help identify alternative etiologies for these symptoms.
Positional complaints related to nTOS are usually mild, due to transient positional or activity-related brachial plexus irritation. Progressive injury risk is low in these situations, and no specific intervention is warranted. There remains a smaller subset of patients with clinically significant nTOS, however, who exhibit progressively disabling symptoms that effectively prevent them from working or carrying out simple daily activities. These patients often describe a long history of consultations with different physicians and partial or ineffective treatments. It is particularly helpful to obtain a detailed description from the patient of activities that exacerbate symptoms, as well as required workplace activities. This assessment is important to document if restrictions from work are necessary, and for guiding decisions about the role of surgical treatment.
Vascular symptoms, particularly hand discoloration or coldness, should be queried. Ischemia is very unusual in nTOS patients, whereas symptoms of vasomotor disturbance are seen in longstanding or severe nTOS. NTOS symptoms may progress to resemble those of complex regional pain syndrome type I (CRPS-I), with persistent vasospasm, disuse edema, and extreme hypersensitivity leading to avoidance and withdrawal from even light touch of the affected extremity. The CRPS-I diagnosis can be supported by vascular laboratory studies revealing abnormal vasoconstrictive responses (cold-pressor tests) or imaging studies of hand microcirculation, but mostly the diagnosis is made clinically and by response to sympathetic blockade. Identifying this condition in nTOS patients may lead to earlier recommendation for operative treatment and consideration of concomitant cervical sympathectomy.
When history suggests arterial insufficiency or thromboembolism, vascular laboratory studies and contrast-enhanced arteriographic imaging are necessary to exclude the presence of subclavian artery aneurysm or occlusive disease. Conversely, a history of arm swelling, cyanotic discoloration, and distended subcutaneous collaterals may indicate venous TOS due to obstruction of the subclavian vein, which requires contrast venography for full evaluation (see Ch. 126 , Thoracic Outlet Syndrome: Venous).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here