Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chest radiography serves a vital role in the management of critical care patients. Most patients in the intensive care unit (ICU) have at least one and frequently more than one device for central venous access, mechanical ventilation, hemodynamic monitoring, hemodynamic support, pleural drainage, or nutrition. The chest radiograph is an essential tool to assess these devices for proper position, to ensure proper function, and to avoid harm from malpositioned lines and tubes. Prompt recognition and reporting of malpositioning and complications are important to reduce morbidity related to thoracic lines and tubes. This chapter describes the use, proper placement, malpositions, and complications of the more common ICU monitoring and support devices.
Endotracheal intubation is performed in patients who require airway protection, are hypoxemic, or are unable to sustain the work of breathing. The position of the endotracheal tube (ETT) is determined by measuring the distance from the tip of the ETT to the carina. In adult patients, the ideal position of the ETT is 3 to 7 cm from the carina with the neck in the neutral position. On each radiograph, assessment of ETT position is important because the ETT can move with changes in head position and with patient movement. The ETT can move up to 2 cm with changes in head position, and given the average length of the adult trachea is approximately 12 cm from the vocal cords to the carina, this potentially constitutes one third or more of the length of the trachea. In general, the “hose goes with the nose,” meaning the ETT distal tip moves toward the carina with neck flexion and away from the carina with neck extension. Occasionally, on portable chest radiographs, it can be readily seen that the neck is in full flexion with the chin overlying the superior mediastinum. This information can be used to refine the interpretation of ETT position.
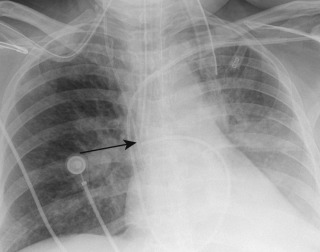
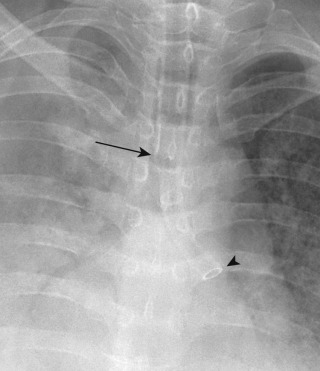
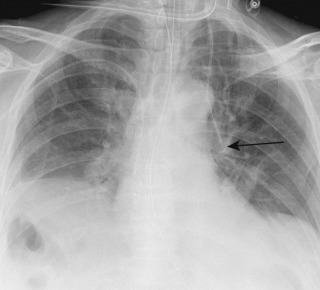
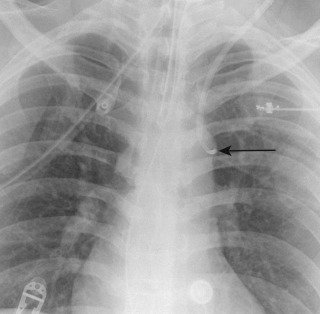
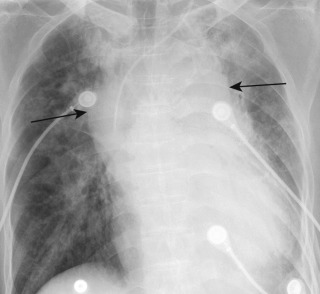
Complications of low ETT placement include bronchial intubation, most often right mainstem intubation because of the more vertical course of the right main bronchus relative to the left ( Fig. 9.1 ). Bronchial intubation may lead to lobar or complete atelectasis of the nonintubated lung. Complications of high ETT placement include risk of extubation, injury to the vocal cords by the ETT cuff balloon, ineffective ventilation, and aspiration ( Fig. 9.2 ). General complications of positive-pressure ventilation include barotrauma such as pneumothorax, pneumomediastinum, subcutaneous emphysema, and pulmonary interstitial emphysema (see Chapter 10 ). Tracheomalacia and tracheal stenosis may occur as delayed complications of endotracheal intubation.
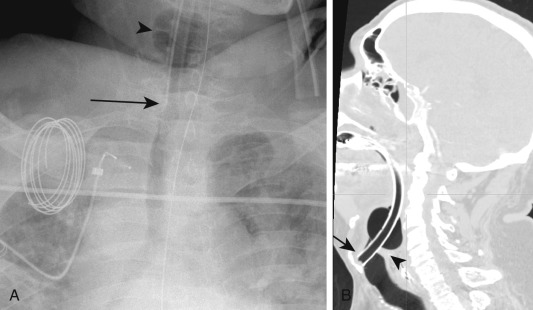
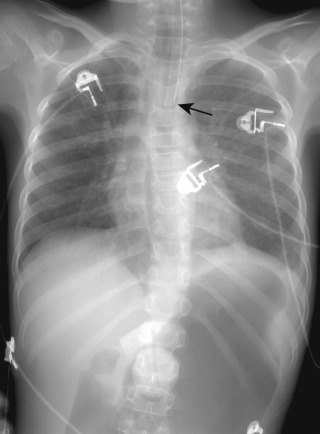
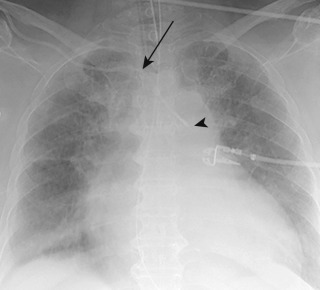
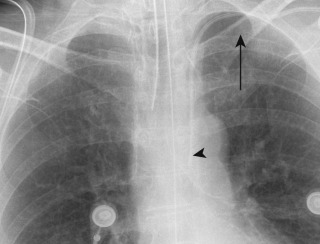
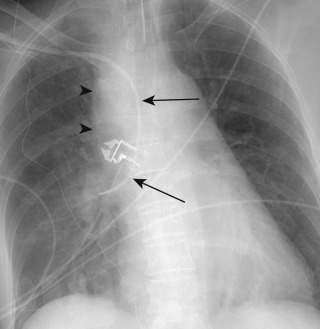
Rare complications of traumatic endotracheal intubation include tracheal perforation, especially of the posterior membranous wall of the trachea. Perforation of the posterior membranous wall can also be associated with esophageal injury and mediastinitis. Rarely, hypopharyngeal perforation and tracheal rupture may occur ( Fig. 9.3 ). Aspiration may occur at the time of intubation or when the ETT balloon cuff is deflated, at which time secretions may be released from above the cuff balloon into the lower airways. Rarely, aspirated foreign bodies such as teeth or dental work may be seen in the airways, esophagus, or stomach, particularly in difficult or traumatic intubations. Esophageal intubation is rare and manifests as an ETT to the left of the trachea rather than overlying the trachea. Air distention of the esophagus and stomach may also be seen due to esophageal insufflation by air ( Fig. 9.4 ). Esophageal intubation can also result in esophageal perforation and manifest with pneumomediastinum. Today, esophageal intubation is rarely seen on postintubation radiographs because it is usually detected by auscultation or capnography, and it is usually corrected before the postintubation radiograph is obtained.

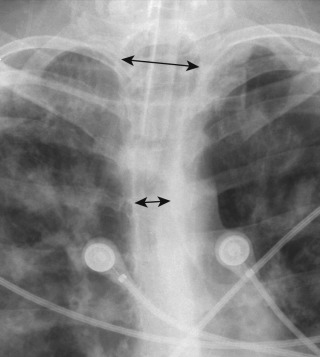
In addition to evaluating the ETT distal tip for proper positioning, it is also important to evaluate the size of the ETT cuff balloon. The ETT cuff balloon should fill the lumen but not distend the tracheal wall. Overdistention of the trachea by the cuff balloon may cause ischemia in the tracheal wall, which could lead to tracheomalacia, tracheal rupture, or tracheal stenosis weeks to months after extubation. It has been reported in the thoracic surgical literature that when the ratio of the diameter of the tracheal cuff balloon to the diameter of the trachea is greater than 1.5, there is an increased risk of tracheal injury ( Fig. 9.5 ).
Occasionally, a double-lumen ETT will be used for mechanical ventilation in cases requiring anatomic lung isolation. Such instances include controlled ventilation of one lung during thoracic surgery, unilateral lung lavage (e.g., alveolar proteinosis), in pulmonary hemorrhage, or in cases of severe infection to avoid spillage to the contralateral lung. For double-lumen ETTs, one lumen is placed in the lower trachea and the other lumen in the right or left main bronchus ( Fig. 9.6 ). One ETT balloon cuff will be present in the trachea above the tracheal lumen orifice, and a second ETT balloon cuff will be in the intubated right or left main bronchus. This isolates the lungs to separate respiratory circuits.
Tracheostomy tubes are placed when patients require long-term mechanical ventilation. Unlike the ETT, the position of a properly secured tracheostomy tube is usually not affected by neck flexion or extension. Thus, a range of accepted distances of the tracheostomy tube distal tip to the carina is not usually used. An appropriately placed tracheostomy tube will be approximately one half to one third the distance from the stoma to the carina. A tracheostomy tube can move out if not properly secured, and this may be visible on chest radiographs. At the time of tracheostomy tube placement, a small amount of pneumomediastinum may be seen. A larger amount of pneumomediastinum at the time of tracheostomy tube placement raises the possibility of a tracheal leak or a tracheal or esophageal injury. Uncommonly, tracheostomy tube placement may result in pneumothorax. After a tracheostomy tube is removed, granulation tissue may result in tracheal stenosis at the cannulation site. Rarely, tracheostomy tubes can perforate the trachea or erode into an adjacent structure such as the innominate artery, leading to massive hemoptysis.
Central venous catheters (CVCs) are commonly used to provide central venous access for intravenous (IV) fluids, medications, nutrition, hemodialysis, and measurement of central venous pressure. There are four broad categories of CVCs: peripherally inserted central catheters (PICCs), temporary (nontunneled) CVCs, permanent (tunneled) CVCs, and implantable ports. The PICC is usually inserted by a forearm vein; the other central catheters are usually inserted via the internal jugular or subclavian vein.
The proper position of the distal tip of a CVC is in the superior vena cava (SVC) or at the junction of the SVC and right atrium (the cava atrial junction). Occasionally, a catheter tip is intentionally positioned in the superior right atrium for improved blood flow, particularly the dialysis catheters. In these cases, right atrial placement should be viewed with caution because of the potential for arrhythmias, cardiac injury, and valvular vegetations if the catheter is placed too low in the right atrium. Precise determination of catheter position on portable chest radiography is often challenging because catheter position is not fixed in location, and the catheter tip can move several centimeters with changes in patient position, arm position, phase of respiration, and radiographic technique.
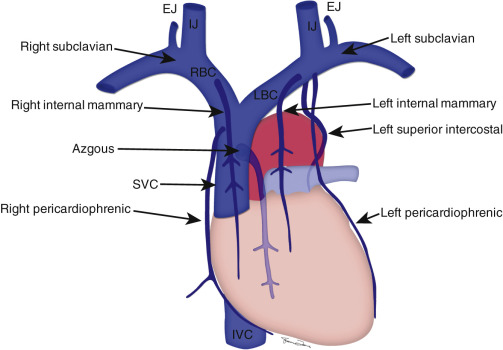
Radiographic assessment of CVC position is important to ensure proper function of the catheter and to avoid catheter-related complications. Radiographs immediately after central line placement show malpositioned CVCs in about 30% of cases. Detection of catheter malposition requires detailed knowledge of the anatomy of the large and small thoracic veins, as well as variants in venous anatomy. Figure 9.7 shows the anatomy of the large central veins, with the line of demarcation between the axillary and subclavian vein at the lateral margin of the first rib. The small thoracic veins depicted in Fig. 9.7 are potential sites for catheter malposition, with the most common malpositions involving the azygous, internal mammary, and left superior intercostal veins.
Radiographic landmarks have been proposed to identify the cranial and caudal aspects of the SVC, although they are controversial and not always anatomically precise. The use of specific anatomic landmarks is often limited by visibility, differences in patient positioning, rotation, and low lung volume technique. In most patients, the right first anterior intercostal space approximates the confluence of the brachiocephalic veins to form the cranial aspect of the SVC. However, a smaller number of patients have a very short SVC with a relatively low confluence of the brachiocephalic veins. For these patients, the right tracheobronchial angle may be a more accurate landmark (with the tracheobronchial angle defined as the junction of the right main bronchus and trachea). The junction of the SVC and right atrium (the cava atrial junction) can be approximated where the lower border of the bronchus intermedius crosses the right heart border. However, this landmark may not be anatomically precise in every case and is not visible on some portable chest radiographs. Although determination of the cranial and caudal aspects of the SVC may be imprecise on chest radiography, a catheter tip between the right tracheobronchial angle and 3 cm below the right tracheobronchial angle is almost always in the SVC.
One of the more common CVC malpositions is a catheter tip in the right atrium ( Fig. 9.8 ). Subclavian catheters and PICCs can extend cephalad into the ipsilateral internal jugular vein. Catheters can also extend across midline and extend peripherally into the contralateral brachiocephalic or subclavian vein. Such catheter malpositions in the larger thoracic veins could lead to catheter malfunction, a less desirable location for infusion of substances requiring high flow, venous thrombosis, and delayed venous stenosis resulting from venous inflammation caused by the catheter tip or substances requiring higher venous flow to avoid venous irritation.
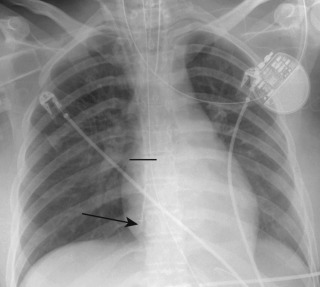
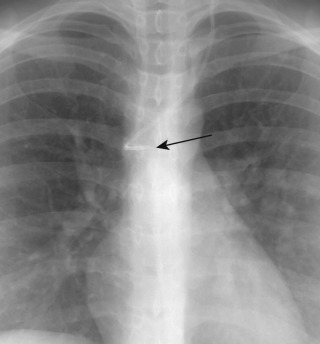
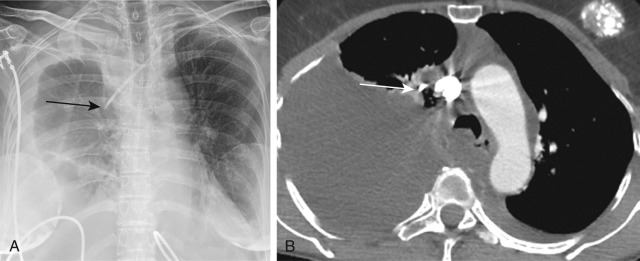
Central venous catheters can also extend into the small thoracic veins, including the azygous, internal mammary, and superior intercostal veins ( Figs. 9.9 to 9.12 ). Catheters in small thoracic veins carry the risk of perforation, thrombosis, ineffective infusion, and ineffective venous blood return. Placement of a CVC in an artery is an urgent finding requiring prompt recognition and communication because of the potential for significant morbidity. Complications include bleeding, air or thrombotic embolus resulting in stroke, and infusion of inappropriate substances directly to the brain (e.g., pressors or total parenteral nutrition). Arterial placement is sometimes but not always clinically suspected because of pulsatile flow through the catheter. Arterial placement is recognized on chest radiography by the course of a catheter that follows the anatomy of major arterial vessels rather than veins ( Figs. 9.13 and 9.14 ).

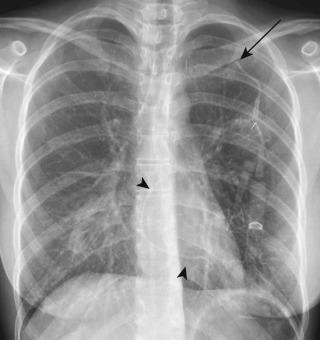
Additional complications of CVC placement may include pneumothorax (up to 6% of lines), mediastinal hematoma, thrombosis, catheter fragmentation, catheter embolus, infection with line sepsis, endocarditis, and septic emboli ( Fig. 9.15 ). An extravascular catheter or perforation of a vessel may manifest by mediastinal widening, development of an apical cap, or increasing pleural effusion caused by hemorrhage or infusion of IV fluid into the mediastinum or pleural space ( Figs. 9.16 and 9.17 ). Left-sided catheters with a distal tip perpendicular and against the lateral wall of the SVC at the confluence of the innominate veins may place the patient at theoretical risk for venous perforation. Catheter narrowing or fragmentation may occur from compression between the first rib and clavicle, which has been termed the pinch-off syndrome ( Fig. 9.18 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here